阿司匹林抵抗与COX1 COX2

Original Article
Genetic Polymorphisms of HO-1and
COX-1Are Associated With Aspirin
Resistance Defined by Light Transmittance
Aggregation in Chinese Han Patients
Xiao-li Li,MD1,2,Jian Cao,MD1,Li Fan,MD1,Qiang Wang,BSc3,Ling Ye,MD4,
Chun-Ping Cui,PhD5,Ya-Zhen Wang,MBBS2,Lin Liu,PhD1,Bin Li,MBBS2,
Ruo-jun Wu,MBBS2,Feng-chun Zhou,BA6,and Jun-hong Zhang,BA2
Abstract
Background:Cyclooxygenase1(COX-1),COX-2,and HO-1are involved in the process of aspirin’s effect.The genetic susceptibility of these enzymes to aspirin resistance(AR)is unclear.Methods:A total of431patients took https://www.360docs.net/doc/b56474828.html,ing arachidonic acid-induced light transmittance aggregation combined with adenosine diphosphate-induced light transmittance aggregation, 36participants served for AR,164participants for semi-AR,and231participants for aspirin sensitivity(AS).The AR with9 single-nucleotide polymorphism in COX-1,COX-2,and HO-1genes was investigated.Results:COX-1rs1330344(à1676A>G) is associated with AR.G-Allele carriers significantly increased the risk of AR.For patients with AS as control,P is.02(odds ratio[OR]?1.77,confidence interval[CI]:1.07-2.92).For patients with semi-AR as control,P is.05.HO-1rs2071746 (à413A>T)is associated with AR.T-Allele carriers significantly increased the risk of AR.For patients with AS as control, P is.04(OR?1.70,CI:1.02-2.79).For patients with semi-AR as control,P is.05(OR?1.68,CI:1.00-2.80).Conclusion: rs2071746in HO-1gene,rs1330344in COX-1gene contribute to AR.
Keywords
aspirin resistance,single-nucleotide polymorphism(SNP),platelet aggregation,hemoxygenase-1(HO-1),cyclooxygenase-1 (COX-1)
Introduction
Nowadays,atherothrombotic diseases have become the leading cause of death in elderly Chinese.Aspirin is still the corner-stone of treatment and prevention for these diseases.1However, epidemiological surveys2have discovered that0.4%to70.1% patients are poor response to aspirin application,known as aspirin resistance(AR).Platelet aggregation measured by pla-telet function tests cannot be effectively inhibited after taking aspirin,known as laboratory AR.Prospective analysis in clin-ical events has shown that patients with laboratory AR have an increased risk of adverse clinical outcomes.3-6Therefore, investigating the mechanism of laboratory AR may aid in the clinical use of aspirin.The Framingham heart study found that the heritable factors are the key determinants for platelet aggre-gation.7We hypothesized that the genetic susceptibility may be the key to aspirin sensitivity(AS),despite other acquired determinants.
For aspirin-resistance genetic screening,the methods used to describe the phenotype must be reliable.Aspirin is a nonse-lective and irreversible inhibitor of cyclooxygenase(COX),which exists in2main isoforms,COX-1and COX-2.The anti-platelet effect of aspirin is recognized as being due to the irreversible inhibition of platelet COX-1and reduction in thromboxane A2(TXA2)production.This function can be
1First Department of Geriatric Cardiology of South Building,Chinese People’s Liberation Army General Hospital,Beijing,China
2Department of Geriatric Cardiology,Beijing309Hospital,Beijing,China
3Department of Transplantation Center,Beijing309Hospital,Beijing,China 4Department of Geriatrics,Chinese People’s Liberation Army General Hos-pital,Beijing,China
5Department of Experimental Haematology,Beijing Institute of Radiation Medicine,Beijing,China
6Department of Health Screening Center,Beijing309Hospital,Beijing,China Xiao-li Li and Jian Cao equally contributed for this work.
