transobturator-tape

ORIGINAL ARTICLE
Prospective comparison of the‘inside–out’
and‘outside–in’transobturator-tape procedures
for the treatment of female stress urinary incontinence Kyu-Sung Lee&Myung-Soo Choo&Young Sook Lee&
Ji-Yeon Han&Ji-Yoon Kim&Byung Joo Jung&
Deok Hyun Han
Received:5June2007/Accepted:27September2007/Published online:17October2007
#International Urogynecology Journal2007
Abstract The aim of this study was to prospectively compare the efficacy and safety of‘inside–out’(TVT-O) and‘outside–in’(TOT)transobturator tape procedures for treatment of female stress urinary incontinence(SUI).One hundred women with SUI were alternately assigned to TVT-O(n=50)or TOT(n=50).About1year after surgery, we compared surgical outcomes in the two https://www.360docs.net/doc/8c13220818.html,T-O and TOT showed similar rates of cure(86vs92%). Approximately1year after surgery,Incontinence Quality of Life questionnaire parameters improved significantly in both groups(p<0.05),but the two groups did not differ(p> 0.05).The rates of patient satisfaction with TVT-O and TOT(96vs98%)were similar.These preliminary results suggest that TVT-O and TOT are equally effective and safe procedures for women with SUI.However,this study was unable to identify a difference between the two procedures due to the underpowered nature of the study.
Keywords Quality of life.Stress urinary incontinence. Prostheses and implants.Tension-free vaginal tape Introduction
Stress urinary incontinence(SUI)is defined as the involun-tary loss of urine associated with activities that increase intra-abdominal pressure,such as coughing,sneezing,laughing, squatting,or performing the Valsalva maneuver[1].Similar to its frequency in Western countries,about37.8%of Korean adult women suffer from SUI[2],which can be a cause of significant social embarrassment and may lead to negative changes in lifestyles and self-esteem.
The surgical treatment of female SUI caused by urethral hypermobility was altered by the description of midurethral support without tension[3,4],leading to the development of a new surgical approach,called tension-free vaginal tape (TVT),which has resulted in significant short-and long-term cure rates[5–8].This method,however,is associated with perioperative complications,including bowel,vascu-lar,and bladder injuries[6–8],with most complications shown to be related to the blind passage of the trocars in the retropubic space.
An alternative technique,the transobturator midurethral sling procedure,has been developed to minimize the complications of TVT.In this procedure,the tape is introduced through the obturator foramen from the outside to the inside[9].This method results in high short-term cure rates,similar to those achieved with TVT,but fewer complications such as bladder perforation[9–11].More recently,an‘inside–out’transobturator urethral sling(TVT-O) was developed,in which the tape is passed through the obturator foramen from the inside to outside[12].
Comparative studies of the transobturator midurethral sling procedure and TVT have reported similar efficacy for female SUI[13–15].To our knowledge,the efficacy and safety of the‘inside–out’(TVT-O)and‘outside–in’(TOT)
Int Urogynecol J(2008)19:577–582
DOI10.1007/s00192-007-0487-5
K.-S.Lee
:Y.S.Lee:B.J.Jung:D.H.Han Department of Urology,Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul,South Korea
K.-S.Lee
e-mail:ksleedr@https://www.360docs.net/doc/8c13220818.html,
M.-S.Choo(*)
:J.-Y.Han:J.-Y.Kim Department of Urology,Asan Medical Center, University of Ulsan College of Medicine,
388-1Pungnap-dong,Songpa-gu,
Seoul138-736,South Korea
e-mail:mschoo@amc.seoul.kr
transobturator tape procedures have not been compared for the treatment of female SUI.We therefore prospectively compared the efficacy and safety of TVT-O and TOT with a minimum follow-up of1year.
