2011IDSA儿童社区获得性肺炎指南 CAP in Children

I D S A G U I D E L I N E S
The Management
of Community-Acquired Pneumonia in Infants and Children Older Than
3Months
of Age:Clinical Practice Guidelines by
the Pediatric Infectious Diseases Society and the
Infectious Diseases Society of America John S.Bradley,1,a Carrie L.Byington,2,a Samir S.Shah,3,a Brian Alverson,4Edward R.Carter,5Christopher Harrison,6
Sheldon L.Kaplan,7Sharon E.Mace,8George H.McCracken Jr,9Matthew R.Moore,10Shawn D.St Peter,11
Jana A.Stockwell,12and Jack T.Swanson 13
1Department of Pediatrics,University of California San Diego School of Medicine and Rady Children's Hospital of San Diego,San Diego,California;
2Department of Pediatrics,University of Utah School of Medicine,Salt Lake City,Utah;3Departments of Pediatrics,and Biostatistics and Epidemiology,
University of Pennsylvania School of Medicine,and Division of Infectious Diseases,Children's Hospital of Philadelphia,Philadelphia,Pennsylvania;
4Department of Pediatrics,Rhode Island Hospital,Providence,Rhode Island;5Pulmonary Division,Seattle Children's Hospital,Seattle Washington;
6Department of Pediatrics,Children's Mercy Hospital,Kansas City,Missouri;7Department of Pediatrics,Baylor College of Medicine,Houston,Texas;
8Department of Emergency Medicine,Cleveland Clinic,Cleveland,Ohio;9Department of Pediatrics,University of Texas Southwestern,Dallas,Texas;
10Centers for Disease Control and Prevention,Atlanta,Georgia;11Department of Pediatrics,University of Missouri–Kansas City School of Medicine,
Kansas City,Missouri;12Department of Pediatrics,Emory University School of Medicine,Atlanta,Georgia;and 13Department of Pediatrics,McFarland
Clinic,Ames,Iowa
Evidenced-based guidelines for management of infants and children with community-acquired pneumonia
(CAP)were prepared by an expert panel comprising clinicians and investigators representing community
pediatrics,public health,and the pediatric specialties of critical care,emergency medicine,hospital medicine,
infectious diseases,pulmonology,and surgery.These guidelines are intended for use by primary care and
subspecialty providers responsible for the management of otherwise healthy infants and children with CAP in
both outpatient and inpatient settings.Site-of-care management,diagnosis,antimicrobial and adjunctive
surgical therapy,and prevention are discussed.Areas that warrant future investigations are also highlighted.
EXECUTIVE SUMMARY Guidelines for the management of community-acquired pneumonia (CAP)in adults have been demonstrated to decrease morbidity and mortality rates [1,2].These guidelines were created to assist the clinician in the care of a child with CAP.They do not represent the only
approach to diagnosis and therapy;there is considerable
variation among children in the clinical course of pe-
diatric CAP,even with infection caused by the same
pathogen.The goal of these guidelines is to decrease
morbidity and mortality rates for CAP in children by
presenting recommendations for clinical management
that can be applied in individual cases if deemed ap-
propriate by the treating clinician.This document is designed to provide guidance in the
care of otherwise healthy infants and children and ad-
dresses practical questions of diagnosis and management
of CAP evaluated in outpatient (of?ces,urgent care
clinics,emergency departments)or inpatient settings in
the United States.Management of neonates and young
infants through the ?rst 3months,immunocompromised
Received 1July 2011;accepted 8July 2011.
a J.S.B.,C.L.B.,and S.S.S.contributed equally to this work.Correspondence:John S.Bradley,MD,Rady Children's Hospital San Diego/UCSD,3020Children's Way,MC 5041,San Diego,CA 92123(jbradley@https://www.360docs.net/doc/2217285582.html,).
Clinical Infectious Diseases óThe Author 2011.Published by Oxford University Press on behalf of the Infectious Diseases Society of America.All rights reserved.For Permissions,please e-mail:journals.permissions@https://www.360docs.net/doc/2217285582.html,.
1058-4838/2011/537-0024$14.00DOI:10.1093/cid/cir531
Clinical Infectious Diseases Advance Access published August 30, 2011Clinical Infectious Diseases Advance Access published August 31, 2011 at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html, Downloaded from
children,children receiving home mechanical ventilation,and children with chronic conditions or underlying lung disease,such as cystic?brosis,are beyond the scope of these guidelines and are not discussed.
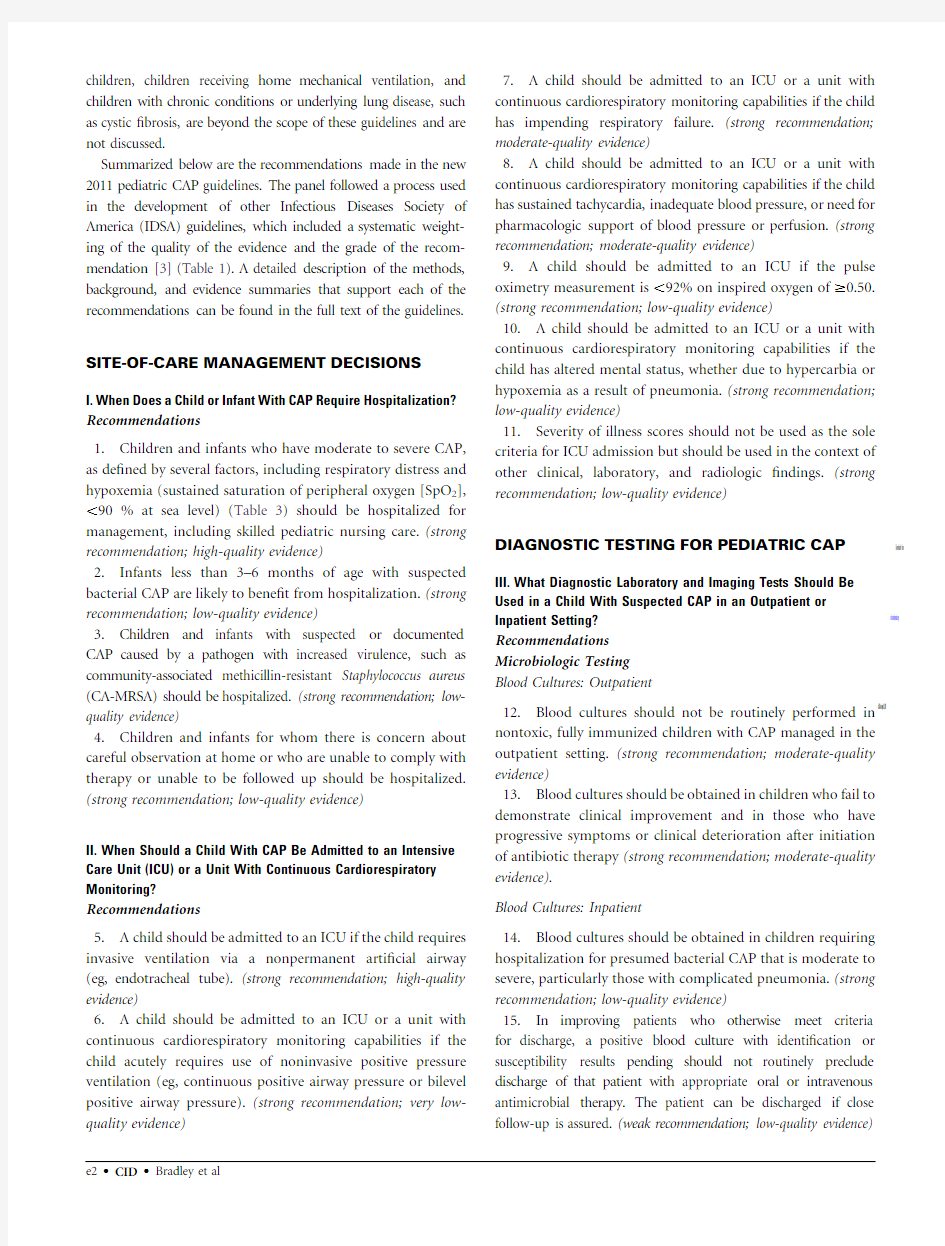
Summarized below are the recommendations made in the new 2011pediatric CAP guidelines.The panel followed a process used in the development of other Infectious Diseases Society of America(IDSA)guidelines,which included a systematic weight-ing of the quality of the evidence and the grade of the recom-mendation[3](Table1).A detailed description of the methods, background,and evidence summaries that support each of the recommendations can be found in the full text of the guidelines.
SITE-OF-CARE MANAGEMENT DECISIONS
I.When Does a Child or Infant With CAP Require Hospitalization? Recommendations
1.Children and infants who have moderate to severe CAP, as de?ned by several factors,including respiratory distress and hypoxemia(sustained saturation of peripheral oxygen[SpO2], ,90%at sea level)(Table3)should be hospitalized for management,including skilled pediatric nursing care.(strong recommendation;high-quality evidence)
2.Infants less than3–6months of age with suspected bacterial CAP are likely to bene?t from hospitalization.(strong recommendation;low-quality evidence)
3.Children and infants with suspected or documented CAP caused by a pathogen with increased virulence,such as community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA)should be hospitalized.(strong recommendation;low-quality evidence)
4.Children and infants for whom there is concern about careful observation at home or who are unable to comply with therapy or unable to be followed up should be hospitalized. (strong recommendation;low-quality evidence)
II.When Should a Child With CAP Be Admitted to an Intensive Care Unit(ICU)or a Unit With Continuous Cardiorespiratory Monitoring?
Recommendations
5.A child should be admitted to an ICU if the child requires invasive ventilation via a nonpermanent arti?cial airway (eg,endotracheal tube).(strong recommendation;high-quality evidence)
6.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child acutely requires use of noninvasive positive pressure ventilation(eg,continuous positive airway pressure or bilevel positive airway pressure).(strong recommendation;very low-quality evidence)
7.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child
has impending respiratory failure.(strong recommendation; moderate-quality evidence)
8.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child
has sustained tachycardia,inadequate blood pressure,or need for pharmacologic support of blood pressure or perfusion.(strong recommendation;moderate-quality evidence)
9.A child should be admitted to an ICU if the pulse oximetry measurement is,92%on inspired oxygen of$0.50. (strong recommendation;low-quality evidence)
10.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the
child has altered mental status,whether due to hypercarbia or hypoxemia as a result of pneumonia.(strong recommendation;
low-quality evidence)
11.Severity of illness scores should not be used as the sole
criteria for ICU admission but should be used in the context of
other clinical,laboratory,and radiologic?ndings.(strong recommendation;low-quality evidence)
DIAGNOSTIC TESTING FOR PEDIATRIC CAP
III.What Diagnostic Laboratory and Imaging Tests Should Be
Used in a Child With Suspected CAP in an Outpatient or
Inpatient Setting?
Recommendations
Microbiologic Testing
Blood Cultures:Outpatient
12.Blood cultures should not be routinely performed in nontoxic,fully immunized children with CAP managed in the outpatient setting.(strong recommendation;moderate-quality evidence)
13.Blood cultures should be obtained in children who fail to demonstrate clinical improvement and in those who have progressive symptoms or clinical deterioration after initiation
of antibiotic therapy(strong recommendation;moderate-quality evidence).
Blood Cultures:Inpatient
14.Blood cultures should be obtained in children requiring hospitalization for presumed bacterial CAP that is moderate to severe,particularly those with complicated pneumonia.(strong recommendation;low-quality evidence)
15.In improving patients who otherwise meet criteria
for discharge,a positive blood culture with identi?cation or susceptibility results pending should not routinely preclude discharge of that patient with appropriate oral or intravenous antimicrobial therapy.The patient can be discharged if close
follow-up is assured.(weak recommendation;low-quality evidence)
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
Table1.Strength of Recommendations and Quality of Evidence
Strength of recommendation and quality of evidence
Clarity of balance between
desirable and undesirable effects
Methodologic quality of supporting
evidence(examples)Implications
Strong recommendation
High-quality evidence Desirable effects clearly
outweigh undesirable effects,
or vice versa Consistent evidence from well-
performed RCTs a or exceptionally
strong evidence from unbiased
observational studies
Recommendation can apply to
most patients in most
circumstances;further
research is unlikely to change
our con?dence in the
estimate of effect.
Moderate-quality evidence Desirable effects clearly
outweigh undesirable effects,
or vice versa Evidence from RCTs with important
limitations(inconsistent results,
methodologic?aws,indirect,or
imprecise)or exceptionally strong
evidence from unbiased
observational studies
Recommendation can apply to
most patients in most
circumstances;further
research(if performed)is
likely to have an important
impact on our con?dence in
the estimate of effect and
may change the estimate.
Low-quality evidence Desirable effects clearly
outweigh undesirable effects,
or vice versa Evidence for$1critical outcome
from observational studies,RCTs
with serious?aws or indirect
evidence
Recommendation may change
when higher quality evidence
becomes available;further
research(if performed)is
likely to have an important
impact on our con?dence in
the estimate of effect and is
likely to change the estimate.
Very low-quality evidence (rarely applicable)Desirable effects clearly
outweigh undesirable effects,
or vice versa
Evidence for$1critical outcome
from unsystematic clinical
observations or very indirect
evidence
Recommendation may change
when higher quality evidence
becomes available;any
estimate of effect for$1
critical outcome is very
uncertain.
Weak recommendation
High-quality evidence Desirable effects closely
balanced with undesirable
effects Consistent evidence from well-
performed RCTs or exceptionally
strong evidence from unbiased
observational studies
The best action may differ
depending on circumstances
or patients or societal values;
further research is unlikely to
change our con?dence in the
estimate of effect.
Moderate-quality evidence Desirable effects closely
balanced with undesirable
effects Evidence from RCTs with important
limitations(inconsistent results,
methodologic?aws,indirect,or
imprecise)or exceptionally strong
evidence from unbiased
observational studies
Alternative approaches are likely
to be better for some patients
under some circumstances;
further research(if performed)
is likely to have an important
impact on our con?dence in
the estimate of effect and
may change the estimate.
Low-quality evidence Uncertainty in the estimates of
desirable effects,harms,and
burden;desirable effects,
harms,and burden may be
closely balanced Evidence for$1critical outcome
from observational studies,from
RCTs with serious?aws or indirect
evidence
Other alternatives may be equally
reasonable;further research is
very likely to have an important
impact on our con?dence in the
estimate of effect and is likely
to change the estimate.
Very low-quality evidence Major uncertainty in estimates
of desirable effects,harms,
and burden;desirable effects
may or may not be balanced
with undesirable effects
may be closely balanced Evidence for$1critical outcome from
unsystematic clinical observations or
2very indirect evidence
Other alternatives may be equally
reasonable;any estimate of
effect,for at$1critical
outcome,is very uncertain.
a RCTs,randomized controlled trials. at IDSA on August 31, 2011 https://www.360docs.net/doc/2217285582.html, Downloaded from
Follow-up Blood Cultures 16.Repeated blood cultures in children with clear clinical improvement are not necessary to document resolution of pneumococcal bacteremia.(weak recommendation;low-quality evidence)17.Repeated blood cultures to document resolution of bacteremia should be obtained in children with bacteremia
caused by S.aureus ,regardless of clinical status.(strong recommendation;low-quality evidence)Sputum Gram Stain and Culture 18.Sputum samples for culture and Gram stain should be obtained in hospitalized children who can produce sputum.(weak recommendation;low-quality evidence)Urinary Antigen Detection Tests
19.Urinary antigen detection tests are not recommended for the diagnosis of pneumococcal pneumonia in children;false-positive tests are common.(strong recommendation;high-quality evidence)
Testing For Viral Pathogens
20.Sensitive and speci?c tests for the rapid diagnosis of in?uenza virus and other respiratory viruses should be used in the evaluation of children with CAP.A positive in?uenza test may decrease both the need for additional diagnostic studies and antibiotic use,while guiding appropriate use of antiviral agents in both outpatient and inpatient settings.(strong
recommendation;high-quality evidence)
21.Antibacterial therapy is not necessary for children,either outpatients or inpatients,with a positive test for in?uenza virus in the absence of clinical,laboratory,or radiographic ?ndings that suggest bacterial coinfection.(strong recommendation;
high-quality evidence).