Corresponding Author:
Li Fan,First Department of Geriatric Cardiology of South Building,Chinese People’s Liberation Army General Hospital,27Fuxing Road,Beijing100853, People’s Republic of China.
Email:fanli301301@https://www.360docs.net/doc/b56474828.html,
Clinical and Applied
Thrombosis/Hemostasis
19(5)513-521
aThe Author(s)2013
Reprints and permission:
https://www.360docs.net/doc/b56474828.html,/journalsPermissions.nav
DOI:10.1177/1076029612444002
https://www.360docs.net/doc/b56474828.html,
detected by arachidonic acid(AA)-induced light transmittance aggregometry(LTA)in vitro,which is regarded as‘‘gold standard.’’8However,another study found that the adenosine diphosphate(ADP)-dependent pathway allows platelets to remain active in some aspirin-treated patients.9Thus in our study,AA-induced light transmittance aggregation combined with ADP-induced light transmittance aggregation was selec-ted for screening AR phenotype.
Hemoxygenase-1(HO-1)is another enzyme that has been shown to be involved in the antithrombotic effects of aspirin.10 Therefore,we proposed that genetic variants of HO-1,in addi-tion to COX-1and COX-2,might also determine aspirin respon-siveness.The genetic polymorphisms of these3enzymes might be involved in AR.We screened these3genes for polymorph-isms looking at9single-nucleotide polymorphisms(SNPs)with the Sequenom iPlex platform.
Methods
Patients
For this study,information and DNA samples were obtained from consecutive patients who presented between April2008 and June2010and took part in physical examination every year in Chinese PLA General hospital,Beijing309hospital,and Navy General Hospital in Beijing with coronary artery disease (CAD),stroke,and peripheral arterial occlusive disease(PAOD) who had been receiving regular aspirin therapy(75-160mg daily)for at least4weeks.Inclusion criteria were!65years of age.Exclusion criteria included the use of clopidogrel,ticlo-pidine,dipyridamole,or other nonsteroidal anti-inflammatory drugs,heparin or low-molecular-weight heparin;acute vascular events;platelet count<150000000/L or>450000000/L;and hemoglobin<8g/dL.Any patients that admitted noncompliance or intermittent compliance were excluded from the analyses.The study was approved by the Scientific and Ethics Review Board of the First Geriatric Cardiology Division,Chinese PLA General Hospital(Beijing,People’s Republic of China).All patients pro-vided written informed consent before inclusion in the study.
Following the screening procedures,431patients on aspirin therapy were enrolled.By the LTA diagnostic criteria detailed below,there were36patients with AR,164patients were par-tial AR or semi-AR,and231patients with AS.These3groups are comparable.
Blood Sampling
Blood samples were obtained from patients between7AM and9 AM,2to12hours after ingestion of the last dose of aspirin to
eliminate the effects of circadian variation on platelet function. The first2mL of blood drawn by venipuncture through a21-gauge needle was discarded.Tubes that contained3.2%sodium citrate were used for LTA and1tube that contained a clavicular tilt angle difference(a mixture of citrate,theophylline,adeno-sine,and dipyridamole)was collected for the measurement of CD62P(P-selectin)and PAC-1(activated GP IIb/IIIa receptors). In addition,3conventional tubes were drawn for high-sensitivity C-reactive protein(hs-CRP),type-B natriuretic peptide,homo-cysteine(HCY),and protein C;the percentage activity of antith-rombin III(ATIII);routine measurement of blood components and blood lipids;and other biochemistry measurements.All assays were processed within2hours of blood sampling. Light Transmittance Aggregation
Platelet aggregation was assessed in platelet-rich plasma at 37 C by LTA.Samples were centrifuged at800rpm for5min-utes to obtain native platelet-rich plasma.The platelet count was assessed using a standard cell counter.Platelet-poor plasma was obtained by the centrifugation of remaining blood at4000rpm at room temperature for8minutes.Aggregation was measured with a ChronoLog Aggregometer(Chronolog, Havertown,Pennsylvania).Aggregation was expressed as the maximal percentage change in light transmittance from base-line after the addition of AA(0.5mmol/L)and ADP(10m mol/ L),with platelet-poor plasma used as the reference.On the basis of this platelet aggregation assay,the definition of AR was the aggregation of!70%with10m mol/L ADP and of !20%with0.5mg/mL AA.9,11Aspirin sensitivity was indi-cated by neither of these criteria being met;AR by both cri-teria being met;only one of the2criteria met was deemed partial AR or semi-AR.