Materials and methods
Subjects
From May2004to May2005,100female patients with urodynamically determined SUI were enrolled in this study. Patients with predominant urge incontinence or pelvic organ prolapse were excluded.Preoperative work-up included a medical history,physical examination,urinaly-sis,urodynamic evaluation,and Incontinence Quality of Life(I-QoL)questionnaire.The I-QoL,which evaluates the effect of SUI on everyday life,has been found to be valid and reliable internationally[16,17].Our study used the validated Korean version of the I-QoL[18].
All participants provided written informed consent after the study protocol had been approved by the institutional review board.
Surgical procedure
Patients were alternately assigned to undergo TVT-O(n= 50;Gynecare,Somerville,NJ,USA)or TOT(n=50; TOT?,Dow Medics,Korea),as described previously[9, 12].Both procedures were performed by two experienced surgeons at the Samsung Medical Center and Asan Medical Center.Cystoscopy was performed on all patients with TOT.Surgical parameters measured included procedure duration,volume of intraoperative bleeding,severity of pain after surgery using a visual analogue scale,and postvoid residual volume.Patients with poor bladder emptying(i.e.,>100ml postvoid residual volume)were discharged with a urethral catheter and returned on the following day to have the catheter removed and to undergo measurements of flow rate and postvoid residual volume. Subject follow-up
Patients were evaluated1week and1month postopera-tively for pain associated with surgery and time to return to normal activity.At1-year follow-up,patients were evalu-ated for surgical results,patient satisfaction,I-QoL ques-tionnaire,long-term complications,urinary flow rate,and postvoid residual volume.Surgical outcomes were eval-uated by the cough stress test with a comfortably full bladder and symptom questionnaire and scored as cured, improved,or failed.Patients were considered‘cured’of SUI if they had a negative cough stress test result and there were no reports of urine leakage during stress.Patients were considered‘improved’if they did not leak on the cough stress test but may have had occasional urine leakage during stress;this occasional leakage did not influence their daily activities or require further treatment.Patients who did not meet these criteria were considered to have‘failed’treatment.Patients were asked to describe their overall satisfaction with surgical outcome as“very satisfied”,“satisfied”,or“not satisfied”,with the first two groups considered as satisfied.Patients were also asked if they would have the same procedure again if their SUI recurred and if they would recommend the procedure to other patients.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences12.0(SPSS,Chicago,IL, USA)program for Windows?(Microsoft Corporation, Seattle,WA,USA),with Student’s t test and a paired t test used to compare parametric continuous variables.Statistical significance was defined as p<0.05.
Results
There were no significant differences in the preoperative characteristics of patients who underwent TVT-O or TOT (Table1).We also found that operation time,mean prolene mesh length,intraoperative bleeding,postoperative pain, postvoid residual volume,wound discomfort,and time to normal activity did not differ significantly between the two groups(Table2).After surgery,8patients in the TVT-O group and12in the TOT group required a urethral catheter on the first day;following removal of the catheter on the next day,however,all voided well.About7patients(14%) in the TVT-O group and9(18%)in the TOT group complained of postoperative inner thigh or buttock discom-fort,but all of these transient symptoms of discomfort disappeared in all patients at1-month follow-up.There were no serious perioperative complications in either group, such as bladder perforation,infection,or significant nerve or vessel injury.
Surgical results for SUI were similar in both groups (Table3).The cure rates were86%in the TVT-O group and 92%in the TOT group.Seven patients in the TVT-O group and12in the TOT group had urge incontinence preoper-atively,which disappeared in five and eight patients, respectively,at1-year follow-up.There were no significant between-group differences in patient satisfaction.