22.Testing for respiratory viruses other than in?uenza virus
can modify clinical decision making in children with suspected
pneumonia,because antibacterial therapy will not routinely be required for these children in the absence of clinical,laboratory,or radiographic ?ndings that suggest bacterial coinfection.(weak recommendation;low-quality evidence)
Testing for Atypical Bacteria 23.Children with signs and symptoms suspicious for Mycoplasma pneumoniae should be tested to help guide
antibiotic selection.(weak recommendation;moderate-quality
evidence)
24.Diagnostic testing for Chlamydophila pneumoniae is not recommended as reliable and readily available diagnostic tests do not currently exist.(strong recommendation;high-quality
evidence)
Ancillary Diagnostic Testing
Complete Blood Cell Count
25.Routine measurement of the complete blood cell count is
not necessary in all children with suspected CAP managed in the
outpatient setting,but in those with more serious disease it may provide useful information for clinical management in the context of the clinical examination and other laboratory and imaging studies.(weak recommendation;low-quality evidence)
26.A complete blood cell count should be obtained for
patients with severe pneumonia,to be interpreted in the context
of the clinical examination and other laboratory and imaging
studies.(weak recommendation;low-quality evidence)
Acute-Phase Reactants
27.Acute-phase reactants,such as the erythrocyte sedimentation rate (ESR),C-reactive protein (CRP)concentration,or serum Table 3.Criteria for Respiratory Distress in Children With Pneumonia Signs of Respiratory Distress 1.Tachypnea,respiratory rate,breaths/min a Age 0–2months:.60Age 2–12months:.50Age 1–5Years:.40Age .5Years:.202.Dyspnea 3.Retractions (suprasternal,intercostals,or subcostal)4.Grunting 5.Nasal ?aring 6.Apnea
7.Altered mental status 8.Pulse oximetry measurement ,90%on room air a Adapted from World Health Organization criteria.Table https://www.360docs.net/doc/2217285582.html,plications Associated With Community-Acquired Pneumonia Pulmonary Pleural effusion or empyema Pneumothorax Lung abscess
Bronchopleural ?stula Necrotizing pneumonia Acute respiratory failure Metastatic Meningitis Central nervous system abscess Pericarditis
Endocarditis Osteomyelitis Septic arthritis Systemic Systemic in?ammatory response syndrome or sepsis Hemolytic uremic syndrome at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html, Downloaded from
procalcitonin concentration,cannot be used as the sole determinant to distinguish between viral and bacterial causes of CAP.(strong recommendation;high-quality evidence)
28.Acute-phase reactants need not be routinely measured in fully immunized children with CAP who are managed as outpatients,although for more serious disease, acute-phase reactants may provide useful information for clinical management.(strong recommendation;low-quality evidence)
29.In patients with more serious disease,such as those requiring hospitalization or those with pneumonia-associated complications,acute-phase reactants may be used in conjunction with clinical?ndings to assess response to therapy.(weak recommendation;low-quality evidence)
Pulse Oximetry
30.Pulse oximetry should be performed in all children with pneumonia and suspected hypoxemia.The presence of hypoxemia should guide decisions regarding site of care and further diagnostic testing.(strong recommendation;moderate-quality evidence)
Chest Radiography
Initial Chest Radiographs:Outpatient
31.Routine chest radiographs are not necessary for the con?rmation of suspected CAP in patients well enough to be treated in the outpatient setting(after evaluation in the of?ce,clinic,or emergency department setting).(strong recommendation;high-quality evidence)
32.Chest radiographs,posteroanterior and lateral,should be obtained in patients with suspected or documented hypoxemia or signi?cant respiratory distress(Table3)and in those with failed initial antibiotic therapy to verify the presence or absence of complications of pneumonia,including parapneumonic effusions,necrotizing pneumonia,and pneumothorax.(strong recommendation;moderate-quality evidence)
Initial Chest Radiographs:Inpatient
33.Chest radiographs(posteroanterior and lateral)should be obtained in all patients hospitalized for management of CAP to document the presence,size,and character of parenchymal in?ltrates and identify complications of pneumonia that may lead to interventions beyond antimicrobial agents and supportive medical therapy.(strong recommendation;moderate-quality evidence)
Follow-up Chest Radiograph
34.Repeated chest radiographs are not routinely required in children who recover uneventfully from an episode of CAP. (strong recommendation;moderate-quality evidence)
35.Repeated chest radiographs should be obtained in children who fail to demonstrate clinical improvement and
in those who have progressive symptoms or clinical deterioration within48–72hours after initiation of antibiotic therapy.(strong recommendation;moderate-quality evidence)
36.Routine daily chest radiography is not recommended
in children with pneumonia complicated by parapneumonic effusion after chest tube placement or after video-assisted thoracoscopic surgery(VATS),if they remain clinically stable.(strong recommendation;low-quality evidence)
37.Follow-up chest radiographs should be obtained in patients with complicated pneumonia with worsening respiratory distress or clinical instability,or in those with persistent fever that is not responding to therapy over48-72 hours.(strong recommendation;low-quality evidence)
38.Repeated chest radiographs4–6weeks after the diagnosis of CAP should be obtained in patients with recurrent pneumonia involving the same lobe and in patients with lobar collapse at initial chest radiography
with suspicion of an anatomic anomaly,chest mass,or
Table4.Criteria for CAP Severity of Illness in Children with Community-Acquired Pneumonia
Criteria
Major criteria
Invasive mechanical ventilation
Fluid refractory shock
Acute need for NIPPV
Hypoxemia requiring FiO2greater than inspired concentration or
?ow feasible in general care area
Minor criteria
Respiratory rate higher than WHO classi?cation for age
Apnea
Increased work of breathing(eg,retractions,dyspnea,nasal?aring,
grunting)
PaO2/FiO2ratio,250
Multilobar in?ltrates
PEWS score.6
Altered mental status
Hypotension
Presence of effusion
Comorbid conditions(eg,HgbSS,immunosuppression,
immunode?ciency)
Unexplained metabolic acidosis
Modi?ed from Infectious Diseases Society of America/American Thoracic
Society consensus guidelines on the management of community-acquired pneumonia in adults[27,table4].Clinician should consider care in an intensive
care unit or a unit with continuous cardiorespiratory monitoring for the child
having$1major or$2minor criteria.
Abbreviations:FiO2,fraction of inspired oxygen;HgbSS,Hemoglobin SS
disease;NIPPV,noninvasive positive pressure ventilation;PaO2,arterial
oxygen pressure;PEWS,Pediatric Early Warning Score[70].
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
foreign body aspiration.(strong recommendation;moderate-quality evidence)
IV.What Additional Diagnostic Tests Should Be Used in a Child With Severe or Life-Threatening CAP?
Recommendations
39.The clinician should obtain tracheal aspirates for Gram stain and culture,as well as clinically and epidemiologically guided testing for viral pathogens,including in?uenza virus,at the time of initial endotracheal tube placement in children requiring mechanical ventilation.(strong recommendation;low-quality evidence)
40.Bronchoscopic or blind protected specimen brush sampling,bronchoalveolar lavage(BAL),percutaneous lung aspiration,or open lung biopsy should be reserved for the immunocompetent child with severe CAP if initial diagnostic tests are not positive.(weak recommendation;low-quality evidence)
ANTI-INFECTIVE TREATMENT
V.Which Anti-Infective Therapy Should Be Provided to a Child With Suspected CAP in Both Outpatient and Inpatient Settings? Recommendations
Outpatients
41.Antimicrobial therapy is not routinely required for preschool-aged children with CAP,because viral pathogens are responsible for the great majority of clinical disease.(strong recommendation;high-quality evidence)
42.Amoxicillin should be used as?rst-line therapy for previously healthy,appropriately immunized infants and preschool children with mild to moderate CAP suspected to be of bacterial origin.Amoxicillin provides appropriate coverage for Streptococcus pneumoniae,the most prominent invasive bacterial pathogen.Table5lists preferred agents and alternative agents for children allergic to amoxicillin(strong recommendation;moderate-quality evidence)
43.Amoxicillin should be used as?rst-line therapy for previously healthy appropriately immunized school-aged children and adolescents with mild to moderate CAP for S.pneumoniae,the most prominent invasive bacterial pathogen.Atypical bacterial pathogens(eg,M.pneumoniae), and less common lower respiratory tract bacterial pathogens,as discussed in the Evidence Summary,should also be considered in management decisions.(strong recommendation;moderate-quality evidence)
44.Macrolide antibiotics should be prescribed for treatment of children(primarily school-aged children and adolescents) evaluated in an outpatient setting with?ndings compatible with CAP caused by atypical https://www.360docs.net/doc/2217285582.html,boratory testing for M.pneumoniae should be performed if available in a clinically relevant time frame.Table5lists preferred and alternative agents
for atypical pathogens.(weak recommendation;moderate-quality evidence)
45.In?uenza antiviral therapy(Table6)should be administered as soon as possible to children with moderate
to severe CAP consistent with in?uenza virus infection during widespread local circulation of in?uenza viruses,particularly
for those with clinically worsening disease documented at the
time of an outpatient visit.Because early antiviral treatment has
been shown to provide maximal bene?t,treatment should not be delayed until con?rmation of positive in?uenza test results. Negative results of in?uenza diagnostic tests,especially rapid antigen tests,do not conclusively exclude in?uenza disease. Treatment after48hours of symptomatic infection may still provide clinical bene?t to those with more severe disease.(strong recommendation;moderate-quality evidence)
Inpatients
46.Ampicillin or penicillin G should be administered to the
fully immunized infant or school-aged child admitted to
a hospital ward with CAP when local epidemiologic data document lack of substantial high-level penicillin resistance for invasive S.pneumoniae.Other antimicrobial agents for empiric therapy are provided in Table7.(strong recommendation; moderate-quality evidence)
47.Empiric therapy with a third-generation parenteral cephalosporin(ceftriaxone or cefotaxime)should be prescribed for hospitalized infants and children who are
not fully immunized,in regions where local epidemiology of invasive pneumococcal strains documents high-level penicillin resistance,or for infants and children with life-threatening infection,including those with empyema (Table7).Non–b-lactam agents,such as vancomycin,have
not been shown to be more effective than third-generation cephalosporins in the treatment of pneumococcal pneumonia for the degree of resistance noted currently in
North America.(weak recommendation;moderate-quality evidence)
48.Empiric combination therapy with a macrolide(oral or parenteral),in addition to a b-lactam antibiotic,should be prescribed for the hospitalized child for whom M.pneumoniae
and C.pneumoniae are signi?cant considerations;diagnostic
testing should be performed if available in a clinically relevant
time frame(Table7).(weak recommendation;moderate-quality evidence)
49.Vancomycin or clindamycin(based on local susceptibility
data)should be provided in addition to b-lactam therapy if clinical,laboratory,or imaging characteristics are consistent
with infection caused by S.aureus(Table7).(strong recommendation;low-quality evidence)
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
Table5.Selection of Antimicrobial Therapy for Specific Pathogens
Pathogen Parenteral therapy Oral therapy(step-down therapy or mild infection)
Streptococcus pneumoniae with MICs for penicillin#2.0l g/mL Preferred:ampicillin(150–200mg/kg/day every
6hours)or penicillin(200000–250000U/kg/day
every4–6h);
Alternatives:ceftriaxone
(50–100mg/kg/day every12–24hours)(preferred
for parenteral outpatient therapy)or cefotaxime
(150mg/kg/day every8hours);may also be
effective:clindamycin(40mg/kg/day every
6–8hours)or vancomycin(40–60mg/kg/day every
6–8hours)
Preferred:amoxicillin(90mg/kg/day in
2doses or45mg/kg/day in3doses);
Alternatives:second-or third-generation
cephalosporin(cefpodoxime,cefuroxime,
cefprozil);oral levo?oxacin,if susceptible
(16–20mg/kg/day in2doses for children
6months to5years old and8–10mg/kg/day
once daily for children5to16years old;
maximum daily dose,750mg)or oral
linezolid(30mg/kg/day in3doses for
children,12years old and20mg/kg/day
in2doses for children$12years old)
S.pneumoniae resistant to penicillin,with MICs $4.0l g/mL Preferred:ceftriaxone(100mg/kg/day every
12–24hours);
Alternatives:ampicillin
(300–400mg/kg/day every6hours),levo?oxacin
(16–20mg/kg/day every12hours for children
6months to5years old and8–10mg/kg/day
once daily for children5–16years old;maximum
daily dose,750mg),or linezolid(30mg/kg/day
every8hours for children,12years old and
20mg/kg/day every12hours for children$12years
old);may also be effective:clindamycin a
(40mg/kg/day every6–8hours)or vancomycin
(40–60mg/kg/day every6–8hours)
Preferred:oral levo?oxacin(16–20mg/kg/day
in2doses for children6months to5years
and8–10mg/kg/day once daily for children
5–16years,maximum daily dose,750mg),
if susceptible,or oral linezolid(30mg/kg/day
in3doses for children,12years and
20mg/kg/day in2doses for children
$12years);
Alternative:oral clindamycin a
(30–40mg/kg/day in3doses)
Group A Streptococcus Preferred:intravenous penicillin(100000–250000
U/kg/day every4–6hours)or ampicillin
(200mg/kg/day every6hours);
Alternatives:ceftriaxone(50–100mg/kg/day every
12–24hours)or cefotaxime(150mg/kg/day every
8hours);may also be effective:clindamycin,if
susceptible(40mg/kg/day every6–8hours)or
vancomycin b(40–60mg/kg/day every6–8hours)Preferred:amoxicillin(50–75mg/kg/day in
2doses),or penicillin V(50–75mg/kg/day in 3or4doses);
Alternative:oral clindamycin a
(40mg/kg/day in3doses)
Stapyhylococcus aureus, methicillin susceptible (combination therapy not well studied)Preferred:cefazolin(150mg/kg/day every8hours)or
semisynthetic penicillin,eg oxacillin
(150–200mg/kg/day every6–8hours);
Alternatives:clindamycin a(40mg/kg/day every
6–8hours)or>vancomycin(40–60mg/kg/day
every6–8hours)
Preferred:oral cephalexin(75–100mg/kg/day
in3or4doses);
Alternative:oral clindamycin a
(30–40mg/kg/day in3or4doses)
S.aureus,methicillin resistant, susceptible to clindamycin (combination therapy not well-studied)Preferred:vancomycin(40–60mg/kg/day every
6–8hours or dosing to achieve an AUC/MIC ratio of
.400)or clindamycin(40mg/kg/day every6–8hours);
Alternatives:linezolid(30mg/kg/day every8hours
for children,12years old and20mg/kg/day every
12hours for children$12years old)
Preferred:oral clindamycin(30–40mg/kg/day
in3or4doses);
Alternatives:oral linezolid
(30mg/kg/day in3doses for children
,12years and20mg/kg/day in2doses
for children$12years)
S.aureus,methicillin resistant, resistant to clindamycin (combination therapy not well studied)Preferred:vancomycin(40–60mg/kg/day every
6-8hours or dosing to achieve an AUC/MIC ratio of
.400);
Alternatives:linezolid(30mg/kg/day every
8hours for children,12years old and20mg/kg/day
every12hours for children$12years old)
Preferred:oral linezolid(30mg/kg/day in
3doses for children,12years and
20mg/kg/day in2doses for children
$12years old);
Alternatives:none;entire treatment course with
parenteral therapy may be required
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
VI.How Can Resistance to Antimicrobials Be Minimized?Recommendations 50.Antibiotic exposure selects for antibiotic resistance;therefore,limiting exposure to any antibiotic,whenever possible,is preferred.(strong recommendation;moderate-quality evidence)51.Limiting the spectrum of activity of antimicrobials to that speci?cally required to treat the identi?ed pathogen is preferred.(strong recommendation;low-quality evidence)https://www.360docs.net/doc/2217285582.html,ing the proper dosage of antimicrobial to be able to achieve a minimal effective concentration at the site of infection is important to decrease the development of resistance.(strong
recommendation;low-quality evidence)53.Treatment for the shortest effective duration will minimize exposure of both pathogens and normal microbiota to antimicrobials and minimize the selection for resistance.(strong recommendation;low-quality evidence)VII.What Is the Appropriate Duration of Antimicrobial Therapy for CAP?
Recommendations
54.Treatment courses of 10days have been best studied,although shorter courses may be just as effective,particularly for more mild disease managed on an outpatient basis.(strong
recommendation;moderate-quality evidence)
55.Infections caused by certain pathogens,notably CA-MRSA,may require longer treatment than those caused by
S.pneumoniae .(strong recommendation;moderate-quality evidence)
VIII.How Should the Clinician Follow the Child With CAP for the
Expected Response to Therapy?
Recommendation
56.Children on adequate therapy should demonstrate clinical and laboratory signs of improvement within 48–72hours.For Table 5.(Continued )
Pathogen Parenteral therapy Oral therapy (step-down therapy
or mild infection)
Haemophilus in?uenza,typeable (A-F)or nontypeable Preferred:intravenous ampicillin (150-200mg/kg/day every 6hours)if b -lactamase negative,ceftriaxone (50–100mg/kg/day every 12-24hours)if b -lactamase producing,or cefotaxime (150mg/kg/day every 8hours);Alternatives:intravenous cipro?oxacin (30mg/kg/day
every 12hours)or intravenous levo?oxacin (16-20mg/kg/day every 12hours for children 6months to 5years old
and 8-10mg/kg/day once daily for children 5to
16years old;maximum daily dose,750mg)
Preferred:amoxicillin (75-100mg/kg/day in 3doses)if b -lactamase negative)or
amoxicillin clavulanate (amoxicillin
component,45mg/kg/day in 3doses or
90mg/kg/day in 2doses)if b -lactamase
producing;
Alternatives:cefdinir,ce?xime,
cefpodoxime,or ceftibuten
Mycoplasma pneumoniae Preferred:intravenous azithromycin (10mg/kg on days 1and 2of therapy;transition to oral therapy if possible);Alternatives:intravenous erythromycin lactobionate (20mg/kg/day every 6hours)or levo?oxacin (16-20mg/kg/day every 12hours;maximum daily dose,750mg)Preferred:azithromycin (10mg/kg on day 1,
followed by 5mg/kg/day once daily on
days 2–5);
Alternatives:clarithromycin
(15mg/kg/day in 2doses)or oral
erythromycin (40mg/kg/day in 4doses);
for children .7years old,doxycycline
(2–4mg/kg/day in 2doses;for adolescents
with skeletal maturity,levo?oxacin
(500mg once daily)or moxi?oxacin
(400mg once daily)
Chlamydia trachomatis or Chlamydophila pneumoniae Preferred:intravenous azithromycin (10mg/kg on days 1and 2of therapy;transition to oral therapy if possible);Alternatives:intravenous erythromycin lactobionate (20mg/kg/day every 6hours)or levo?oxacin (16-20mg/kg/day in 2doses for children 6months to 5years old and 8-10mg/kg/day once daily for children 5to 16years old;maximum daily dose,750mg)Preferred:azithromycin (10mg/kg on day 1,followed by 5mg/kg/day once daily
days 2–5);
Alternatives:clarithromycin
(15mg/kg/day in 2doses)or oral
erythromycin (40mg/kg/day in 4doses);
for children .7years old,doxycycline
(2-4mg/kg/day in 2doses);for adolescents
with skeletal maturity,levo?oxacin
(500mg once daily)or moxi?oxacin
(400mg once daily)
Doses for oral therapy should not exceed adult doses.