Single-Nucleotide Polymorphism Detection
DNA samples were extracted from peripheral blood obtained from all the patients with AR and AS by a standard phenol–chloroform method.The SNP detection was performed by the use of the Sequenom MassARRAY iPLEX platform(Seque-nom,California and USA).12The assay consists of an initial locus-specific polymerase chain reaction(PCR),followed by single-base extension that uses mass-modified dideoxynucleo-tide terminators of an oligonucleotide primer.The PCR primers and single-base extension probes were designed by the Assay Design 3.1software from Sequenom.The genes and their respective haplotypes as well as the primer pairs and probes are listed in Table1.The SNPs were genotyped by the Sequenom MassArray system according to the instructions of the manufac-turer.The PCR was performed using iPlex chemistry according to the recommendations of the manufacturer as found in the MassArray iPlex standard operating procedure.Data analysis was performed with the MassArray Typer software version4.0. Statistical Analysis
Comparisons of the continuous variables were made using the analysis of variance(ANOVA)test or Wilcoxon rank sum test, dependent upon the distribution of the data.Normal data are presented as mean+standard deviation,data of skewness dis-tribution are presented as median(Q R),Q R?Q3àQ1.All SNPs evaluated in this study were tested for deviation from the Hardy-Weinberg equilibrium with the use of a chi-square test by Haploview4.2software.Genotype and allele differences
514Clinical and Applied Thrombosis/Hemostasis19(5)
between the SNPs used Pearson chi-square test or Fisher exact test by THESIS software.The associations between HO-1 polymorphisms,COX-1polymorphisms,and AR were ana-lyzed in logistic regression models after the adjustment of age and gender by SNPstats in Web.The odds ratio(OR)and95% confidence interval(CI)were used to estimate the associations of allele,genotype,and haplotype between the case and con-trol.P<.05was considered statistically significant. Results
Characteristics of the Patients
The study analysis included431patients on aspirin therapy. Baseline clinical characteristics are shown in Table2.Based on the criteria of the AA-induced aggregation and ADP-induced aggregation,231(53.60%)patients were shown to be sensitive to aspirin,while164(38.05%)patients were clas-sified as semi-AR and36(8.35%)patients were classified as AR.These3groups were comparable.No significant differ-ences were found among the3groups with respect to age,sex, body mass index(BMI),smoking habits,alcohol,hypertension, CAD,cerebrovascular disease,PAOD,use of calcium-channel blockers,platelet count,Blood urea nitrogen(BUN),creati-nine,glucose,cholesterol,high density lipoprotein(HDL), low-density lipoprotein(LDL),HCY,hs-CRP,ATIII activity,PAC-1,and CD62P.In contrast,a significant difference was observed in those patients who take angiotensin-converting enzyme inhibitors/angiotensin receptor blockers(P?.014) and nitrates(P?.003).
Allelic and Genotype Frequencies
The allelic and genotypic frequencies of COX-1_rs1888943, COX-1_rs3842787,COX-1_rs5787,COX-1_rs5789,COX-1_rs5794,COX-2_rs5277,and COX-2_rs20417variants did not differ significantly among all the patients with AR, semi-AR,and AS.However,between the patients with AR and AS or with semi-AR,the frequencies of the COX-1_rs1330344variant alleles,HO-1_rs2071746variant alleles, and HO-1_rs2071746variant genotypes differed significantly (Table3).