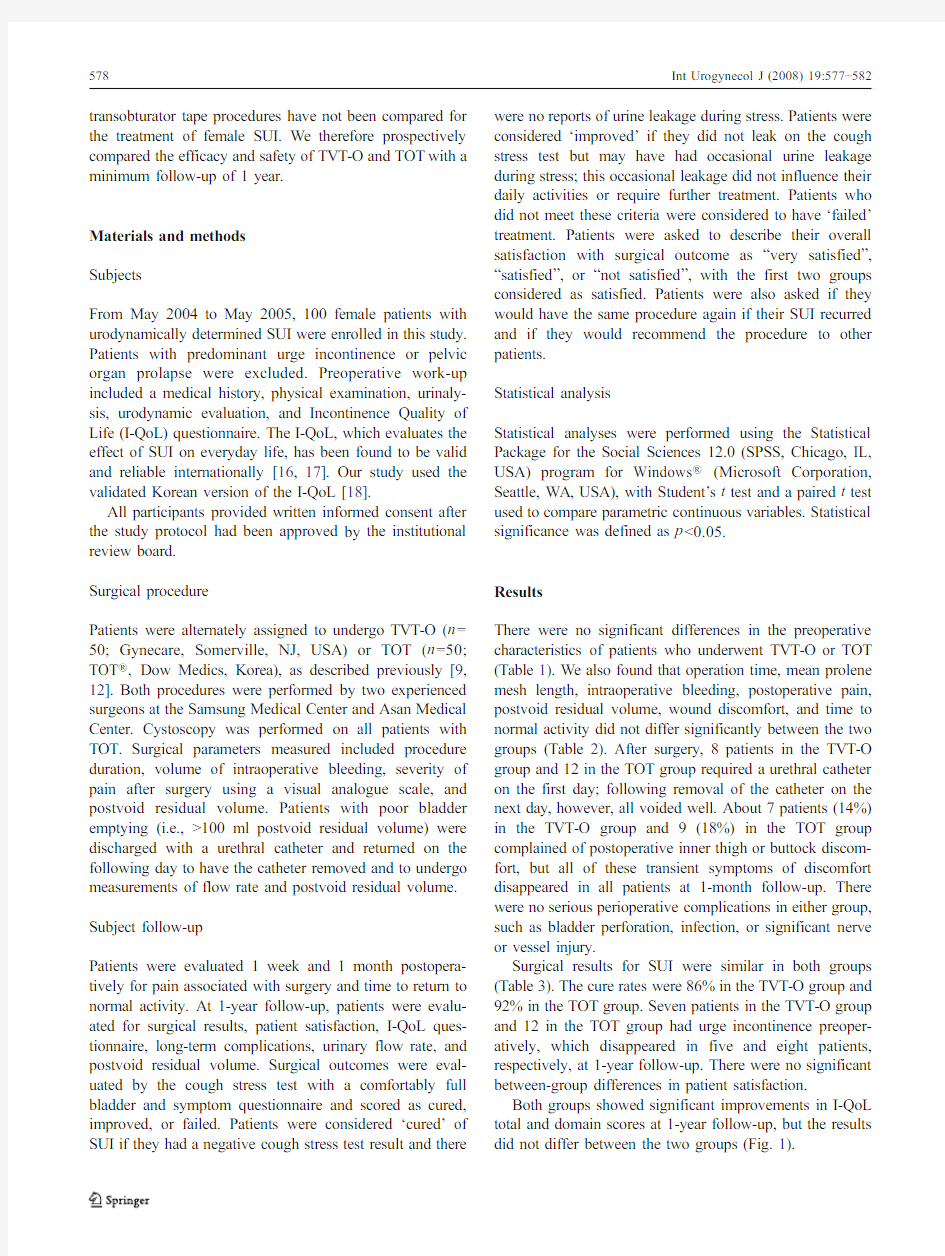
Both groups showed significant improvements in I-QoL total and domain scores at1-year follow-up,but the results did not differ between the two groups(Fig.1).
Mean maximum flow rate decreased significantly in both groups postoperatively,6.8ml/s in the TVT-O group and 6.5ml/s in the TOT group.Postvoid residual volume did not differ between the groups(Table4).De novo urge incontinence symptoms developed postoperatively in two TVT-O(4%)and one TOT(2%)patient(p=0.500).There were no other complications,such as prolonged voiding difficulty,wound infection,or vaginal erosion,in any of the patients.