Abbreviations:AUC,area under the time vs.serum concentration curve;MIC,minimum inhibitory concentration.
a Clindamycin resistance appears to be increasing in certain geographic areas among S.pneumoniae and S.aureus infections.
b For b -lactam–allergi
c children.
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html, Downloaded from
children whose condition deteriorates after admission and initiation of antimicrobial therapy or who show no improvement within48–72hours,further investigation should be performed.(strong recommendation;moderate-quality evidence)
ADJUNCTIVE SURGICAL AND NON–
ANTI-INFECTIVE THERAPY FOR PEDIATRIC CAP
IX.How Should a Parapneumonic Effusion Be Identified? Recommendation
57.History and physical examination may be suggestive of parapneumonic effusion in children suspected of having CAP,but chest radiography should be used to con?rm the presence of pleural?uid.If the chest radiograph is not conclusive,then further imaging with chest ultrasound or computed tomography(CT)is recommended.(strong recommendation; high-quality evidence)
X.What Factors Are Important in Determining Whether Drainage of the Parapneumonic Effusion Is Required? Recommendations
58.The size of the effusion is an important factor that determines management(Table8,Figure1).(strong recommendation;moderate-quality evidence)
Table6.Influenza Antiviral Therapy
Drug[186187]Formulation
Dosing recommendations
Treatment Prophylaxis a
Children Adults Children Adults
Oseltamivir (Tami?u)75-mg capsule;
60mg/5mL
Suspension
$24months old:
4mg/kg/day in
2doses,for a
5-day treatment
course
150mg/day in
2doses for
5days
#15kg:30mg/day;.15to
23kg:45mg/day;.23to
40kg:60mg/day;.40kg:
75mg/day(once daily in
each group)
75mg/day
once daily
#15kg:60mg/day;
.15to23kg:90mg/day;
.23to40kg:120mg/day;
.40kg:150mg/day
(divided into2doses
for each group)
9–23months old:
7mg/kg/day in
2doses;0–8months
old:6mg/kg/day in
2doses;premature
infants:2mg/kg/day
in2doses
9–23months old:3.5mg/kg
once daily;3–8months old:
3mg/kg once daily;not
routinely recommended for
infants,3months old
owing to limited data in
this age group
Zanamivir (Relenza)5mg per inhalation,
using a Diskhaler
$7years old:2inhalations
(10mg total per dose),
twice daily for5days
2inhalations
(10mg total per
dose),twice daily
for5days
$5years old:2inhalations
(10mg total per dose),
once daily for10days
2inhalations
(10mg total
per dose),
once daily
for10days
Amantadine (Symmetrel)b 100-mg tablet;
50mg/5mL
suspension
1–9years old:5–8mg/kg/day
as single daily dose or in
2doses,not to exceed
150mg/day;9–12years old:
200mg/day in2doses(not
studied as single daily dose)
200mg/day,as
single daily dose
or in2doses
1–9years old:
same as
treatment dose;
9–12years old:
same as
treatment dose
Same as
treatment
dose
Rimantadine (Flumadine)b 100-mg tablet;
50mg/5mL
suspension
Not FDA approved for
treatment in children,but
published data exist on safety
and ef?cacy in children;
suspension:1–9years old:
6.6mg/kg/day
(maximum150mg/kg/day)in
2doses;$10years old:
200mg/day,as single daily
dose or in2doses
200mg/day,either
as a single daily
dose,or divided
into2doses
FDA approved for
prophylaxis down to
12months of age.
1–9years old:
5mg/kg/day
once daily,not to exceed
150mg;$10years old:
200mg/day as single daily
dose or in2doses
200mg/day,
as single
daily dose
or in
2doses
NOTE.Check Centers for Disease Control and Prevention Website(http://www.?https://www.360docs.net/doc/2217285582.html,/)for current susceptibility data.
a In children for whom prophylaxis is indicated,antiviral drugs should be continued for the duration of known in?uenza activity in the community because of the potential for repeated and unknown exposures or until immunity can be achieved after immunization.
b Amantadine and rimantadine should be used for treatment and prophylaxis only in winter seasons during which a majority of in?uenza A virus strains isolated are adamantine susceptible;the adamantanes should not be used for primary therapy because of the rapid emergence of resistance.However,for patients requiring adamantane therapy,a treatment course of 7days is suggested,or until24–48hours after the disappearance of signs and symptoms. at IDSA on August 31, 2011 https://www.360docs.net/doc/2217285582.html, Downloaded from
Table7.Empiric Therapy for Pediatric Community-Acquired Pneumonia(CAP)
Empiric therapy
Site of care Presumed bacterial
pneumonia
Presumed atypical
pneumonia
Presumed in?uenza
pneumonia a
Outpatient
,5years old(preschool)Amoxicillin,oral(90mg/kg/day
in2doses b)
Alternative:
oral amoxicillin clavulanate
(amoxicillin component,
90mg/kg/day in2doses b)Azithromycin oral(10mg/kg on
day1,followed by5mg/kg/day
once daily on days2–5);
Alternatives:oral clarithromycin
(15mg/kg/day in2doses
for7-14days)or oral
erythromycin(40mg/kg/day
in4doses)
Oseltamivir
$5years old Oral amoxicillin(90mg/kg/day in
2doses b to a maximum
of4g/day c);for children
with presumed bacterial
CAP who do not have clinical,
laboratory,or radiographic
evidence that distinguishes
bacterial CAP from
atypical CAP,a macrolide
can be added to a b-lactam
antibiotic for empiric therapy;
alternative:oral amoxicillin
clavulanate(amoxicillin
component,90mg/kg/day
in2doses b to a maximum
dose of4000mg/day,
eg,one2000-mg tablet
twice daily b)Oral azithromycin(10mg/kg on
day1,followed by5mg/kg/day
once daily on days2–5to a
maximum of500mg on day1,
followed by250mg on days2–5);
alternatives:oral clarithromycin
(15mg/kg/day in2doses to a
maximum of1g/day);
erythromycin,doxycycline for
children.7years old
Oseltamivir or zanamivir
(for children7years
and older);alternatives:
peramivir,oseltamivir
and zanamivir
(all intravenous)are
under clinical
investigation in children;
intravenous zanamivir
available for
compassionate use
Inpatient(all ages)d
Fully immunized with conjugate vaccines for Haemophilus in?uenzae type b and Streptococcus pneumoniae;local penicillin resistance in invasive strains of pneumococcus is minimal Ampicillin or penicillin G;
alternatives:
ceftriaxone or cefotaxime;
addition of vancomycin or
clindamycin for
suspected CA-MRSA
Azithromycin(in addition to
b-lactam,if diagnosis of
atypical pneumonia is in
doubt);alternatives:
clarithromycin or
erythromycin;
doxycycline for children
.7years old;levo?oxacin
for children who have
reached growth maturity,
or who cannot tolerate
macrolides
Oseltamivir or zanamivir
(for children$7years old;
alternatives:peramivir,
oseltamivir and
zanamivir(all intravenous)
are under clinical
investigation
in children;intravenous
zanamivir available for
compassionate use
Not fully immunized for H, in?uenzae type b and
S.pneumoniae;local penicillin resistance in invasive strains of pneumococcus is
signi?cant Ceftriaxone or cefotaxime;addition of
vancomycin or clindamycin for
suspected CA-MRSA;alternative:
levo?oxacin;addition of vancomycin
or clindamycin for suspected
CA-MRSA
Azithromycin(in addition to
b-lactam,if diagnosis in
doubt);alternatives:
clarithromycin or erythromycin;
doxycycline for children.7years
old;levo?oxacin for children
who have reached growth
maturity or who cannot
tolerate macrolides
As above
For children with drug allergy to recommended therapy,see Evidence Summary for Section V.Anti-Infective Therapy.For children with a history of possible, nonserious allergic reactions to amoxicillin,treatment is not well de?ned and should be individualized.Options include a trial of amoxicillin under medical observation;a trial of an oral cephalosporin that has substantial activity against S.pneumoniae,such as cefpodoxime,cefprozil,or cefuroxime,provided under medical supervision;treatment with levo?oxacin;treatment with linezolid;treatment with clindamycin(if susceptible);or treatment with a macrolide(if susceptible). For children with bacteremic pneumococcal pneumonia,particular caution should be exercised in selecting alternatives to amoxicillin,given the potential for secondary sites of infection,including meningitis.
Abbreviation:CA-MRSA,community-associated methicillin-resistant Staphylococcus aureus.
a See Table6for dosages.
b See text for discussion of dosage recommendations based on local susceptibility data.Twice daily dosing of amoxicillin or amoxicillin clavulanate may be effective for pneumococci that are susceptible to penicillin.
c Not evaluate
d prospectively for safety.
d Se
e Table5for dosages. at IDSA on August 31, 2011 https://www.360docs.net/doc/2217285582.html, Downloaded from
59.The child’s degree of respiratory compromise is an important factor that determines management of parapneumonic effusions (Table 8,Figure 1)(strong recommendation;moderate-quality evidence)XI.What Laboratory Testing Should Be Performed on Pleural Fluid?Recommendation 60.Gram stain and bacterial culture of pleural ?uid should be performed whenever a pleural ?uid specimen is obtained.(strong recommendation;high-quality evidence)61.Antigen testing or nucleic acid ampli?cation through polymerase chain reaction (PCR)increase the detection of pathogens in pleural ?uid and may be useful for management.
(strong recommendation;moderate-quality evidence)62.Analysis of pleural ?uid parameters,such as pH and levels of glucose,protein,and lactate dehydrogenase,rarely change patient management and are not recommended.(weak recommendation;very low-quality evidence)63.Analysis of the pleural ?uid white blood cell (WBC)count,with cell differential analysis,is recommended primarily to help differentiate bacterial from mycobacterial etiologies and from malignancy.(weak recommendation;moderate-quality evidence)XII.What Are the Drainage Options for Parapneumonic Effusions?Recommendations 64.Small,uncomplicated parapneumonic effusions should not routinely be drained and can be treated with antibiotic therapy alone.(strong recommendation;moderate-quality evidence)65.Moderate parapneumonic effusions associated with respiratory distress,large parapneumonic effusions,or documented purulent effusions should be drained.(strong recommendation;moderate-quality evidence)
66.Both chest thoracostomy tube drainage with the addition
of ?brinolytic agents and VATS have been demonstrated to be effective methods of treatment.The choice of drainage procedure depends on local expertise.Both of these methods are associated
with decreased morbidity compared with chest tube drainage alone.However,in patients with moderate-to-large effusions that are free ?owing (no loculations),placement of a chest tube
without ?brinolytic agents is a reasonable ?rst option.(strong recommendation;high-quality evidence)
XIII.When Should VATS or Open Decortication Be Considered in
Patients Who Have Had Chest Tube Drainage,With or Without Fibrinolytic Therapy?
Recommendation
67.VATS should be performed when there is persistence of
moderate-large effusions and ongoing respiratory compromise despite 2–3days of management with a chest tube and completion of ?brinolytic therapy.Open chest de ′bridement with decortication represents another option for management
of these children but is associated with higher morbidity rates.
(strong recommendation;low-quality evidence)
XIV.When Should a Chest Tube Be Removed Either After Primary
Drainage or VATS?
68.A chest tube can be removed in the absence of an intrathoracic air leak and when pleural ?uid drainage is
Table 8.Factors Associated with Outcomes and Indication for Drainage of Parapneumonic Effusions
Size of effusion Bacteriology Risk of poor outcome Tube drainage with or
without ?brinolysis or VATS a Small:,10mm on lateral decubitus radiograph or opaci?es less than one-fourth of hemithorax
Bacterial culture and Gram stain results unknown or negative
Low No;sampling of pleural ?uid is not routinely required
Moderate:.10mm rim of ?uid but opaci?es less than half of the hemithorax Bacterial culture and/or Gram stain results negative or positive (empyema)Low to moderate No,if the patient has no respiratory compromise and the pleural ?uid is not consistent with empyema
(sampling of pleural ?uid by
simple thoracentesis may
help determine presence or absence
of empyema and need for a drainage
procedure,and sampling with a
drainage catheter may provide both
diagnostic and therapeutic bene?t);
Yes,if the patient has respiratory
compromise or if pleural ?uid is
consistent with empyema
Large:opaci?es more than half of the hemithorax Bacterial culture and/or Gram stain results
positive (empyema)
High Yes in most cases
a VATS,video-assisted thoracoscopic surgery.
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html, Downloaded from
,1mL/kg/24h,usually calculated over the last 12hours.(strong recommendation;very low-quality evidence)XV.What Antibiotic Therapy and Duration Is Indicated for the Treatment of Parapneumonic Effusion/Empyema?Recommendations 69.When the blood or pleural ?uid bacterial culture identi?es a pathogenic isolate,antibiotic susceptibility should be used to determine the antibiotic regimen.(strong recommendation;high-
quality evidence)70.In the case of culture-negative parapneumonic effusions,antibiotic selection should be based on the treatment recommendations for patients hospitalized with CAP (see Evidence Summary for Recommendations 46–49).(strong recommendation;moderate-quality evidence)71.The duration of antibiotic treatment depends on the adequacy of drainage and on the clinical response demonstrated for each patient.In most children,antibiotic treatment for 2–4weeks is adequate.(strong recommendation;low-quality evidence)MANAGEMENT OF THE CHILD NOT
RESPONDING TO TREATMENT
XVI.What Is the Appropriate Management of a Child Who Is Not Responding to Treatment for CAP?
Recommendation
72.Children who are not responding to initial therapy after 48–72hours should be managed by one or more of the following:a.Clinical and laboratory assessment of the current
severity of illness and anticipated progression in order to determine whether higher levels of care or support are required.(strong recommendation;low-quality evidence)b.Imaging evaluation to assess the extent and progression of the pneumonic or parapneumonic process.(weak
recommendation;low-quality evidence)
c.Further investigation to identify whether the original pathogen persists,the original pathogen has developed resistance to the agent used,or there is a new secondary infecting agent.(weak recommendation;low-quality
evidence)Figure 1.Management of pneumonia with parapneumonic effusion;abx,antibiotics;CT,computed tomography;dx,diagnosis;IV,intravenous;US,ultrasound;VATS,video-assisted thoracoscopic surgery.
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html, Downloaded from
73.A BAL specimen should be obtained for Gram stain and culture for the mechanically ventilated child.(strong recommendation;moderate-quality evidence)
74.A percutaneous lung aspirate should be obtained for Gram stain and culture in the persistently and seriously ill child for whom previous investigations have not yielded a microbiologic diagnosis.(weak recommendation;low-quality evidence)
75.An open lung biopsy for Gram stain and culture should be obtained in the persistently and critically ill,mechanically ventilated child in whom previous investigations have not yielded a microbiologic diagnosis.(weak recommendation; low-quality evidence)
XVII.How Should Nonresponders With Pulmonary Abscess or Necrotizing Pneumonia Be Managed?
Recommendation
76.A pulmonary abscess or necrotizing pneumonia identi?ed in a nonresponding patient can be initially treated with intravenous antibiotics.Well-de?ned peripheral abscesses without connection to the bronchial tree may be drained under imaging-guided procedures either by aspiration or with a drainage catheter that remains in place,but most abscesses will drain through the bronchial tree and heal without surgical or invasive intervention.(weak recommendation;very low-quality evidence) DISCHARGE CRITERIA
XVIII.When Can a Hospitalized Child With CAP Be Safely Discharged?
Recommendations
77.Patients are eligible for discharge when they have documented overall clinical improvement,including level of activity,appetite,and decreased fever for at least12–24hours. (strong recommendation;very low-quality evidence)
78.Patients are eligible for discharge when they demonstrate consistent pulse oximetry measurements.90%in room air for at least12–24hours.(strong recommendation;moderate-quality evidence)
79.Patients are eligible for discharge only if they demonstrate stable and/or baseline mental status.(strong recommendation; very low-quality evidence)
80.Patients are not eligible for discharge if they have substantially increased work of breathing or sustained tachypnea or tachycardia(strong recommendation;high-quality evidence) 81.Patients should have documentation that they can tolerate their home anti-infective regimen,whether oral or intravenous, and home oxygen regimen,if applicable,before hospital discharge.(strong recommendation;low-quality evidence)
82.For infants or young children requiring outpatient oral antibiotic therapy,clinicians should demonstrate that parents are able to administer and children are able to comply adequately with taking those antibiotics before discharge. (weak recommendation;very low-quality evidence)
83.For children who have had a chest tube and meet the requirements listed above,hospital discharge is appropriate
after the chest tube has been removed for12–24hours,either
if there is no clinical evidence of deterioration since removal or
if a chest radiograph,obtained for clinical concerns,shows
no signi?cant reaccumulation of a parapneumonic effusion
or pneumothorax.(strong recommendation;very low-quality evidence)
84.In infants and children with barriers to care,including concern about careful observation at home,inability to comply
with therapy,or lack of availability for follow-up,these issues
should be identi?ed and addressed before discharge.(weak recommendation;very low-quality evidence)
XIX.When Is Parenteral Outpatient Therapy Indicated,In
Contrast to Oral Step-Down Therapy?