HO-1rs2071746(à413A>T)Associated With AR The T allele of HO-1in rs2071746(à413A>T)was associated with AR,when compared with not only AS patients but also with semi-AR patients(P?.04and.05;OR?1.70and 1.68;CI?[1.02,2.79]and[1.00,2.80],respectively).In con-trast,the T allele in rs2071746(à413A>T)was not associated with semi-AR(P?.94,OR?1.01,CI?[0.76,1.35]),when
Table1.Details of the Primers and Probes for the Candidate Genes.
Gene Ref SNP Base Change Primer and Probe
COX-1Rs1888943à8759C>T Second:ACGTTGGATGAAAGGAACCAGAGCTGGTGA
First:ACGTTGGATGACCCTCAGAAAGCTACCTCT
Probe:AGGGTGGTTGAGGTTGTTATCC
Rs1330344à1676A>G Second:ACGTTGGATGCACCCATCTGCACTCAAAAC
First:ACGTTGGATGTCTGATTCTGAGGTGAAGGC
Probe:ccccgTGTGTGGCCCTGGCACTA
Rs384278750C>T Second:ACGTTGGATGCTGGGTCCGCGAGCAGGA
First:ACGTTGGATGTCTGCAGGGAGTCTCTTGCT
Probe:AGGACGGGGAGCGGC
Rs5787323G>A Second:ACGTTGGATGTGGGAGTTTGTCAATGCCAC
First:ACGTTGGATGATAAGGTTGGAGCGCACTGT
Probe:gCAATGCCACCTTCATCCA
Rs5789709C>A Second:ACGTTGGATGTCTGTCCACAGGTAGACCTC
First:ACGTTGGATGTCCTTAAAGAGCCGCAGTTG
Probe:cctGCCACATTTATGGAGACAATC
Rs57941441G>A Second:ACGTTGGATGAGGGACTGCATCCAGGAAAC
First:ACGTTGGATGGGTTTGGCATGAAACCCTAC
Probe:ACAGCTGCTCACCTAC
COX-2Rs20417à765G>C Second:ACGTTGGATGTGTTCTCCGTACCTTCACCC
First:ACGTTGGATGAGGACCAGTATTATGAGGAG
Probe:TTGTTTCTTGGAAAGAGAGG
Rs5277306G>C Second:ACGTTGGATGATTCCCTTCCTTCGAAATGC
First:ACGTTGGATGGCTAAAAACCTTAGAAAGAC
Probe:CGAAATGCAATTATGAGTTATGT
HO-1Rs2071746à413A>T Second:ACGTTGGATGTCCCAGAAGGTTCCAGAAAG
First:ACGTTGGATGGGGTTGCTAAGTTCCTGATG
Probe:AGCGCTGCTCAGAGCAA
Abbreviations:Ref,reference;SNP,single-nucleotide polymorphism.
Li et al515
compared with patients with AS(Table3).Patients who were homozygous or heterozygous for the T allele were signif-icantly more likely to have aspirin resistance(genotype AT or TT)in the HO-1gene compared with the AA wild-type gen-otype,the AT and TT genotypes significantly increased the risk of AR,while patients with AS acting as a control,P is .0077(OR? 3.31,CI?[1.24-8.83]);adjusted by age and sex,P is.0058(OR?3.47,CI?[1.29-9.34]).Patients with Semi-AR acting as a control,P is.0024(OR?3.95, CI?[1.46-10.68]);adjusted by age and sex,P is.0022 (OR?4.03,CI?[1.48-10.96];Table4).COX-1rs1330344(à1676A>G)Associated
With AR
The G allele of COX-1rs1330344(à1676A>G)was associated with AR,when compared with not only the AS patients but also with semi-AR patients(P?.02and.05,OR?1.77and 1.66,CI?[1.07,2.92]and[0.99,2.77],respectively]).In contrast,the G allele of COX-1rs1330344(à1676A>G)was not associated with semi-AR,P?.66,OR?1.07,CI?[0.80,1.43],when compared with patients with AS(Table3). However,the P value of genotype frequencies of COX-1
Table2.Demographic Details for the Patients.