Discussion
The effectiveness and safety of the transobturator approach are very promising,and the TVT-O and TOT procedures have become popular surgical treatments for female SUI [19].Short-term continence rates with TOT were similar to those of retropubic TVT[13–15].Some surgeons have personal preferences,but to our knowledge,there is no consensus on which of these procedures is superior.
We prospectively compared operation-related morbidity and surgical outcomes of the inside–out TVT-O and the outside–in TOT procedures in patients with a minimum follow-up of1year.Both procedures are minimally invasive,had similar operation-related morbidities,and appeared equally effective for the surgical treatment of SUI. Table2Surgery-related complications and morbidity in patients undergoing inside–out transobturator tape(TVT-O)and outside–in transobturator tape(TOT)procedures
TVT-O
(n=50)
TOT
(n=50)
p
Operative time(min)11.2±2.611.5±1.90.895a Used prolene mesh length(cm)16.1±1.715.7±1.80.226a Intraoperative bleeding(ml)33.1±19.232.9±23.10.966a Postoperative pain(V AS)
At2hours 2.7±1.3 2.6±1.20.643b At1week0.8±1.30.8±1.20.699b At1month0.1±0.20.2±0.40.167b Postvoid residual volume(ml)
On day of operation37.3±50.348.4±61.10.419b At1week after operation33.3±46.135.0±45.10.720b Catheterization patient8(16%)12(24%)0.227c Thigh discomfort7(14%)9(18%)0.393c Time to normal activity(days) 5.1±3.0 5.7±3.10.183b Short-term voiding difficulty8(16%)12(24%)0.393c Values are given as mean±SD(range)and n(%).
NS Not significant(p>0.05);VAS visual analogue scale
a Student’s t test
b Mann–Whitney test
c Chi-square test
Table3Surgical results of patients who underwent inside–out transobturator tape(TVT-O)and outside–in transobturator tape (TOT)procedures
TVT-O
(n=50)
TOT
(n=50)
p
Stress urinary incontinence
Cured43(86%)46(92%)0.262a Improved5(10%)2(4%)0.134b Failed2(4%)2(4%)0.691b Subjective satisfaction
Very satisfied31(62%)34(68%)0.338a Satisfied17(34%)15(30%)0.415a Not satisfied2(4%)1(2%)0.500b Patient would undergo reoperation if symptoms recur
Yes48(96%)47(94%)0.500a No2(4%)3(6%)0.500b Recommend to other patients
Yes48(96%)45(90%)0.218a No2(4%)5(10%)0.218b Values are given as n(%).
NS Not significant(p>0.05)
a Chi-square test
b Fisher’s exact test
Table1Preoperative characteristics of patients who underwent inside–out transobturator tape(TVT-O)and outside–in transobturator tape(TOT)procedures
TVT-O (n=50)TOT
(n=50)
p
Age(years)52.3±7.353.1±8.10.595a Parity(times) 2.48±1.1 1.5±0.50.140b Menopause20(40%)21(42%)0.5c Previous pelvic surgery8(16%)8(16%)0.607c Previous incontinence
surgery
4(8%)4(8%)0.643c
Preoperative clinical parameters
Symptomatic period(years) 6.9±4.67.4±4.70.607b Grade of SUI(1–3) 1.6±0.7 1.6±0.60.479b Preoperative urodynamic parameters
Qmax(ml/s)24.1±7.625.7±9.10.324a Postvoid residual urine(ml)17.9±27.923.7±23.70.967b ALPP(cm H2O)92.3±41.878.5±41.80.104a I-QoL scores
Total57.9±13.959.2±17.30.699a Avoidance and limiting
behavior
44.1±18.446.2±21.20.605a
Psychosocial impacts34.6±16.532.6±19.90.586a Social embarrassment43.9±17.644.0±20.50.987a Values are given as mean±SD(range)and n(%).