Recommendations
85.Outpatient parenteral antibiotic therapy should be offered to families of children no longer requiring skilled nursing care in an acute care facility but with a demonstrated
need for ongoing parenteral therapy.(weak recommendation; moderate-quality evidence)
86.Outpatient parenteral antibiotic therapy should be offered through a skilled pediatric home nursing program
or through daily intramuscular injections at an appropriate pediatric outpatient facility.(weak recommendation;low-quality evidence)
87.Conversion to oral outpatient step-down therapy when possible,is preferred to parenteral outpatient therapy.(strong recommendation;low-quality evidence)
PREVENTION
XX.Can Pediatric CAP Be Prevented?
Recommendations
88.Children should be immunized with vaccines for bacterial pathogens,including S.pneumoniae,Haemophilus in?uenzae
type b,and pertussis to prevent CAP.(strong recommendation;
high-quality evidence)
89.All infants$6months of age and all children and adolescents should be immunized annually with vaccines for
in?uenza virus to prevent CAP.(strong recommendation;high-
quality evidence)
90.Parents and caretakers of infants,6months of age, including pregnant adolescents,should be immunized with vaccines for in?uenza virus and pertussis to protect the infants
from exposure.(strong recommendation;weak-quality evidence)
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
91.Pneumococcal CAP after in?uenza virus infection is decreased by immunization against in?uenza virus.(strong recommendation;weak-quality evidence)
92.High-risk infants should be provided immune prophylaxis with respiratory syncytial virus(RSV)–speci?c monoclonal antibody to decrease the risk of severe pneumonia and hospitalization caused by RSV.(strong recommendation; high-quality evidence)
INTRODUCTION
Burden of Disease
Pneumonia is the single greatest cause of death in children worldwide[4].Each year,.2million children younger than 5years die of pneumonia,representing 20%of all deaths in children within this age group[5].Although dif?cult to quan-tify,it is believed that up to155million cases of pneumonia occur in children every year worldwide[5].
In the developed world,the annual incidence of pneumonia is 3–4cases per100children,5years old[6,7].In the United States,outpatient visit rates for CAP between1994–1995and 2002–2003were de?ned using International Classi?cation of Diseases,Ninth Revision,Clinical Modi?cation(ICD-9-CM)di-agnosis codes and reported in the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey and identi?ed rates ranging from74to92per1000 children,2years old to35–52per1000children3–6years old [8].In2006,the rate of hospitalization for CAP in children through age18years,using data from the Healthcare Cost Utilization Project’s Kids’Inpatient Database,also based on ICD-9-CM discharge diagnosis codes,was201.1per100000[9]. Infants,1year old had the highest rate of hospitalization(912.9 per100000)whereas children13–18years had the lowest rate (62.8per100000)[9].Data from the Centers for Disease Control and Prevention(CDC)document that in2006, 525infants and children,15years old died in the United States as a result of pneumonia and other lower respiratory tract in-fections[10].The reported incidence of pneumonia in children, both pathogen speci?c and as a general diagnosis,varies across published studies based on de?nitions used,tests performed, and the goals of the investigators.CAP in children in the United States,the focus of these guidelines,is de?ned simply as the presence of signs and symptoms of pneumonia in a previously healthy child caused by an infection that has been acquired outside of the hospital[11,12].However,pneumonia de?-nitions can also be designed to be very sensitive for epidemio-logic considerations(eg,fever and cough)or very speci?c,as de?ned by government regulatory agencies for approval of antimicrobials to treat pneumonia(eg,clinical symptoms and signs in combination with radiologic documentation or mi-crobiologic con?rmation)[13].Pneumonia,broadly de?ned as a lower respiratory tract infection(LRTI),may also be de?ned in
a way that is clinically oriented,to assist practitioners with di-agnosis and management.
Etiology
Many pathogens are responsible for CAP in children,most prominently viruses and bacteria[6,7,14–18].Investigators
have used a variety of laboratory tests to establish a microbial etiology of CAP.For example,diagnosis of pneumococcal pneumonia has been based on positive cultures of blood,anti-
body responses,antigen detection,and nucleic acid detection.
Each test has different sensitivity,speci?city,and positive and negative predictive values that are dependent on the prevalence
of the pathogen at the time of testing.Therefore,comparing etiologies of pneumonia between published studies is challeng-
ing.More recent investigations have used a variety of sensitive molecular techniques including nucleic acid detection,particu-
larly for viral identi?cation.In many children with LRTI,di-agnostic testing may identify2or3pathogens,including combinations of both viruses and bacteria,making it dif?cult to determine the signi?cance of any single pathogen[19–21]. Furthermore,unique to pediatrics,the developing immune system and age-related exposures result in infection caused by different bacterial and viral pathogens,requiring that the in-cidence of CAP and potential pathogens be de?ned separately
for each age group[7].
The advent of polysaccharide-protein conjugate vaccines
for H.in?uenzae type b and7serotypes of S.pneumoniae
(7-valent pneumococcal conjugate vaccine[PCV7])dramat-
ically decreased the incidence of infection,including CAP, caused by these bacteria.Newer vaccines that protect against
a greater number of pneumococcal serotypes are in various
stages of clinical development,with a newly licensed13-valent pneumococcal conjugate vaccine(PCV13)available in the
United States.Reports of epidemiologic investigations on the etiology of CAP before the widespread use of these vaccines
cited S.pneumoniae as the most common documented bacterial pathogen,occurring in4%–44%of all children investigated[14–16,18].
In some studies,viral etiologies of CAP have been docu-mented in up to80%of children younger than2years;in contrast, investigations of older children,10–16years,who had both
clinical and radiographic evidence of pneumonia,documented
a much lower percentage of viral pathogens[15,16,18,20].
Of viral pathogens,RSV is consistently the most frequently detected,representing up to40%of identi?ed pathogens in those younger than2years,but rarely identi?ed in older children
with CAP.Less frequently detected are adenoviruses,bocavirus, human metapneumovirus,in?uenza A and B viruses,para-
in?uenza viruses,coronaviruses and rhinovirus[14,16,18,22,23]. Epidemiologic investigations of hospitalized children with CAP
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
document that2%–33%are simultaneously infected by2or more viruses[19,20].
Epidemiologic studies that have assessed both viral and bac-terial pathogens have reported bacterial pathogens isolated in 2%–50%of children with CAP;inpatient studies that enroll more seriously ill children often document higher rates of bac-terial infection compared with outpatient studies[16,17,20,21]. Pathogens responsible for‘‘atypical pneumonia’’have been identi?ed in3%–23%of children studied,with M.pneumoniae most often identi?ed in older children and C.pneumoniae in infants[14–18].Atypical pneumonia caused by Mycoplasma is characteristically slowly progressing,with malaise,sore throat, low-grade fever,and cough developing over3–5days.In con-trast to adults with pneumonia,Legionella sp.has only rarely been identi?ed in children[24].
Although CAP caused by Mycobacterium tuberculosis and the nontuberculous mycobacteria have been well-documented, the incidence of these serious infections in the United States is far less than that of viral or bacterial CAP and is often linked to high-risk exposures[25].Likewise,fungal pneumonia in normal hosts caused by Histoplasma,Coccidioides,Blastomyces, and Cryptococcus is uncommon,and in most epidemiologic studies,children with fungal pneumonia are not identi?ed. Mycobacterial and fungal pneumonia are not addressed in these guidelines.
Clinical Questions Addressed by the Expert Panel
Site-of-Care Management Decisions
I.When does a child or infant with CAP require hospitalization? II.When should a child with CAP be admitted to an intensive care unit(ICU)or a unit with continuous cardiorespiratory monitoring?
Diagnostic Testing for Pediatric CAP
III.What diagnostic laboratory and imaging tests should be used in a child with suspected CAP in a clinic or hospital ward setting?
IV.What additional diagnostic tests should be used in a child with severe or life-threatening CAP?
Anti-Infective Treatment
V.Which anti-infective therapy should be provided to a child with suspected CAP in both the outpatient and inpatient settings? VI.How can resistance to antimicrobials be minimized? VII.What is the appropriate duration of antimicrobial ther-apy for CAP?
VIII.How should the clinician follow up the child with CAP for the expected response to therapy?
Adjunctive Surgical and Non–Anti-infective Therapy for Pediatric CAP
IX.How should a parapneumonic effusion be identi?ed? X.What factors are important in determining whether drainage of the parapneumonic effusion is required?
XI.What laboratory testing should be performed on pleural
?uid?
XII.What are the drainage options for parapneumonic effu-sions?
XIII.When should VATS or open surgical decortication be considered in patients who have had chest tube drainage with or without?brinolytic therapy?
XIV.When should a chest tube be removed either after pri-
mary drainage or VATS?
XV.What antibiotic therapy and duration is indicated for the treatment of parapneumonic effusion/empyema?(see also sec-
tion on Anti-infective Treatment)
Management in the Child Not Responding to Treatment
XVI.What is the appropriate management of a child who is
not responding to treatment for CAP?
XVII.How should the nonresponder with a pulmonary ab-
scess or necrotizing pneumonia be managed?
Discharge Criteria
XVIII.When can a hospitalized child with CAP be safely discharged?
XIX.When is parenteral outpatient therapy indicated,in contrast to oral step-down therapy?
Prevention
XX.Can pediatric CAP be prevented?
There are many aspects to the clinical management of CAP and
its complications(Table2).Clinical practice recommendations regarding the daily management of children hospitalized with
CAP,including intravenous?uid management,techniques for delivery of and monitoring oxygenation,and management of respiratory tract secretions as well as important economic and
social issues were beyond the scope of this?rst edition of the pediatric CAP guidelines and were not addressed by the panel.
METHODOLOGY
Practice Guidelines
Practice guidelines are‘‘systematically developed statements to
assist practitioners and patients in making decisions about ap-propriate health care for speci?c clinical circumstances’’[26]. Attributes of good guidelines include validity,reliability,re-producibility,clinical applicability,clinical?exibility,clarity, multidisciplinary process,review of evidence,and documenta-
tion[26].
Panel Composition
The Pediatric Infectious Diseases Society(PIDS)and the IDSA Standards and Practice Guidelines Committee(SPGC)convened experts in pediatric CAP from the?elds of community pediat-
rics,public health,and the pediatric subspecialties of critical care medicine,emergency medicine,hospital medicine,infectious diseases,pulmonology,and surgery.Panel participants included representatives from the following collaborating organizations:
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
American Academy of Pediatrics(AAP),American College of Emergency Physicians,American Thoracic Society–Pediatric Section,Society for Hospital Medicine,the Society of Critical Care Medicine,and the American Pediatric Surgical Association. In addition,expert consultants in diagnostic microbiology including virology,and interventional radiology were asked to review and provide feedback on the draft guidelines.
Process Overview
As with other clinical practice guidelines developed by IDSA, a need for guidelines for pediatric CAP was demonstrated and the goals for the guidelines were similar to those for CAP in adults[27].Clinical questions were developed by the writing group and approved by the IDSA https://www.360docs.net/doc/2217285582.html,puterized litera-ture searches of the National Library of Medicine PubMed da-tabase were performed to identify data published through May 2010,although more recent articles with particular relevance to these guidelines have been included.Relevant abstracts from recent professional meetings and existing guidelines on pediatric CAP were also identi?ed,collected,and reviewed.
As with all IDSA clinical practice guidelines initiated after 1October2008,the expert panel employed the GRADE(Grades of Recommendation,Assessment,Development,and Evalua-tion)method of assigning strength of recommendation and quality of the evidence to each recommendation(see Table2) [3].As applied to these guidelines,the writing group believes that in circumstances for which the quality of evidence is low or very low,there are likely to be situations in which even strong recommendations may not apply to speci?c subgroups within a population that is intended for that recommendation.For many conditions that lack moderate-or high-quality evidence, clinical judgment still plays an important role in management. Unfortunately,for many situations,current,prospectively col-lected,high-quality evidence was not available,highlighting the critical need for further investigation in order to establish a solid basis for future recommendations.
Consensus Development Based on Evidence
The expert panel met initially on3occasions via teleconference to complete the organizational work of the guideline,and in person at the2009Annual Meeting of the IDSA.Within the panel,subgroups were formed for each clinical question. Each subgroup reviewed the literature relevant to that clinical question and was responsible for drafting the recom-mendation(s)and evidence summaries for their assigned sec-tion.The drafts were circulated within the panel for commentary and discussed in additional conference calls and during a face-to-face meeting held in conjunction with the2010 Pediatric Academic Societies meeting.Further re?nement of the recommendations and evidence summaries occurred in 4subsequent teleconference calls.
All members of the panel participated in the preparation and
review of the draft guidelines.Feedback was solicited from ex-
ternal peer reviewers and from the organizations represented on
the expert panel.These guidelines have been endorsed by the
AAP,the American College of Emergency Physicians,the American Society of Microbiology,the American Thoracic So-
ciety,the Society for Hospital Medicine,and the Society of Critical Care Medicine.The guidelines were reviewed and ap-proved by the PIDS Clinical Affairs Committee,the IDSA SPGC,
the Council of the PIDS,and the Board of Directors of the IDSA
before dissemination.
Guidelines and Conflict of Interest
All members of the expert panel complied with the IDSA
policy on con?icts of interest that requires disclosure of any
?nancial or other interest that might be construed as consti-
tuting an actual,potential,or apparent con?ict.They were
given the IDSA con?icts of interest disclosure statement
and were asked to identify ties to companies developing products that might be affected by promulgation of the https://www.360docs.net/doc/2217285582.html,rmation was requested regarding employ-ment,consultancies,stock ownership,honoraria,research funding,expert testimony,and membership on company advisory committees.The panel made decisions on a case-
by-case basis as to whether an individual’s role should be
limited as a result of a con?ict.Potential con?icts are listed in
the Acknowledgments section.
GUIDELINE RECOMMENDATIONS FOR
MANAGEMENT OF CAP IN INFANTS AND
CHILDREN
Site-of-Care Management Decisions
I.When Does a Child or Infant With CAP Require Hospitalization?
Recommendations
1.Children and infants who have moderate to severe CAP as
de?ned by several factors,including respiratory distress and hypoxemia(sustained SpO2,,90%at sea level)(Table3)
should be hospitalized for management including skilled pediatric nursing care.(strong recommendation;high-quality evidence)
2.Infants,3–6months of age with suspected bacterial
CAP are likely to bene?t from hospitalization.(strong recommendation;low-quality evidence)
3.Children and infants with a suspicion or documentation
of CAP caused by a pathogen with increased virulence,such as
CA-MRSA,should be hospitalized.(strong recommendation;
low-quality evidence)
4.Children and infants for whom there is concern about
careful observation at home or who are unable to comply with
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
therapy or unable to be followed up should be hospitalized. (strong recommendation;low-quality evidence)
Evidence Summary
These guidelines are primarily designed to address infants and children living in the United States,with reasonable access to healthcare.The history,presentation,and examination of the child are the major determinants of the severity of the illness and the appropriate level of care with respect to outpatient or in-patient management.The physician’s overall assessment of the child’s status,at the time of examination and the anticipated clinical course should determine the site of care.However,the guidelines writing group recognizes that data from chest radi-ography,pulse oximetry,or laboratory studies are used variably by practitioners to support medical decision making.For these guidelines,we de?ne‘‘simple pneumonia’’as either broncho-pneumonia(primary involvement of airways and surrounding interstitium),or lobar pneumonia involving a single lobe.‘‘Complicated pneumonia’’is de?ned as a pulmonary paren-chymal infection complicated by parapneumonic effusions, multilobar disease,abscesses or cavities,necrotizing pneumonia, empyema,pneumothorax or bronchopleural?stula;or pneu-monia that is a complication of bacteremic disease that includes other sites of infection.
For resource-poor regions of the world,the World Health Organization(WHO)de?nes pneumonia primarily as cough or dif?cult breathing and age-adjusted tachypnea:(age2–11months, $50/min;1–5years,$40/min;$5years,.20breaths/min) [5].Furthermore,severe pneumonia is de?ned as‘‘cough or dif?culty breathing plus one of the following:lower chest in-drawing,nasal?aring,or grunting.’’Very severe pneumonia is de?ned as‘‘cough or dif?culty breathing plus one of the fol-lowing:cyanosis,severe respiratory distress,inability to drink or vomiting everything,or lethargy/unconsciousness/con-vulsions.’’Such de?nitions of various levels of severity and studies to validate interventions for each level of severity are not well characterized for children living in resource-rich areas of the world.
At the more severe end of the spectrum of clinical pre-sentation,most experts and professional societies recommend that any child or infant with respiratory distress(Table3)should be admitted to the hospital for management[28–31].Com-parative studies from the developed world,evaluating the out-comes of children with various degrees of respiratory distress who are managed as outpatients compared with those managed as inpatients,have not been published.A‘‘toxic appearance,’’which is not well de?ned but is represented by the components provided in Table3,is universally accepted as an indication for admission to the hospital[28,29].
In the past few decades,many consensus guidelines and clinical decision rules have been proposed for adults with CAP [27,32–38].There are multiple adult studies that describe scoring systems that have been demonstrated to be useful in predicting both which adults should be hospitalized and which
adults require intensive care[27,32–38].Unfortunately,these scoring systems have not been validated in children and do not consider pediatric comorbid conditions,developmental stage,or psychosocial factors that in?uence the treating clinician’s de-
cision on the site of treatment for pediatric patients with CAP [39].
Validated scoring systems to predict which children with pneumonia should be hospitalized do not exist.Scores to predict mortality in critically ill children hospitalized in pediatric ICUs
have existed for2decades[40].Severity of illness scores built
upon multiple logistic regression models,such as the Pediatric
Risk of Mortality score and the Pediatric Index of Mortality
predict the risk of death for children in ICU settings.These may facilitate outcome prediction in the ICU but do not reliably help
the clinician to discriminate severity of illness in the less acutely
ill child,thereby limiting utility in level-of-care decision making
[41–44].
More directly relevant to evaluating severity of disease in CAP
is the simple measurement of oxygenation by pulse oximetry. Hypoxemia is well established as a risk factor for poor outcome
in children and infants with any type of disease,especially re-spiratory diseases.The use of pulse oximetry to detect hypox-
emia has con?rmed this relationship such that guidelines and
clinical decision rules usually recommend pulse oximetry in any
patient with pneumonia.In the developing world,for pediatric patients with nonsevere pneumonia(as de?ned by WHO),
a pulse oximetric SpO2measurement of,90%at the initial visit
has been documented to be predictive of failure of outpatient
oral amoxicillin treatment[45].In adults,hypoxemia is an in-
dicator for respiratory failure requiring ICU admission in pa-
tients with pneumonia[46,47]and has also been independently associated with short-term mortality[32,48].Widespread agreement exists that admission is indicated in a previously healthy child with CAP and an oxygen saturation in room air
(at sea level)of,90%,although some would hospitalize chil-
dren who have oxygen saturations as high as93%[49].At higher altitudes,lower oxygen saturations may be more appropriate to
de?ne respiratory failure,as demonstrated in Bolivia[50].
Clinical surrogates exist for adequate oxygenation,or,con-versely,for hypoxemia and severe pneumonia.The child or infant’s overall general assessment and ability to be consoled usually denote normal oxygenation[51].‘‘A moderate or severe alteration of general status’’was an independent risk factor for
death in children hospitalized in the developing world with an
acute LRTI[52].Although cyanosis may sometimes be dif?cult
to detect,its presence denotes severe hypoxemia[52].A sys-tematic review of published studies,primarily in the developing world,found that central cyanosis had a higher speci?city for predicting hypoxemia in children than other signs[53].
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
Tachypnea is a nonspeci?c clinical sign,but may represent a marker for respiratory distress and/or hypoxemia.‘‘Rapid breathing as perceived by the mother’’was statistically associated with hypoxemia in a study of children with pneumonia[50].An increase in the age-speci?c respiratory rate or tachypnea has been linked to treatment failure in children with severe pneu-monia in the developing world[54].Although tachypnea in infants with pneumonia may correlate with presence of hyp-oxemia,tachypnea may also be caused by fever,dehydration,or a concurrent metabolic acidosis[55].In a study from a pediatric emergency department in Boston of children,5years old un-dergoing chest radiography for possible pneumonia,the re-spiratory rates for those with documented pneumonia did not differ signi?cantly from those for children without pneumonia. However,of children with WHO-de?ned tachypnea,20%had con?rmed pneumonia,compared with12%without tachypnea [56].
Retractions and grunting have also been found to be in-dicators of increased severity of LRTIs in children hospitalized in Argentina[57].Retractions,whether intercostal,suprasternal or subcostal indicate a greater severity of pneumonia[29].Nasal ?aring and‘‘head bobbing’’have also been statistically associ-ated with hypoxemia[50].
Dehydration,vomiting,or inability to take oral medication are additional considerations for hospitalization.Children in whom oral outpatient antimicrobial therapy has been attempted unsuccessfully and who demonstrate new and progressive re-spiratory distress(Table3)will most often require hospitaliza-tion.Furthermore,those with psychosocial concerns,such as noncompliance with therapy or lack of reliable follow-up for any reason,may warrant admission[28,29,31].Studies from both the United States[58]and Canada[59]found that children and infants with pneumonia were more likely to be hospitalized if they were of lower socioeconomic status.This may be attributed, in part,to nonmedical issues,including inaccessibility to ade-quate outpatient services.
Children with pneumonia caused by CA-MRSA,as described in case series,have a high incidence of necrotizing pneumonia and frequently require ICU admission[60,61].In a retrospec-tive study of both adults and children with Panton-Valentine leukocidin–positive S.aureus CAP,78%required mechanical ventilation[43].If there is high suspicion for or documentation of CA-MRSA as a causative organism,the clinician should hospitalize the child for treatment with parenteral antimicrobial therapy and close observation,even if the respiratory symptoms are not severe at the time of initial evaluation.
The presence of signi?cant comorbid conditions is also a risk factor for the development of pneumonia;the presence of pneumonia often results in a worsening of the underlying condition.In Dallas,Texas,20%of children admitted with CAP had comorbid conditions,including reactive airway disease,genetic syndromes,and neurocognitive disorders[17].Tan and colleagues from8pediatric tertiary care centers found that36%
of children hospitalized for pneumococcal pneumonia had un-derlying comorbid conditions that also included immunologic disorders and hematologic,cardiac,and chronic pulmonary conditions[62].Children with a comorbid condition and in-
?uenza infection are more likely to require hospitalization than otherwise healthy children[23,63,64].Although children who
have chronic conditions may be at greater risk of pneumonia,
these conditions are extremely diverse,so speci?c management
issues for comorbid conditions will not be addressed in these guidelines[65,66].
Young age is an additional risk factor for severity of pneu-
monia and need for hospitalization.The incidence of pneu-
monia and risk of severe pneumonia are greater in infants and
young children.The attack rates are 35–40per1000infants (age,,12months),30–35per1000preschool-aged children
(2–5years),15per1000school-aged children(5–9years),and
6–12per1000children.9years old[67].Furthermore,infants
and young children tend to have more severe pneumonia with
a greater need for hospitalization and a higher risk of respiratory failure.One independent risk factor for death in children hos-pitalized for acute respiratory tract infections in the Central African Republic was age between2and11months[52]. However,malnutrition may also contribute to severity of disease
in the developing world,tempering conclusions about mortality
in this age group from respiratory tract disease alone[68].
A clinical tool designed to predict which child with severe pneumonia would have failure of oral antimicrobial therapy in
the developing world found that the age of the child was one of
the most important clinical predictors(highly signi?cant for those,6months of age)[54].In the developed world,pro-spectively collected data have not been published documenting
a cutoff age below which hospitalization is necessary for im-proved outcomes.In the United States,very young infants(up
to3months of age)with CAP are generally admitted to the hospital for initial management.Given the increased risk of morbidity,the admission of infants up to6months of age with suspected bacterial CAP is also prudent[29,69].
II.When Should a Child with CAP Be Admitted to an Intensive
Care Unit(ICU)or a Unit With Continuous Cardiorespiratory Monitoring?
Recommendations
5.A child should be admitted to an ICU if the child requires invasive ventilation via a nonpermanent arti?cial airway(eg, endotracheal tube).(strong recommendation;high-quality evidence)
6.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the
child acutely requires use of noninvasive positive pressure
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
ventilation(eg,continuous positive airway pressure or bilevel positive airway pressure).(strong recommendation;very low-quality evidence)
7.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child has impending respiratory failure.(strong recommendation; moderate-quality evidence)
8.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child has sustained tachycardia,inadequate blood pressure,or need for pharmacologic support of blood pressure or perfusion. (strong recommendation;moderate-quality evidence)