NS Not significant(p>0.05);SUI stress urinary incontinence;Qmax maximum flow rate;ALPP abdominal leak point pressure;I-QoL incontinence quality of life
a Student’s t test
b Mann–Whitney U test
c Chi-square test
The original transobturator midurethral sling procedure consisted of an outside –in approach with the tunneller passed from the skin incision to the vaginal incision [9].Assessment of the efficacy and safety of TOT for SUI in 183patients showed cure rates of 85.6and 83%at 3-and 6-months,respectively;at 1-year,80.5%remained cured,and 7.5%were improved [10].Similar results were obtained for patients undergoing TOT alone and those undergoing TOT with concurrent prolapse surgery.For the inside –out approach,a new helical tunneller and introducer were developed to pass the tape from the vaginal incision through the obturator foramen and toward the thigh fold without entering the pelvic region [12].When we prospec-tively compared TVT and TVT-O,we found that the SUI cure rates at 1year were 86.8and 86.8%,respectively [15].In this study,the cure rates were 86%for TVT-O and 92%for TOT.Although the sample size may have been inadequate to identify a real difference between the procedures,we found that,at 1year,the cure rates of TVT-O and TOT were similar to each other and similar to that of TVT.
Debodinance [20]also conducted nonrandomized,pro-spective study of 100SUI patients:50TVT-O vs 50Monarc (American Medical Systems,Minnetonka,
MN,
Fig.1Changes in mean I-QoL total and domain scores after inside –out transobturator tape (TVT-O)and outside –in transobturator tape (TOT)procedures after 1year.a Total scores.b Avoidance behaviors.c Psychosocial impacts.d Social embarrassment.I-QoL Incontinence
quality of life.*p <0.05compared with preoperative values.?p >0.05changes from preoperative to postoperative between the TVT-O and TOT groups
USA).The cure rate at1year was94%in the TVT-O group vs90%in the Monarc group,and the results are very similar to those reported in this study.
Compared with TVT,both TVT-O and TOT can eliminate the complications related to penetration of the retropubic space,thus eliminating the risk of bowel and major vascular injury.While bladder perforation is the most common complication occurring during TVT,the transobturator approach reduces the risks of bladder and urethral perfora-tion,thus eliminating the need for cystoscopy.However, bladder perforation during TOT was reported in3of61 patients[21].Theoretically,the transobturator tape does not penetrate the retropubic space,but the tip of the tunneller can injure the bladder,the bladder neck,or the urethra if its course is misaligned or in an oblique direction[22].We performed cystoscopy on all TOT patients,but there was no incidence of bladder perforation.Bladder perforation during TOT can be avoided by insertion of an index finger into the vaginal dissection.Since there have been no reports of bladder perforation during TVT-O,we did not perform cystoscopy during this procedure.
Implantation of a TVT,TVT-O,and Monarc tape in each of ten embalmed hemipelvises,and measurement of the distance between the dorsal nerve of the clitoris and the obturator canal relative to the devices showed that,while the distances relative to the nerve were the same,TVT-O was closer to the obturator canal and TVT was more distant, indicating that the nerve path can be avoided using the outside–in route,whereas the inside–out route is closer to the obturator canal[23].Dissection of12fresh frozen cadavers and measurement of the trajectory of the TVT-O tape showed that this technique was safe,reliable,and reproducible[24].We observed no incidence of nerve injury using either procedure.
De Leval[12]performed inside–out transobturator sling surgery on107SUI women,of which33(31%) underwent simultaneous prolapse repair and none had any intraoperative complications.At1-month follow-up,how-ever,one patient had minor vaginal erosion,and three developed complete urinary retention(two of whom had undergone prolapse repair),requiring urethrolysis.In our study,20patients(8TVT-O and12TOT)required a urethral catheter on the first day postoperatively,but following catheter removal the next day,all voided well.