9.A child should be admitted to an ICU if the pulse oximetry measurement is#92%with inspired oxygen of $0.50.(strong recommendation;low-quality evidence)
10.A child should be admitted to an ICU or a unit with continuous cardiorespiratory monitoring capabilities if the child has altered mental status,whether due to hypercarbia or due to hypoxemia as a result of pneumonia.(strong recommendation; low-quality evidence)
11.Severity of illness scores should not be used as the sole criterion for ICU admission but should be used in the context of other clinical,laboratory,and radiologic?ndings.(strong recommendation;low-quality evidence)
Evidence Summary
When a child requires hospitalization for CAP,the clinician needs to consider the capabilities of the accepting facility or unit. Variations in the level of monitoring and in the skills of the bedside providers(nurse,respiratory therapist,and physician) will in?uence the decision on where to effectively monitor and treat the ill child.Appropriate placement of the ill child with increased work of breathing,tachypnea,or hypoxemia optimizes the use of ICU and general care area resources.Consultation with a specialist in pediatric critical care medicine is recom-mended if there is any concern regarding appropriate patient placement based on severity of disease(Table4).ICU-level care is not typically required for children with CAP.However,in a study from Dallas,Texas,6.5%of children hospitalized with CAP re-quired mechanical ventilation[17],and1.3%of children with CAP died,although almost one-third had comorbid conditions.
A greater proportion of those with mixed bacterial and viral infections required mechanical ventilation(8.3%);mortality was 5.6%in this subgroup of children hospitalized with CAP[17]. Hypoxemia is present in many children with CAP,and in many cases low-?ow supplemental oxygen provided by nasal cannula or face mask will suf?ce to restore oxygenation satu-ration for management on a hospital ward.Children requiring a fraction of inspired oxygen(FiO2)of$0.50to maintain sat-uration.92%should be cared for in a unit capable of contin-uous cardiorespiratory monitoring and rapid response should the clinical situation worsen.Other signs of respiratory distress and potential respiratory insuf?ciency include increased work of breathing(as evidenced by retractions[suprasternal,subcostal,
or intercostals]),nasal?aring,and use of accessory muscles), recurrent apnea,or grunting.Grunting,when present,is a sign
of severe disease and impending respiratory failure[71].Oxygen saturation by pulse oximetry is usually monitored continuously
for a child with increased work of breathing or signi?cant dis-tress,particularly if he or she has a decreased level of activity or agitation[51].
The child’s overall clinical appearance and behavior may
predict as much about the severity of illness as any score avail-
able.The exclusive use of severity of illness scores at hospital admission does not reliably provide the clinician with enough
data to determine the need for ICU-level care.
The arterial oxygen pressure PaO2/FiO2ratio provides an indication of the degree of respiratory insuf?ciency and im-
paired oxygen diffusion and,in conjunction with clinical ex-amination,will enhance the determination of illness severity.
This test requires an arterial blood gas determination of the
PaO2,so its use is warranted only in evaluation of severe CAP
with interpretation of the PaO2/FiO2ratio by a physician experienced in treating children with respiratory failure.
The severity of pneumonia and need for ICU admission may
be de?ned in part by the etiology.In a retrospective review of children admitted to a pediatric tertiary care center with invasive pneumococcal infection,those with concurrently positive viral studies(in?uenza,rhinovirus,adenovirus,RSV),were admitted
to pediatric ICU more frequently and found to have longer pediatric ICU stays[72].In2retrospective case series of pedi-
atric patients,CA-MRSA pneumonia has been shown to have
a high incidence of necrotizing pneumonia,a need for ICU care,
and high associated mortality[60,61].
DIAGNOSTIC TESTING FOR PEDIATRIC CAP
III.What Diagnostic Laboratory and Imaging Tests Should Be
Used in a Child With Suspected CAP in an Outpatient or
Inpatient Setting?
Recommendations
Microbiologic Testing
Blood Cultures:Outpatient
12.Blood cultures should not be routinely performed in nontoxic,fully immunized children with CAP managed in the outpatient setting.(strong recommendation;moderate-quality evidence)
13.Blood cultures should be obtained in children who fail to demonstrate clinical improvement and in those who have progressive symptoms or clinical deterioration after initiation
of antibiotic therapy(strong recommendation;moderate-quality evidence).
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
Blood Cultures:Inpatient
14.Blood cultures should be obtained in children requiring hospitalization for presumed bacterial CAP that is moderate to severe,particularly those with complicated pneumonia.(strong recommendation,low-quality evidence)
15.In improving patients who otherwise meet criteria for discharge,a positive blood culture with identi?cation or susceptibility results pending should not routinely preclude discharge of that patient with appropriate oral or intravenous antimicrobial therapy.The patient can be discharged if close follow-up is assured.(weak recommendation;low-quality evidence)
Follow-up Blood Cultures
16.Repeat blood cultures in children with clear clinical improvement are not necessary to document resolution of pneumococcal bacteremia.(weak recommendation;low-quality evidence)
17.Repeat blood cultures to document resolution of bacteremia should be performed in children with bacteremia caused by S.aureus,regardless of clinical status.(strong recommendation;low-quality evidence)
Sputum Gram Stain and Culture
18.Sputum samples for culture and Gram stain should be obtained in hospitalized children who can produce sputum. (weak recommendation;low-quality evidence)
Urinary Antigen Detection Tests
19.Urinary antigen detection tests are not recommended for the diagnosis of pneumococcal pneumonia in children; false-positive results are common.(strong recommendation; high-quality evidence)
Testing For Viral Pathogens
20.Sensitive and speci?c tests for the rapid diagnosis of in?uenza virus and other respiratory viruses should be used in the evaluation of children with CAP.A positive in?uenza test result may both decrease the need for additional diagnostic studies and decrease antibiotic use,while guiding appropriate use of antiviral agents in both outpatient and inpatient settings. (strong recommendation;high-quality evidence)
21.Antibacterial therapy is not necessary for children,either outpatients,or inpatients,with a positive test result for in?uenza virus in the absence of clinical,laboratory,or radiographic?ndings that suggest bacterial coinfection. (strong recommendation;high-quality evidence)
22.Testing for respiratory viruses other than in?uenza virus can modify clinical decision making in children with suspected pneumonia,because antibacterial therapy will not routinely be required for these children in the absence of clinical,laboratory,or radiographic?ndings that suggest bacterial coinfection. (weak recommendation;low-quality evidence)
Testing for Atypical Bacteria
23.Children with signs and symptoms suspicious for
M.pneumoniae should be tested to help guide antibiotic selection.(weak recommendation;moderate-quality evidence)
24.Diagnostic testing for C.pneumoniae is not recommended
as reliable,and readily available diagnostic tests do not currently
exist.(strong recommendation;high-quality evidence)
Ancillary Diagnostic Testing
Complete Blood Cell Count
25.Routine measurement of the complete blood cell count is
not necessary in all children with suspected CAP managed in the outpatient setting,but for those with more serious disease it may provide useful information for clinical management in the context of the clinical examination and other laboratory and imaging studies.(weak recommendation;low-quality evidence)
26.A complete blood cell count should be obtained for patients with severe pneumonia,to be interpreted in the context
of the clinical examination and other laboratory and imaging studies.(weak recommendation;low-quality evidence)
Acute-Phase Reactants
27.Acute-phase reactants such as the ESR,CRP,or serum procalcitonin cannot be used as the sole determinant to distinguish between viral and bacterial causes of CAP.(strong recommendation;high-quality evidence)
28.Acute-phase reactants need not be routinely measured in
fully immunized children with CAP who are managed as outpatients,although for more serious disease,they may provide useful information for clinical management.(strong recommendation;low-quality evidence)
29.In patients with more serious disease,such as those requiring hospitalization or those with pneumonia-associated complications,acute-phase reactants may be used in conjunction with clinical?ndings to assess response to therapy.(weak recommendation;low-quality evidence)
Pulse Oximetry
30.Pulse oximetry should be performed in all children with pneumonia and suspected hypoxemia.The presence of hypoxia
should guide decisions regarding site of care and further diagnostic testing.(strong recommendation;moderate-quality evidence)
Chest Radiography
Initial Chest Radiographs:Outpatient