In comparative study of two versions of the transobturator tape,outside–in technique using the Obtape(Mentor-Porges, Le Plessis Robinson,France)developed more vaginal erosion than the inside–out TVT-O(7.29vs 1.78%,p< 0.05)[25].This is in disagreement with our results,which demonstrated that there were no tape erosions with both techniques.However,other factors related to vaginal erosion, apart from the surgical technique,such as biomechanical properties of the mesh used,infection,and the properties of tissue,need to be addressed to analyze the tape-erosion pattern.
The vaginal incision was longer in the TOT(1.5–2cm) than in the TVT-O(1.0cm)procedure because the former should be large enough to allow the surgeon to introduce his index finger against the ischiopubic https://www.360docs.net/doc/8c13220818.html,rger incisions and increased dissection may cause tape mi-gration.Vaginal dissection had to be deeper in TVT-O because the obturator membrane was perforated with the tip of the scissors,and the introducer was pushed into the preformed dissection pathway until it reached and perforated the obturator membrane.We found,however, that intraoperative blood loss in the two groups did not differ significantly.
We did not observe significant between-group differ-ences in success rate,satisfaction rate,postoperative pain, and voiding difficulty.Although we have no preferences in general,we prefer TVT-O for patients with narrow vaginas and those with hard or bad tissue conditions of the vagina because TVT-O requires less dissection than TOT.
Conclusions
We would like to conclude that in our series,TVT-O and TOT appear equally effective for female SUI.However,this study was unable to identify a difference between the two procedures.The findings may be due to the underpowered nature of the study.Ideally,large well-constructed random-ized controlled trial with longer follow-up period is necessary to determine any differences in long-term surgical outcomes and complications.
Table4Uroflometry and postvoid residual in patients who underwent inside–out transobturator tape(TVT-O)and outside–in transobturator tape(TOT)procedures
Preoperative Postoperative p Qmax(ml/s)
TVT-O(n=50)24.1±7.617.3±6.6<0.001 TOT(n=50)25.7±9.119.2±5.9<0.001 PVR(ml)
TVT-O(n=50)17.9±27.927.9±33.50.105a TOT(n=50)23.7±23.724.9±32.80.865a
NS b NS b
Values are given as mean±SD(range).
NS Not significant(p>0.05);Qmax maximum flow rate;PVR postvoid residual volume
a Paired t test
b Student’s t test
References
1.Abrams P,Cardozo L,Fall M,Griffiths D,Rosier P,Ulmsten U
et al(2002)The standardisation of terminology of lower urinary tract function:report from the Standardisation Sub-committee of the International Continence Society.Neurourol Urodyn 21:167–178
2.Choo MS,Ku JH,Oh SJ,Lee KS,Paick JS,Seo JT et al(2007)
Prevalence of urinary incontinence in Korean women:an epidemiologic survey.Int Urogynecol J Pelvic Floor Dysfunct doi:10.1007/s00192–007–0322-z
3.Ulmsten U,Petros P(1995)Intravaginal slingplasty(IVS):an
ambulatory surgical procedure for treatment of female urinary incontinence.Scand J Urol Nephrol29:75–82
4.Petros PE,Ulmsten UI(1993)An integral theory and its method
for the diagnosis and management of female urinary incontinence.
Scand J Urol Nephrol Suppl153:1–93
5.Doo CK,Hong B,Chung BJ,Kim JY,Jung HC,Lee KS et al
(2006)Five-year outcomes of the tension-free vaginal tape procedure for treatment of female stress urinary incontinence.
Eur Urol50:333–338
6.Nilsson CG,Falconer C,Rezapour M(2004)Seven-year follow-
up of the tension-free vaginal tape procedure for treatment of urinary incontinence.Obstet Gynecol104:1259–1262
7.Holmgren C,Nilsson S,Lanner L,Hellberg D(2005)Long-term
results with tension-free vaginal tape on mixed and stress urinary incontinence.Obstet Gynecol106:38–43
8.Meschia M,Pifarotti P,Bernasconi F,Guercio E,Maffiolini M,
Magatti F et al(2001)Tension-Free vaginal tape:analysis of outcomes and complications in404stress incontinent women.Int Urogynecol J Pelvic Floor Dysfunct12Suppl2:S24–27
9.Delorme E,Droupy S,de Tayrac R,Delmas V(2004)Transobturator
tape(Uratape):a new minimally-invasive procedure to treat female urinary incontinence.Eur Urol45:203–207
10.Costa P,Grise P,Droupy S,Monneins F,Assenmacher C,
Ballanger P et al(2004)Surgical treatment of female stress urinary incontinence with a trans-obturator-tape(T.O.T.)Uratape: short term results of a prospective multicentric study.Eur Urol 46:102–106
11.Mansoor A,Védrine N,Darcq C(2003)Surgery of female urinary
incontinence using trans-obturator tape(TOT):a prospective randomised comparative study with TVT.Neurourol Urodyn 22:488–489
12.de Leval J(2003)Novel surgical technique for the treatment of
female stress urinary incontinence:transobturator vaginal tape inside–out.Eur Urol44:724–73013.deTayrac R,Deffieux X,Droupy S,Chauveaud-Lambling A,
Calvanese-Benamour L,Fernandez H(2004)A prospective random-ized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence.
Am J Obstet Gynecol190:602–608
14.Mellier G,Benayed B,Bretones S,Pasquier JC(2004)Suburethral
tape via the obturator route:is the TOT a simplification of the TVT?
Int Urogynecol J Pelvic Floor Dysfunct15:227–232
15.Lee KS,Han DH,Choi YS,Yum SH,Song SH,Doo CK et al
(2007)A prospective trial comparing tension-free vaginal tape and transobturator vaginal tape inside–out for the surgical treatment of female stress urinary incontinence:1-year followup.J Urol 177:214–218
16.Wagner TH,Patrick DL,Bavendam TG,Martin ML,Buesching
DP(1996)Quality of life of persons with urinary incontinence: development of a new measure.Urology47:67–71
17.Patrick DL,Martin ML,Bushnell DM,Yalcin I,Wagner TH,
Buesching DP(1999)Quality of life of women with urinary incontinence:further development of the incontinence quality of life instrument(I-QoL).Urology53:71–76
18.Oh SJ,Park HG,Lim SH,Hong SK,Kim SW,Kim HH et al
(2002)Translation and linguistic validation of Korean version of the Incontinence quality of life(I-QoL)instrument.J Korean Continence Soc6:10–23
19.Al-Singary W,Shergill IS,Allen SE,John JA,Arya M,Patel HR
(2007)Trans-obturator tape for incontinence:a3-year follow-up.
Urol Int78:198–201
20.Debodinance P(2007)Trans-obturator urethral sling for the
surgical correction of female stress urinary incontinence:Out-side–in(Monarc)versus inside–out(TVT-O)Are the two ways reassuring?Eur J Obstet Gynecol Reprod Biol133:232–238 21.Minaglia S,Ozel B,Klutke C,Ballard C,Klutke J(2004)Bladder
injury during transobturator sling.Urology64:376–377
22.Delmas V,Hermieu JF,Dompeyre P(2003)The transobturator
tape Uratape:anatomical dangers.Eur Urol Suppl2:197
23.Achtari C,McKenzie BJ,Hiscock R,Rosamilia A,Schierlitz L,
Briggs CA(2006)Anatomical study of the obturator foramen and dorsal nerve of the clitoris and their relationship to minimally invasive slings.Int Urogynecol J Pelvic Floor Dysfunct17:330–334
24.Bonnet P,Waltregny D,Reul O,de Leval J(2005)Transobturator
vaginal tape inside out for the surgical treatment of female stress urinary incontinence:anatomical considerations.J Urol173:1223–1228 25.Abdel-Fattah M,Sivanesan K,Ramsay I,Pringle S,Bjornsson S
(2006)How common are tape erosions?A comparison of two versions of the transobturator tension-free vaginal tape procedure.
BJU Int98:594–598