31.Routine chest radiographs are not necessary for the
con?rmation of suspected CAP in patients well enough to be
at IDSA on August 31, 2011
https://www.360docs.net/doc/2217285582.html,
Downloaded from
案例分析考核——社区获得性肺炎(daan)
(案例已经修改)案例考核——社区获得性肺炎 患者男,47岁,身高180cm,体重75kg,于4月7入院。 主诉:乏力、发热伴咳嗽、咳痰一周。 现病史:患者于一周前因劳累、受凉后出现乏力、发热,伴畏寒、咳嗽、咽痛,无寒战,无呕吐,无皮疹,咳嗽,咳少量白色粘痰,无咯血。发热最高至40.2℃,在家自服“布洛芬混悬液”后,出汗,热退。每日夜间发热,第二日发热时间前移。于社区门诊静脉注射“头孢”等药物(每日一次,具体药物及用量不详),症状未能控制。4月4日于我院门诊治疗给予“哌拉西林/他唑巴坦4.5g q12h、阿奇霉素0.25 qd”等抗感染治疗,体温仍不能控制,为求进一步治疗,收入院。 患者自发病以来,神智清,精神可,进食可,大小便未见异常,体重无明显变化。 既往史:既往体健,无结核等传染病接触史。 个人史:生于原籍,无外地及疫区久居史。否认吸烟饮酒史及其他不良嗜好。家族史:父母亲体健。否认家族遗传病史。 过敏史:否认食物、药物过敏史。 查体:T 38℃P 76次/分R 18次/分BP 108/52mmHg SPO2 96% 中年男性,急性病容,神智清,发育正常,营养中等,步入病房,查体合作。全身皮肤无黄染、无瘀斑,浅表淋巴结无肿大。头颅无畸形,结膜无充血,苍白,巩膜不黄,口唇微紫绀,口腔黏膜无溃疡,咽红充血,双侧扁桃体不大。颈软,气管居中,甲状腺不肿大。胸廓对称,无胸壁静脉曲张,无胸壁压痛。双肺呼吸
音低,未闻及干湿性啰音。心界不扩大,心率76次/分,律齐,S1低钝,各瓣膜听诊区未闻及病理性杂音,无心包摩擦音。腹软,无压痛及反跳痛,未见胃肠蠕动波,肝脾肋下未及,无移动性浊音,麦氏点无压痛;脊柱四肢正常,无双下肢浮肿,莫非氏征(—),双侧巴氏征(—)。 辅助检查: 4月4 日血常规:WBC13.72×109L N 83.5 % L 10.3% 4月4日胸片:双肺纹理增多,右下肺炎不能排除,建议进一步检查。 4月7日肺CT:右下肺炎。 入院诊断: 社区获得性肺炎 出院诊断: 社区获得性肺炎 主要药物治疗方案:
单病种社区获得性肺炎-住院、儿童
漳州市第三医院 单病种质控登记表 第一诊断:社区获得性肺炎-住院、儿童(ICD-10 J13-J15,J18) 患者姓名:性别:年龄:床号住院号 发病时间: 年月日时分 到达医院急/门诊时间: 年月日时分 入院时间: 年月日时分 一、住院时病情严重程度评估 1.符合入院标准 □呼吸空气时SaO2 ≤0.92(海平面)或≤0.90(高原)有中心性紫绀 □呼吸困难,胸壁吸气性凹陷,鼻煽 □间歇性呼吸暂停,呼吸呻吟 □持续高热3-5天不退或有先天性心脏病、先天性支气管发育不良、先天性呼吸道发育不良、重度贫血、重度营养不良等基础疾病 □胸片等医学影像资料证实双侧或多肺叶受累或肺叶实变并肺不张、胸腔积液或短期内病变进展者 □拒食或并有脱水者 2.符合重症/入住ICU标准 □吸入氧浓度(FiO2)≧0.6,SaO2 ≤0.92(海平面)或≤0.90(高原) □休克和(或)意识障碍 □呼吸频率加快、脉速伴严重呼吸窘迫和耗竭征象,伴或不伴PaCO2 升高 □反复出现呼吸暂停或出现慢而不规则的呼吸 3.主要伴随疾病: 二、氧合评估(入院后首次) 1.动脉血气分析(PaO2): 2.指氧仪检查(SatO2): 3.氧合指数=PaO2/FiO2(计算值): 三、病原学检测 1.住院24小时以内采集血、痰培养是□否□ 在门诊已用抗菌药:是□否□ 2.在首次抗菌药物治疗前采集血、痰培养是□否□ 在外院已用抗菌药:是□否□ 四、抗菌药物使用时机□入院4h内□入院6h内□入院8h内 五、起始抗菌药物选择 1.重症/ICU患者起始抗菌药物选择 □羟氨苄青霉素+克拉维酸或氨苄青霉素+舒巴坦 □头孢呋辛或头孢曲松或头孢噻亏 □苯唑青霉素+头孢曲松或头孢噻亏 □大环内酯类+头孢曲松或头孢噻亏 □其他 2.非重症患者起始抗菌药物选择 □阿莫西林或阿莫西林+克拉维酸 □头孢二代 □□克林霉素 □大环内酯类 □其他
小儿重症肺炎
婴幼儿重症肺炎 婴幼儿重症肺炎是儿科医生在临床工作中经常遇到的病例。症状重,处理难度较大,有些病例反复发作。因此我们要认识其发病机制,和主要病因与诱因、临床过程中呈现的不同状态,合理和规范化临床治疗对策,是病情好转避免呼吸衰竭的关键。 一、病因和发病机制 1.病因婴幼儿支气管肺炎的主要病原体是细菌、病毒、支原体,近年来由于抗生素滥用问题日益严重,特别是许多新抗生素的广泛使用,使得耐药菌株的感染成为细菌感染的主要原因。病毒性和支原体性肺炎也显著增加。 儿童不同年龄阶段社区获得性肺炎的病原学 病原体直接侵袭,机体反应性改变,免疫机制参与,三者共同作用。 二、临床表现 多数患儿先有上呼吸道感染,逐渐出现发热、咳嗽、气促,多数热型不规则,亦有表现弛张热或稽留热。其它表现还有进食困难,呕吐,腹泻等,少数有些有皮疹。 常见体征包括呼吸急促、鼻翼扇动、三凹征、喘憋、烦躁、紫绀、矛盾呼吸等。听诊有喘鸣音/湿罗音。肺泡含气量增加时,膈肌下移使肝下界下移。 X线胸片示肺内斑片状影,可明确肺炎诊断。 病原学诊断:鼻咽分泌物培养,特异抗体测定等。 三、同病原肺炎的严重状态 包括原发感染所致的全身严重状态;肺部病变的广泛程度或累及胸腔、纵膈;肺脏与其它脏器功能不全或衰竭,即败血症、休克、呼吸衰竭甚至MODS。 不同病原肺炎的临床表现特点
四、婴儿重症肺炎三种临床状态及发展趋势 重症肺炎患儿临床上存在着不同的病因和病情发展过程。我们归纳为以下三种状态,有时以某种为主,也可互相交叉、重叠发生,在危重症病例多为同时存在。 1.急诊状态:肺炎患儿突然出现以下情况常使病情恶化,包括气道高反应性、气道梗阻、分泌物潴留、呼吸暂停、抽搐、呛奶、胃食道反流、呼吸肌疲劳等。此时处于潜在呼吸衰竭(impending respiratory failure)或临界呼吸衰竭(criticalrespiratory failure)状态,严重者立即出现呼吸衰竭,甚至呼吸心跳骤停。以急诊状态收入PICU患儿占2/3。 婴儿气道高反应性的发生率逐年增加,且严重度加重。病因有RSV感染、先心病肺充血、有早产史患儿、新生儿期遗留慢性肺疾患、胃食道反流、气道对各种物理化学刺激敏感,如吸入气体过冷、过热,湿度过大或不足、体位不适,吸痰过度刺激,甚至疼痛哭闹等均可诱发。 临床表现为发作性呼吸困难、喘憋、三凹征、紫绀。因均存在气道病变,加之气道窄,咳嗽能力弱,易呛奶,有时吸气音几乎消失,发生窒息、呼吸衰竭、心力衰竭和心肺功能衰竭。很多婴儿重症肺炎(以病毒性多见)可发生气道梗阻的急诊状态。严重者可发展为闭塞性毛细支气管炎(bronchiolitis obliterans)。这种急诊情况可以发生在家庭、急诊室、普通病房和ICU内,常需紧急气管插管辅助通气,因气道高反应性常呈反复发作,可持续数小时,也可在数天至数周内反复发生。严重时即使在气管插管常规机械通气下,亦很难维持有效通气和氧合。处理需在有经验的上级医师指导下进行。 心跳呼吸骤停是重症肺炎急诊的最严重情况。发作时可出现急性心衰,其重要机制之一是心肺互相影响,胸腔负压的急速增加导致左室跨壁压增加,使左室搏出量下降。我院5年内共89例次,每年分别在6~10例次,即使在PICU监测条件下也仍有发生。反映了婴儿重症肺炎急诊状态的危险程度。 2.危重状态:即急性肺损伤(ALI)和急性呼吸窘迫综合征(ARDS) 重症肺炎可发展为ALI和ARDS。甚至继续发展为休克和多脏器功能障碍综合症(MODS),约占PICU 婴儿重症肺炎1/3,病程中也可发生上述气道高反应性等急诊事件。发生ALI或ARDS时,肺部感染启动异常全身炎症反应,有细胞因子和炎症介质参与,使肺部病变迅速加重,表现严重低氧血症,普通给氧不能缓解,需要在ICU内给予呼气末正压(PEEP)为主的机械通气。同时患儿可合并脑水肿、DIC、中毒性心肌炎、脓胸和胸腔积液、肺大疱等并发症。死亡率较高。本PICU资料显示典型ARDS病例65例(11.8%),死亡44例(67.7%)。按照近年来诊断标准回顾分析显示,ALI约占1/4~1/3。 婴儿ALI的特点为:常存在肺瘀血,肺水肿,肺出血和气道高反应性等混合性致病因素,使临床症状、体征和胸片呈现多种表现。导致ARDS的原因多见于:(1)重症肺炎病原体致病力较强,如金葡菌、肺炎克雷白菌、腺病毒、EB病毒等。(2)恶性病和慢性病患儿存在免疫功能低下和肺部间质病变,进而继发细菌、病毒、真菌和卡氏肺囊虫等感染。(3)在肺炎早期即出现败血症。(4)MODS时,肺成为首先受累的器官,即ALI或ARDS常是MODS动态发展过程中最先表现的状态。 3.亚急性、慢性疾病状态:反复发生肺炎病情复杂 肺炎伴随各种先天性、慢性疾病,如先心病、先天性喉、气管软化症、新生儿期遗留慢性肺疾患、肺血管炎(川崎病、Wegner肉芽肿、狼疮等)。其中先心病最为常见,因其存在肺血多和肺高压的特殊发病
《成人社区获得性肺炎基层诊疗指南(2018年)》发布
推荐理由:成人社区获得性肺炎(CAP)指在医院外罹患的肺实质炎症,包括具有明确潜伏期的病原体感染在入院后于潜伏期内发病的肺炎。CAP是全球第六大死因,在全球所有年龄组都有较高的发病率和死亡率,是医疗卫生资源的主要负担之一。目前国内多项成人CAP流行病学调查结果显示,肺炎支原体和肺炎链球菌是我国成人CAP的重要致病原。中华医学会、中华医学会杂志社、中华医学会全科医学分会、中华医学会呼吸病学分会肺部感染学组共同制定了《成人社区获得性肺炎基层诊疗指南(2018年)》,以期指导临床工作。 我国尚缺乏CAP确切的发病率、病死率和疾病负担数据,成人CAP流行病学数据多来自大城市中心城区的大医院,缺少社区卫生服务中心、乡镇卫生院的流行病学资料。本指南的制定借鉴了国外部分CAP流行病学资料、诊治管理方面的成熟和先进理念,同时结合了我国现有研究资料和临床实践经验。临床表现(1)起病情况:CAP大多呈急性病程,可因病原体、宿主免疫状态和并发症、年龄等不同而有差异。(2)胸部症状:咳嗽是最常见症状,可伴有或不伴有咳痰。细菌感染者常伴有咳痰。铁锈色痰常提示肺炎链球菌感染,砖红色痰常提示肺炎克雷伯菌感染,金黄色脓痰常提示金黄色葡萄球菌感染,黄绿色脓痰常提示铜绿假单胞菌感染。(3)全身症状和肺外症状:发热是最常见的全身症状,常为稽留热或弛张热,可伴有寒战或畏寒。部分危重患者表现为低体温。其他伴随非特异症状包括头痛、乏力、食欲缺乏、腹泻、呕吐、全身不适、肌肉酸痛等。(4)体征:发热患者常呈急性面容,重症患者合并呼吸衰竭时可有呼吸窘迫、发绀,合并感染性休克时可有低血压、四肢末梢湿冷。胸部体征随病变范围、实变程度、是否合并胸腔积液等情况而异。鉴别诊断(1)急性气管-支气管炎:多无呼吸困难、肺部湿啰音,表现较轻。常与病毒性上呼吸道感染有关。胸部影像学检查多正常。(2)肺结核:多有全身中毒症状,如午后低热、盗汗、疲乏无力、体重减轻。病程多呈亚急性或慢性经过。X线胸片或CT见病变多在上叶尖后段或下叶背段,多有卫星灶。痰中可找到结核分枝杆菌。一般抗菌治疗无效。(3)肺癌:多无急性感染中毒症状,有时痰中带血,血白细胞不高。可伴发阻塞性肺炎,经抗生素治疗炎症消退后肿瘤阴影渐趋明显,或可见肺门淋巴结肿大,有时出现肺不张。若抗生素治疗后肺部炎症不见消散,或消散后于同一部位再次出现肺部炎症,应密切随访。(4)肺血栓栓塞症:多有静脉血栓的危险因素,可发生咯血、晕厥,呼吸困难较明显。X线胸片示区域性肺血管纹理减少,有时可见尖端指向肺门的楔形阴影。动脉血气分析常见低氧血症及低碳酸血症。D-二聚体多有升高。治疗(1)抗感染治疗:基层医疗机构CAP治疗需根据病情严重度、治疗场所、年龄、基础疾病等决定初始抗感染药物的使用。(2)其他治疗:除了针对病原体的抗感染治疗外,对于部分患者,氧疗、雾化、化痰、补液、营养支持以及物理治疗等辅助治疗对CAP患者也是必要的。需定时监测患者体温、呼吸频率、脉搏、血压和精神状态情况。疾病管理(1)对于治疗反应迟缓、有基础疾病的患者治疗后可复查胸部影像学。对于高龄CAP患者,需注意心肺并发症及其他并存疾病的治疗和管理。对于症状和影像持续改善不明显,需及时转诊上级医院。(2)戒烟、避免酗酒、保证充足营养、保持口腔健康,有助于预防肺炎的发生。保持良好卫生习惯,有咳嗽、喷嚏等呼吸道症状时戴口罩或用纸巾、肘部衣物遮挡口鼻有助于减少呼吸道感染病原体播散。(3)预防接种肺炎链球菌疫苗可减少特定人群罹患肺炎的风险。目前应用的肺炎链球菌疫苗包括肺炎链球菌多糖疫苗和肺炎链球菌结合疫苗。我国已上市23价肺炎链球菌多糖疫苗,可有效预防侵袭性肺炎链球菌的感染。 ——原文:中华医学会,中华医学会杂志社,中华医学会全科医学分会,等.成人社区获得性肺炎基层诊疗指南(2018年)[J].中华全科医师杂志,2019,18(2):117-126. DOI:10.3760/cma.j.issn.1671-7368.2019.02.005
社区获得性肺炎答案
单项选择题 1. 英国急诊入院病人最常见原因是 A.冠心病 B.脑血管病 C.区获得性肺炎 D.外伤 2. 容易感染耐药肺炎球菌的有 A.65岁以上 B.酗酒 C.患免疫抑制性疾病 D.以上都是 3. 社区获得性肺炎最常见的病原体 A.呼吸道病毒 B.肺炎链球菌 C.军团菌 D.嗜血杆菌 4. 判断社区获得性肺炎病情重的因素有 A.呼吸、脉搏、血压等异常 B.意识的改变 C.体温过高或过低 D.以上都是
5. 下列属于诊断重症肺炎条件之一的是 A.血压〈90/60mmhg B.Pa02〈80 mmhg C.尿量〈80mml/h D.体温390C以上 6. 下列有确诊价值的痰液检测结果是 A.防污染毛刷样本病原菌≥103/ml B.支气管灌洗液标本病原菌≥102/ml C.痰培养优势菌生长≥+++ D.3天内多次培养得到相同细菌 7. 对社区获得性肺炎诊断有确诊价值的检测结果 A.血或脓液培养到病原体 B.经纤支镜或人工气道吸引的标本培养病原菌的浓度≥105/ml (半 定量培养++) C.支气管肺泡灌洗液标本病原菌≥104/ml 半定量培养+--++ D.以上都是 8. 社区获得性肺炎易感染绿脓杆菌的危险因素是 A.广谱抗菌药应用7天以上或长期用激素的病人 B.养老院的老年人 C.酗酒 D.免疫抑制性疾病
9. 对于查不到病原体的社区获得性肺炎老年人,初始经验性治疗多选用 A.第二代头孢菌素 B.大环内酯类、青霉素类 C.第一代头孢菌素 D.强力霉素 10. 延迟送检或待处理的痰标本的应置于多少度保存 A.10度 B.6度 C.4度 D.20度
小儿肺炎的诊断和治疗
小儿肺炎诊疗“攻略” 作者:首都医科大学附属北京安贞医院儿科苏瑛刘桂英 肺炎的分类 肺炎是指不同病原体或其他因素(如吸入羊水、油类或过敏反应)等引起的肺部炎症。主要临床表现为不同程度的发热、咳嗽、气促、呼吸困难和肺部固定性中、细湿啰音。重症患者可累及循环、神经及消化系统而出现相应的临床症状,如心力衰竭、中毒性脑病及中毒性肠麻痹等。常见肺炎分类方法如下。 按病理大叶性肺炎、支气管肺炎和间质性肺炎。 按病因病毒性肺炎、细菌性肺炎、支原体肺炎、衣原体肺炎、非感染病因引起的肺炎等。 按病程急性肺炎(病程<1个月)、迁延性肺炎(病程1~3个月)、慢性肺炎(病程>3个月)。
按病情轻症肺炎、重症肺炎。 按发生肺炎的地区社区获得性肺炎、院内获得性肺炎。 按表现是否典型典型肺炎、非典型肺炎。 临床上如果病原体明确,则按病因分类,有助于指导治疗,否则可按病理或其他方法分类。 支气管肺炎的特点 支气管肺炎是累及支气管壁和肺泡的炎症,为小儿时期最常见的肺炎,2岁以内儿童多发。一年四季均可发病,致病原最常为细菌和病毒,也可由病毒、细菌混合感染。病毒主要有呼吸道合胞病毒、腺病毒、流感及副流感病毒等。细菌感染以肺炎链球菌多见,近年来肺炎支原体、衣原体和流感嗜血杆菌致支气管肺炎发病有增加趋势。病原体常由呼吸道入侵,少数经血行入肺。 病理和病理生理变化 病理变化以肺组织充血、炎性细胞浸润为主。临床上支气管肺炎与间质性肺炎常同时存在。 病理生理变化由于支气管、肺泡炎症引起通气和换气障碍,导致缺氧和二氧化碳潴留。 临床特征 起病多数较急,发病前数日多先有上呼吸道感染,主要临床表现为不同程度的发热、咳嗽、气促、肺部固定性的中、细湿啰音,以及精神不振、食欲减退、烦躁不安,轻度腹泻或呕吐等全身症状。重症肺炎由于严重的缺氧及脓毒血症,除呼吸系统改变外,可发生循环、神经和消化等系统功能障碍。早期合理治疗者并发症少见。若延误诊断或病原体致病力强者可引起并发症,例如脓胸、脓气胸、肺大泡等。
儿童获得肺炎规范
儿童社区获得性肺炎诊疗规范(2019年版) 世界卫生组织资料显示,2016年肺炎造成92万5岁以下儿童死亡,其中98%来自发展中国家。肺炎也是当前我国5岁以下儿童死亡的主要原因之一,其中绝大部分儿童肺炎为社区获得性肺炎(Community Acquired Pneumonia ,CAP)。社区获得性肺炎中的重症难治性支原体肺炎和腺病毒肺炎等遗留的气道闭塞,是造成儿童患慢性气道疾病、影响生命质量的重要原因。近年来,我国CAP 诊疗水平有了长足进步,但在一些地方、一些医疗机构还存在抗生素应用不尽合理、检查方法选择缺乏针对性等问题。鉴于此,国家卫生健康委、国家中医药局组织各相关学科专家,结合我国国情,制定了《儿童社区获得性肺炎诊疗规范(2019年版)》,进一步提高诊疗规范化水平,重点聚焦重症CAP的诊断和高危因素识别,经验性和目标治疗等,以期降低病死率和后遗症发生率。 一、简介 本规范中CAP的定义是指在医院外(社区)发病的感染性肺炎,包括在医院外(社区)感染了具有明确潜伏期的病原体而在入院后发病的肺炎。CAP为肺实质和(或)肺间质部位的急性感染,引起机体不同程度缺氧和感染症状,通常有发热、咳嗽、呼吸增快、肺部湿性啰音等表现,并有胸部
X线片(以下简称胸片)的异常改变。本规范中CAP不包括吸入性以及过敏性等非感染性肺炎。 由于新生儿病原体及临床表现的特殊性,本规范仅针对生后29天到18岁以下儿童的CAP。我国幅员辽阔,地域、经济、文化以及卫生环境等存在较大差异,因此本规范仅为总体原则。 二、主要病原谱和耐药现状 (一)主要病原谱。 1.呼吸道病毒。呼吸道病毒是婴幼儿乃至学龄前期CAP 的常见病原。常见的呼吸道病毒包括呼吸道合胞病毒、流感病毒、腺病毒、副流感病毒和鼻病毒等。新发病毒有人类偏肺病毒、博卡病毒、新型冠状病毒、人禽流感病毒等。其他如巨细胞病毒等疱疹类病毒以及肠道病毒等偶可引起CAP。 2.细菌。常见革兰阳性细菌包括:肺炎链球菌(Streptococcus pneumoniae, SP)、金黄色葡萄球菌(Staphylococcus aureus,SA)、A群链球菌(Group A streptococcus,GAS)等;常见革兰阴性细菌包括:流感嗜血杆菌(Haemophilus influenzae,Hi)、卡他莫拉菌(Moraxella catarrhalis,MC)、大肠埃希菌(Escherichia coli,E.coli)、肺炎克雷伯菌(Klebsiella pneumoniae,KP)、铜绿假单胞菌(Pseudomonas aeruginosa)等。其中SP是生后20天至儿童期各年龄段CAP最常见的病原,也是重症肺炎和坏死性肺炎的最常见病原。SA多感染婴幼
社区获得性肺炎诊疗常规
社区获得性肺炎诊疗常规诊断】 一、临床表现。 (一)典型表现 1.大多数起病前常有上呼吸道感染史,常有受寒、劳累诱因,老年人肺炎或有肺或全身基础疾病的肺炎起病隐匿、表现不典型。 2.发热。 3.咳嗽、咯痰:早期为干咳,渐转有痰,痰多脓性,咯血少见,肺炎链球菌肺炎为铁锈色痰。 4.胸痛:病变累及胸膜时则呈针刺样痛;下叶肺炎刺激隔胸膜疼痛可放射至肩部或腹部。 5.全身症状:头痛、肌肉酸痛,乏力,或有恶心,呕吐,腹胀,腹泻,重症患者可有嗜睡、意识障碍。惊厥等。 (二)体检1.急性病容,呼吸浅速,可有鼻翼扇动。不同程度的紫绀和心动过速。重症可出现感染性休克。 2.肺炎链球菌性肺炎常有口唇单纯疱疹。 3.早期胸部无异常体征或仅湿罗音,随疾病发展出现患侧呼吸运动减弱,叩诊浊音、呼吸音降低、管状音和湿性罗音。老年人肺炎。革兰阴性杆菌肺炎和慢性支气管炎继发肺炎,多同时累及双肺,双下肺可闻及湿罗音。 二、检查 (一)血白细胞总数和中性粒细胞多升高。 (二)痰涂片镜检及培养有助病原诊断(见第十一节医院获得性肺炎)。 (三)免疫学和分子生物学方法可用于军团菌和支原体诊断。 (四)胸部X线检查1.肺炎球菌性肺炎多表现为叶、节段片状阴影。 2.葡萄球菌肺炎常为肺多发性类圆形阴影,或空洞形成。 3革兰阴性杆菌、病毒性、支原体性肺炎常呈支气管肺炎型且易形成多发性小腔。 三、诊断标准 (一)新近出现的咳嗽,咳痰,或在原有咳嗽、咯痰的基础上症状加重,出现脓性痰。(二)发热。 (三)体检发现肺实变体征或出现湿性罗音。 (四)WBC>10.0xl09,或<4.0xl09,伴或不伴核左移。 (五)胸透或胸片出现片状,斑片状影像或问质改变,伴或不伴胸腔积液;除外了肺结核、以及肺栓塞、肺水肿、肺部肿瘤、某些非感染性间质性肺炎、Wegener肉芽肿。肺嗜酸性粒细胞浸润症等非感染性疾病。以上1、2、3,4任一种情况加上5可诊断为肺炎。若符合社区获得性肺炎的定义可诊断。 【治疗】一、对症治疗可吸氧,化痰止咳、输液,有休克者抗休克。二、抗菌治疗先经验治疗,对可能的病原菌选择敏感抗生素,2~3大后视病情,必要时改换抗生素,并依病原菌资料选药。肺炎链球菌:首选青霉素G;次选大环内酯类,林可霉素、一代头孢和氟喹诺酮类。耐青霉素者用二,三代头抱菌素。流感嗜血杆菌:首选氨苄西林;其次选阿莫西林,产酶菌可用二,三代头孢菌素。舒他西林,阿莫西林/棒酸,氧氟沙星。葡萄球菌:用青霉素G,一代头孢菌素,克林霉素,红霉素等大环内酯类。产酶的可用舒他西林、阿莫西林准酸或青霉素合用氨基糖苷类,耐甲氧西林的金黄色葡萄球菌和表皮葡萄球菌可选万古霉素或替考拉宁。肺炎克雷伯杆菌、大肠杆菌:首选氨基糖苷类加哌拉西林;次选二、三代头抱,氟喹诺酮类,舒他西林。军团菌:首选大环内酯类,如红霉素(一般静脉给药),合用利福平或多西环素。支原体、衣原体:大环内酯类;氟喹诺酮类。病毒性:可用抗病毒药,如病毒唑等。肺炎疗程一般7~14天,金葡菌肺炎、军团菌肺炎、免疫抑制患者肺炎,疗程宜延长。 【疗效标准】一、治愈症状体征及胸部调线阴影全部消失。二、好转症状消失或减轻,胸部调线阴影部分吸收,诱因尚未解除。三、未愈症状体征和胸部调线均无好转。
社区获得性肺炎
社区获得性肺炎(community-acquired pneumonia,CAP) 社区获得性肺炎是指在医院外罹患的感染性肺实质(含肺泡壁,即广义上的肺间质)炎症,包括具有明确潜伏期的病原体感染在入院后于潜伏期内发病的肺炎。 【病原学】 目前国内多项成人CAP的流行病学调查结果显示:肺炎支原体和肺炎链球菌是我国成人CAP的重要致病原。其他常见病原体包括流感嗜血杆菌、肺炎衣原体、肺炎克雷伯菌即金黄色葡萄球菌,但铜绿假单胞菌及鲍曼不动杆菌少见。对于特殊人群如高龄或存在基础疾病的患者(如心脑血管疾病、慢性呼系统疾病、充血性心力衰竭、肾功能衰竭、糖尿病等),肺炎克雷伯菌及大肠埃希菌等革兰氏阴性菌更常见。另外,我国成人CAP中病毒检出率为15-34.9%,流感病毒占首位,病毒检测阳性患者中5.8%-65.7%可合并细菌或非典型病原体感染。在病原体耐药方面,我国肺炎链球菌对大环内酯类药物的耐药率为63.2-75.4%,肺炎支原体对大环内酯类药物耐药率高,对多西环素或米诺环素、喹诺酮类抗菌药物敏感。 【流行病学】 CAP对所有年龄段人群均有影响,在>65岁的老年人发病率大于青壮年。不同年龄人群的主要病原体无明显差异。CAP的高危因素有:慢性心、肺、肝、肾等疾病,脑血管疾病,自身免疫性疾病,糖尿病及免疫抑制状态等。合并其他疾病的老年人预后差。 【临床表现】 1.CAP多呈急性起病。 2.咳嗽是最常见症状,大多伴有咳痰、呼吸困难。典型的痰液表现有助于诊断。 3.大多数有发热和寒战,乏力很常见,可有出汗、头痛、肌肉酸痛、厌食等其他症状。 4.体征可有呼吸急促、发绀。胸部查体可有患侧呼吸动度减弱、触觉语颤增强、叩诊浊音、听诊闻及湿啰音。 【辅助检查】 1.白细胞计数:外周白细胞计数升高。 2.c反应蛋白及降钙素原PCT升高。 3.血氧:动脉氧分压和氧合指数是评估并且的基本参数。 4.影像学检查:胸部X线是基本检查,胸部CT敏感性更高。影像学显示出新的斑片状浸润影、叶/段实变影、磨玻璃影或间质性改变有助于确诊。 【诊断标准】 CAP的诊断标准:符合1,3及2中的任何一项,并除外肺结核、肺部肿瘤、非感染性肺间质疾病、肺水肿、肺不张、肺栓塞、肺嗜酸性粒细胞浸润症及肺血管炎等后,可建立临床诊断。 1.社区发病; 2.肺炎相关临床表现:①新近出现的咳嗽、咳痰或原有呼吸道疾病症状加重,伴或不伴脓胸/胸痛/呼吸困难/咯血;②发热;③肺实变体征和(或)闻及湿性啰音;④外周血白细胞>10?109/L,或<4,伴或不伴细胞核左移。 3.肺部影像学检查显示出新的斑片状浸润影、叶/段实变影、磨玻璃影或间质性改变,伴或不伴胸腔积液。 重症CAP的诊断标准:符合下列1项主要标准或≥3项次要标准者可诊断为重症肺炎。 主要标准:①需要气管插管行机械通气治疗;②脓毒症休克经积极液体复苏后仍需要血管活性药物治疗。 次要标准:①呼吸频率≥30次/min;②氧合指数≤250mmHg;③多肺叶浸润;④意识障碍和(或)定向障碍;⑤血尿素氮≥7.4mmol/L;⑥收缩压<90mmHg需积极液体复苏。 【治疗】 1.抗感染治疗 CAP诊断后尽早进行经验性抗感染治疗以降低病死率,缩短住院时间。根据48-72小时治疗后反应并结合病原学结果调整治疗方案。不同人群的初始经验性抗感染治疗不同,见下表1。 2.辅助治疗:除抗感染治疗外,补液、维持水电解质平衡、营养支持以及物理治疗也是必要的。对于低氧血症患者,要给予鼻导管或面罩氧疗,维持血氧饱和度90%以上。无创通气能降低急性呼衰CAP患者的气管插管率和病死率。糖皮质激素能降低合并感染性休克CAP患者的病死率,推荐琥珀酸氢化可的松200mg/d,感染性休克纠正后立即停药,一般用药不超过7d。 【预防】 戒烟、避免酗酒有助于预防肺炎的发生。预防接种肺炎链球菌疫苗可减少特定人群的发病。
1、儿童社区获得性肺炎诊疗指南
沙坪坝区人民医院儿科 儿童社区获得性肺炎诊疗规范 【概述】 社区获得性肺炎是指原本健康的儿童在医院外获得的感染性肺炎,包括感染了具有明确潜伏期的病原体而在入院后潜伏期内发病的肺炎,是相对于医院获得性肺炎而言。是婴幼儿时期重要的常见病、多发病,是儿童住院的常见原因。年幼儿50%由病毒引起,年长儿由细菌、支原体感染为主。 【病史要点】 1、询问发热、咳嗽、气促、发绀及并发症的发展变化过程,了解发热程度、热型,咳嗽轻重,有无痰响、吼喘及进食呛咳。 2、询问病后精神状态,有无烦躁、呻吟、萎靡、嗜睡和惊厥;食欲的改变、进食减少程度,有无呕吐、腹泻。 3、院外诊断、重要检查和治疗情况,特别是所用抗生素种类及疗程。 4、病前有无上呼吸道感染、流感、麻疹、百日咳等传染病史及接触史,既往预防接种史。 【体检要点】 1、测量体温、呼吸、心率,注意营养发育状况,精神、神志状态。 2、呼吸困难情况,有无喘憋、鼻扇、呻吟、点头样呼吸、胸壁吸气性凹陷,有无口周、甲床青紫,面色青灰或苍白;小婴儿尚须注意有无呼吸节律异常。 3、肺部体征:肺部有无中细湿罗音及语颤增强、叩浊等肺部实变体征。 4、是否有呼吸衰竭、心功能不全及其它脏器功能受累而出现的体征:注意心音强弱、心率和心律;有无腹胀,肝脏大小、质地及压痛,脾脏大小;有无下肢水肿。 5、注意有无皮肤化脓性感染灶及合并的气胸、脓气胸体征(提示金
葡菌感染)。 【辅助检查】 血常规、CRP、血沉、降钙素原、ASO,尿肺炎链球菌抗原,肺炎支原体抗体、肺炎衣原体抗体,呼吸道常见病毒检测,痰液、气管吸出物、胸腔穿刺液等体液行细菌培养和药敏试验,拟诊细菌感染、病情严重或有并发症的患儿应做血培养,阳性者,治疗后应复查;心肌酶谱、肝肾功能、电解质、大便常规(3岁以下查轮状病毒抗原)、尿常规,危重病例应作血气分析,所有住院肺炎或疑似低氧血症者,均需监测血氧饱和度。胸部X 线检查,(必要时CT)。 【诊断标准】 肺炎有发热、咳嗽,呼吸频率增快(<2月,呼吸≥60次/分;2-12月,呼吸≥50次/分;1-5岁,呼吸≥40次/分;≥5岁,呼吸≥30次/分),胸壁吸气性凹陷,呼吸困难,喘鸣,肺部湿性罗音等临床表现,结合胸部X 线检查结果,可作出诊断。 WHO推荐,2月-5岁儿童出现胸壁吸气性凹陷或鼻翼扇或呻吟之一表现者,提示有低氧血症,考虑为重度肺炎;如出现中心性紫绀、严重呼吸窘迫、拒食或脱水症、意识障碍(嗜睡、昏迷、惊厥)之一表现者,为极重度肺炎。动重度肺炎征象:激惹或嗜睡、拒食、呼吸急促(婴幼儿<2月,呼吸≥60次/分;2-12月,呼吸≥50次/分;1-5岁以下,呼吸≥40次/分)、下胸壁凹陷及紫绀。 并发症:肺部并发症包括胸腔积液、脓胸、脓气胸、肺脓肿、支气管胸膜瘘、坏死性肺炎、呼吸衰竭等;肺外并发症包括脑膜炎、脑脓肿、心包炎、心内膜炎、骨髓炎、关节炎、脓毒症、溶血尿毒症综合征等。 鉴别诊断:急性支气管炎、肺结核、支气管异物等。 【治疗方案及原则】 1、一般治疗:保持室内空气流通,保证足够入量,不能进食者静脉补液,总液体量为基础代谢正常需要量的80%,1/4-1/5张液体24小时匀速滴注,速度<5ml/kg.h;有中度以上脱水者,不也总量可按脱水分度推荐
(完整word版)儿童单病种社区获得性肺炎肺炎考试题及答案
儿科单病种社区获得性肺炎考试题及答案姓名成绩 一,问答题 1.儿童住院社区获得性肺炎的诊断依据: 2.儿童住院社区获得性肺炎入院后1-3天必需检查项目:
3.儿童住院社区获得性肺炎的治愈出院标准 4.儿童住院社区获得性肺炎的除外病例 二,填空题: 1.标准住院日(7-14 )天 2.初始治疗第(1-3 )天进行临床评估,根据患者病情变化调整抗菌药物。 3.入院后1-3天除了必需检查项目外还可以根据患者情况进行:(血培养)、(胸部CT )、(D-二聚体)、(B超)等。 4.对症支持治疗包括(吸氧)、(退热)、(止咳化痰),(平喘)
参考答案 1).儿童住院社区获得性肺炎的诊断依据: 1. 咳嗽、咳痰,或原有呼吸道疾病症状加重,并出现脓性痰,伴或不伴胸痛; 2. 发热; 3. 肺实变体征和(或)闻及湿性啰音; 4. 白细胞数量>10×109/L或<4×109/L,伴或不伴细胞核左移; 5. 胸部影像学检查显示片状、斑片状浸润性阴影或间质性改变。 以上1-4项中任何1项加第5项,并除外肺部其他疾病后,可明确临床诊断2)儿童住院社区获得性肺炎入院后1-3天必需检查项目: 1)血常规、尿常规、便常规 (2)肝肾功能、血糖、电解质、血沉、C反应蛋白(CPR)、血气分析、感染性疾病筛查(乙肝、丙肝、梅毒、艾滋病等) (3)病原学检查(支原体抗体、病毒筛查、军团菌抗体、结核抗体)痰涂片、痰培养及药敏 (4)胸正侧位片、心电图 3)儿童住院社区获得性肺炎的治愈出院标准 治愈标准: 1、症状和体征完全消失 2、检查肺部炎症性阴影吸收 3、痰培养阴性 出院标准:
1.症状好转,体温正常超过72小时; 2.生命征平稳,可以接受口服药物治疗; 3.肺部病灶基本吸收,血常规基本正常。 4)儿童住院社区获得性肺炎的除外病例 1.年龄大于18岁的病例 2.由外院住院诊疗后转入本院 3.参与临床药物与器械试验 4.肺炎反复门诊抗生素治疗无效 5.同一疾病30日内重复入院 6.呼吸机相关性肺炎 7.医院获得性肺炎 8.新生儿支气管肺炎 9.婴儿喘息性支气管肺炎10.婴儿支气管肺炎11.本次住院时间超过60天的。
儿童社区获得性肺炎诊疗规范(2019版)
儿童社区获得性肺炎诊疗规范 (2019年版) 世界卫生组织资料显示,2016年肺炎造成92万5岁以下儿童死亡,其中98%来自发展中国家。肺炎也是当前我国5岁以下儿童死亡的主要原因之一,其中绝大部分儿童肺炎为社区获得性肺炎(Community Acquired Pneumonia,CAP)。社区获得性肺炎中的重症难治性支原体肺炎和腺病毒肺炎等遗留的气道闭塞,是造成儿童患慢性气道疾病、影响生命质量的重要原因。近年来,我国CAP诊疗水平有了长足进步,但在一些地方、一些医疗机构还存在抗生素应用不尽合理、检查方法选择缺乏针对性等问题。鉴于此,国家卫生健康委、国家中医药局组织各相关学科专家,结合我国国情,制定了《儿童社区获得性肺炎诊疗规范(2019年版)》,进一步提高诊疗规范化水平,重点聚焦重症CAP的诊断和高危因素识别,经验性和目标治疗等,以期降低病死率和后遗症发生率。 一、简介 本规范中CAP的定义是指在医院外(社区)发病的感染性肺炎,包括在医院外(社区)感染了具有明确潜伏期的病原体而在入院后发病的肺炎。CAP为肺实质和(或)肺间质部位的急性感染,引起机体不同程度缺氧和感染症状,通常有发热、咳嗽、呼吸增快、肺部湿性啰音等表现,并有胸部X线片(以下简称胸片)的异常改变。本规范中CAP不包括吸入性以及过敏性等非感染性肺炎。 由于新生儿病原体及临床表现的特殊性,本规范仅针对生后29天到18岁以下儿童的CAP。我国幅员辽阔,地域、经济、文化以及卫生环境等存在较大差异,因此本规范仅为总体原则。 二、主要病原谱和耐药现状 (一)主要病原谱。
1.呼吸道病毒。呼吸道病毒是婴幼儿乃至学龄前期CAP的常见病原。常见的呼吸道病毒包括呼吸道合胞病毒、流感病毒、腺病毒、副流感病毒和鼻病毒等。新发病毒有人类偏肺病毒、博卡病毒、新型冠状病毒、人禽流感病毒等。其他如巨细胞病毒等疱疹类病毒以及肠道病毒等偶可引起CAP。 2.细菌。常见革兰阳性细菌包括:肺炎链球菌(Streptococcus pneumoniae,SP)、金黄色葡萄球菌(Staphylococcus aureus,SA)、A群链球菌(Group A streptococcus,GAS)等;常见革兰阴性细菌包括:流感嗜血杆菌(Haemophilus influenzae,Hi)、卡他莫拉菌(Moraxella catarrhalis,MC)、大肠埃希菌(Escherichia coli,E.coli)、肺炎克雷伯菌(Klebsiella pneumoniae,KP)、铜绿假单胞菌(Pseudomonas aeruginosa)等。其中SP是生后20天至儿童期各年龄段CAP最常见的病原,也是重症肺炎和坏死性肺炎的最常见病原。SA多感染婴幼儿,分甲氧西林敏感金黄色葡萄球菌(Methicillin-sensitive staphylococcus aureus,MSSA)和耐甲氧西林金黄色葡萄球菌(Methicillin-resistant staphylococcus aureus,MRSA),MSSA和MRSA均可引起重症肺炎或坏死性肺炎,我国也有儿童社区获得性MRSA(CA-MRSA)肺炎报道,该菌感染病死率较高。GAS肺炎多为重症肺炎或坏死性肺炎。Hi肺炎多见于5岁以下儿童,MC肺炎多见于婴幼儿,一般不引起重症CAP。E.coli和KP虽不是CAP的常见病原,但可引起重症肺炎,多见于婴儿,或有慢性吸入、先天性心脏病、气道畸形、免疫功能低下、重症病毒感染等基础疾病者。 3.非典型微生物。肺炎支原体(Mycoplasma pneumoniae,MP)不仅是学龄前期和学龄期儿童CAP的常见病原,近年来在1~3岁婴幼儿亦不少见。肺炎衣原体(Chlamydia penumoniae,CP)多见于学龄期和青少年,但在我国肺炎衣原体独立引起的肺炎较少报道。沙眼衣
(完整版)考试题(呼吸系统)(含答案)
(呼吸系统一) 考试题 姓名考试时间120分钟得分 一、单择题(每一题1分,共50分) 1、慢性阻塞性肺疾病急性发作最常见的原因是()E A、空气污染 B、接触香烟烟雾 C、接触过敏原 D、气候变化 E、感染 2、男,70岁。因咳嗽、咳痰30年,气短5年,近期加重前来体检。胸部X线片示双肺透光度增加。其胸部査体最可能出现的体征是( D ) A、语颤增强 B.呼吸音增强 C、叩诊实音 D、叩诊过清音 E.三凹征 3、男,66岁。活动后突发左侧胸痛伴呼吸困难1天。既往慢性阻塞性肺疾病病x ^ 10余年。査体:R26次/分,BP95/60nunHg。口唇发绀,左肺呼吸音明显减弱,心率102次/分,律齐。 3.1、该患者最可能的诊断是(B ) A、急性心肌梗死 B、自发性气胸 C、阻塞性肺不张 D、胸腔积液 E、肺栓塞 3.2、为明确诊断,应先采取的检查措施是( B) A、CT肺动脉造影 B、胸腔穿刺 C、支气管镜 D、胸部X线片 E、电心图 4、对年老体弱、痰堡较多且无力咳痰的慢性支气管炎患者,不宜使用的药物为( E ) A、氧氟沙星 B、溴己新 C、羧甲司坦 D、氨溴索 E、可待因 5、以反复发作性干咳、胸闷为主要症状的疾病是( A ) A、支气管哮喘 B、支气管异物 C、支气管肺炎 D、支气管结核 E、支气管肺癌 6、支气管哮喘发作时,最有诊断意义的体征是( E) A、胸廓饱满 B、肋间隙增宽 C、触诊胸部语颤减弱 D、叩诊胸部过清音 E、听诊两肺广泛哮鸣音 7、提示支气管哮喘患者病情危重的是(D ) A、呼气相延长 B、脉压增加 C、呼吸性碱中毒 D、胸腹矛盾运动 E、烦躁不安 8、冠心病患者伴发支气管哮喘时危慎用哪种药物?(C ) A、氨茶碱 B、肾上腺糖皮质激素 C、肾上腺素 D 、酮替酚 E、色甘酸二钠 9、当支气管哮喘患者发作时禁用的药物是(C ) A、肾上腺素 B、氨茶碱 C、吗啡 D、沙丁胺醇 E、泼尼松 10、当支气管哮喘与心源性哮喘一时难以鉴别时,为缓解症状,可采用的药物是(C ) A、呋塞米(速尿) B、吗啡或哌替啶(度冷丁) C、氨茶碱 D、毛花苷丙(西地兰) E、肾上腺素 11、支气管扩张症最有意义的体是(C ) A、贫血 B、杵状指以 C、固定的局限性湿啰音 D、消瘦 E、多变的哮鸣音 11、支气管扩张的典型痰液表现为(B ) A、大量白色泡沫痰 B、大量脓性痰,有分层 C、大量粉红色泡沫痰 D、大量乳状痰 E、大量白色黏液状痰 12.1、女性,25岁。2天前咳血痰,今日咯血量达200ml左右。既往身体健康。体检:T37.0度,右肩胛下少量细小啰音,心尖部2级柔和收缩期杂音。X线胸片无异常发现。此病人首选止血药物是(A) A、垂体后叶素 B、 6-氨基己酸 C、立止血(巴曲酶) D、氨基甲酸 E、安络血 12.2、若需作体位引流,病人应取(B) A、半卧位 B、头低足高左侧卧位 C、头低足高右侧卧位 D、俯卧位 E、仰卧位
社区获得性肺炎诊断和治疗指南(中华医学会呼吸病学分会)
社区获得性肺炎诊断和治疗指南 中华医学会呼吸病学分会 社区获得性肺炎(community-acquired pneumonia,CAP)是指在医院外罹患的感染性肺实质(含肺泡壁,即广义上的肺间质)炎症,包括具有明确潜伏期的病原体感染而在入院后潜伏期内发病的肺炎。CAP是威胁人类健康的常见感染性疾病之一,其致病原的组成和耐药特性在不同国家、不同地区之间存在着明显差异,而且随着时间的推移而不断变迁。近年来,由于社会人口的老龄化、免疫损害宿主增加、病原体变迁和抗生素耐药率上升等原因,CAP 的诊治面临许多新问题。最近,中华医学会呼吸病学分会完成了两项较大样本的全国性CAP 流行病学调查,在此基础上,结合国外CAP诊治方面的最新研究进展,对1999年制定的《社区获得性肺炎诊断和治疗指南(草案))进行了适当修改,旨在指导临床建立可靠的诊断,全面评估病情,确定处理方针,改善预后,尽量避免不恰当的经验性治疗,减少抗生素选择的压力,延缓耐药,节约医药卫生资源。 一、CAP的临床诊断依据 1.新近出现的咳嗽、咳痰或原有呼吸道疾病症状加重,并出现脓性痰,伴或不伴胸痛。 2.发热。 3.肺实变体征和(或)闻及湿性啰音。 4.WBC>10×109/L或<4×109/L,伴或不伴细胞核左移。 5.胸部X线检查显示片状、斑片状浸润性阴影或间质性改变,伴或不伴胸腔积液。 以上1~4项中任何1项加第5项,并除外肺结核、肺部肿瘤、非感染性肺间质性疾病、肺水肿、肺不张、肺栓塞、肺嗜酸性粒细胞浸润症及肺血管炎等后,可建立临床诊断。 二、CAP的病原学诊断 1.病原体检测标本和方法:见表1。 表1 社区获得性肺炎主要病原体检测标本和方法 病原体标本来源显微镜检查培养血清学其他 需氧菌和兼性厌氧 菌痰液、经纤维支气管镜或人工气道吸 引的下呼吸道标本、BALF、经PSB 采集的下呼吸道标本、血液、胸腔积 液、肺活肺活检标本、尿液 革兰染色+ - 免疫层析法检测肺 炎链球菌抗原(针对 成人肺炎链球菌感 染的快速诊断方法) 厌氧菌经纤维支气管镜或人工气道吸引的 下呼吸道标本、BALF、经PSB采集的 下呼吸道标本、血液、胸腔积液 革兰染色+ - 分枝杆菌痰液、经纤维支气管镜或人工气道吸 引的下呼吸道标本、BALF、经PSB 采集的下呼吸道标本、肺活检标本 萋尼染色+ + PPD试验、组织病理 军团菌属痰液、肺活检标本、胸腔积液、经纤 维支气管镜或人工气道吸引的下呼 吸道标本、BALF、经PSB采集的下呼 吸道标本、双份血清、尿液 FA(嗜肺军团 菌) + IFA、EIA 尿抗原(主要针对嗜 肺军团菌Ⅰ型) 衣原体属鼻咽拭子、双份血清-+(有条 件时) 肺炎衣原体 MIF、CF、EIA 鼻咽拭子的PCR仅限 于临床研究
社区获得性肺炎
社区获得性肺炎 社区获得性肺炎:是指在院外由细菌、病毒、衣原体和支原体等多种微生物所引起的。主要临床症状是咳嗽、伴或不伴咳痰和胸疼。 社区获得性肺炎病原体: 主要涉及细菌、支原体、衣原体和病毒4大类。细菌最常见。 社区获得性肺炎的病毒病原有甲、乙型流感病毒,1、2、3型类流感病毒,呼吸道合胞病毒和腺病毒等。其他微生物病原有肺炎支原体、肺炎衣原体和鹦鹉热衣原体等。 就细菌病原来说,社区获得性肺炎,除结核杆菌和军团菌可直接通过飞沫将菌吸入到肺实质,假单胞菌可直接定居于气管外,其余均为通过吸入来自自体咽喉部的感染因子而获得的。临床较为常见的社区获得性肺炎的细菌病原是肺炎链球菌、结核分枝杆菌、流感嗜血杆菌、金黄色葡萄球菌、军团菌、克雷伯杆氏菌和卡他摩拉克菌等。 就细菌而言,社区获得性肺炎与医院内获得性肺炎相反,主要是由革兰阳性菌所致,其中以肺炎链球菌最为常见,其阳性率占已知病原的40%~60%,其次为结核杆菌及金黄色葡萄球菌。 80%的病源为单一致病菌,20%存在两种或两种以上致病菌,少数结核病人可检查到多种病原体,这可能表明原来的共生菌在结核病人身上可能成为致病菌。 重型社区获得性肺炎患者多发生在60岁以上者且多具某些基础疾病如糖尿病,慢性阻塞性肺疾患,这些患者则有较大比例(20%~30%)的病源为革兰阴性杆菌。而在青年人群中,院外细菌性肺炎的致病菌则不同,大部分以革兰阳性菌感染为主。 少部分患者为:无病原学依据,约占30%~50%,其原因可能是由于在入院前使用过抗生素治疗或是由于所用检测手段不完备所致。 临床表现: 1. 前驱症状:相当一部分病人有明确的受凉或过度疲劳的诱因,其前驱症状主要有鼻炎样症状或上呼吸 道感染的症状,如鼻塞、鼻流清涕、喷嚏、咽干、咽痛、咽部异物感、声音嘶哑、头痛、头昏、眼睛热胀、流泪及轻度咳嗽等。并非每一个社区获得性肺炎患者都会有前驱症状,其发生率依病原体不同一般在30%~65%之间。 2.全身毒血症 绝大多数社区获得性肺炎患者都会不同程度地出现全身毒血症样症状,如畏寒、寒战、发热、头昏、头痛、全身肌肉和关节酸痛、体乏、饮食不佳、恶心、呕吐;重症患者还可出现神志障碍或精神症状。 3.呼吸系统症状 即咳嗽、咳痰、咯血、胸痛、呼吸困难五大症状。并非每一个患者或每一种病原体所致的肺炎都会同时出现以上五大症状。如支原体肺炎常表现为干性呛咳,重者伴胸骨后疼痛;病毒性和浆细胞性肺炎咳嗽可逐渐加重,但胸痛和气促较少见,年轻人发作时常表现为典型的急性症状,而老年或重症患者咳嗽、咳痰较少,甚至常无明显呼吸道症状,免疫缺陷患者肺炎发病早期可仅表现为呼吸频率增快、发热、不安,也可无明显呼吸道症状。典型的肺炎链球菌肺炎可咳铁锈色痰,葡萄球菌肺炎时有咳脓血痰,克雷白杆菌肺炎患者咳痰可呈砖红色,铜绿假单胞菌肺炎脓痰中可带淡绿色,厌氧菌肺炎患者可咳脓性恶臭痰。抗生素的广泛应用,临床上所见的社区获得性肺炎患者在呼吸道症状表现上以轻型或不典型者为多。 4.肺外症状