Variable AR(n?36)Semi-AR(n?164)AS(n?231)P Value Age,years76.33+8.8574.02+8.0373.88+8.00.234 No.of female115978.796 BMI,kg/m224.93+3.2624.93+3.9825.29+3.60.614 Weistline,cm89.68+9.7191.72+11.8191.95+11.69.689 No.of smokers114151.495 No.of drinkers63545.789 No.exercise32149208.925 No.hypertension27109165.445 No.coronary artery disease2491131.465 No.ICVD165885.592 No.PAOD61321.259 No.hyperlipoidemia145891.413 No.atrial fibrillation1310.380 No.diabetes mellitus1969106.467 No.COPD21629.381 No.CRF2913.998 No.CHF134961.434 Medication
No.ACEIs/ARBs61546.014a https://www.360docs.net/doc/b56474828.html,Bs106384.486 No.statins164564.096 No.nitrates13263.003a Laboratory data
Platelet count,per m L207.60+67.40209.30+59.47207.81+57.11.969 BUN,mmol/L 6.58+2.08 6.02+1.53 5.75(5.12).301b Creatinine,m mol/L83.88+25.4482.78+51.7978.67+25.15.465 UA,mmol/L325.00+107.72327.13+88.90324.66+84.79.969 Glucose,mmol/L 6.25+1.31 6.11+1.45 6.04+1.35.697 Total cholesterol,mmol/L 4.75+1.00 4.82+1.03 5.18+3.11.272 Triglyceride,mmol/L 1.78+0.92 1.63+0.72 1.57+0.70.277 HDL,mmol/L 1.28+0.38 1.27+0.34 1.34+0.37.126 LDL,mmol/L 2.82+0.80 2.85+0.79 2.30+0.91.797 HCY,m mol/L16.59+4.5216.19+7.2417.98+9.50.122 hs-CRP(mg/dL)0.22(0.27)0.24(0.23)0.22(0.31).784b ATIII activity,%101.18+16.26105.39+12.63105.13+14.68.283 NT-proBNP(pg/mL)95.10(104.13)70.10(80.00)75.10(85.05).090b PAC-1(%)43.30(53.90)46.20(45.45)41.10(51.05).097b CD62P(%) 6.60(11.70)8.50(13.85) 5.75(15.85).570b Abbreviations:BMI,body mass index;PAOD,peripheral arterial occlusive disease;AR,aspirin resistance;AS,aspirin sensitivity;ACEIs,angiotensin-converting enzyme inhibitor;ARBs,angiotensin receptor blocker;CCBs,calcium-channel blockers;HCY,homocysteine;hs-CRP,high-sensitivity C-reactive protein;ATIII, antithromibin III;BNP,type-B natriuretic peptide;ICVD,ischemic cerebrovascular disease;COPD,chronic obstructive pulmonary disease;CRF,chronic renal failure;CHF,chronic congestive heart failure;UA,uric acid;HDL,high density lipoprotein;LDL,low-density lipoprotein;NT-proBNP,N-terminal Pro-Brain Natriuretic Peptide;CD62P,P-selectin;PAC-1,activated GP IIb/IIIa receptors.
a P<.05.
b Skewed distribution of data.
516Clinical and Applied Thrombosis/Hemostasis19(5)
Table3.Distribution of SNPs in HO-1,COX-1and COX-2Genes Among the3Groups.
Ref SNP
Aspirin Resistance
vs Aspirin-Sensitivity
Aspirin Resistance vs
Semi-Aspirin Resistance
Semi-Aspirin Resistance
vs Aspirin-Sensitivity
Case
(n?36)
Control
(n?231)
P Value
(OR,95%CI)
Case
(n?36)
Control
(n?164)
P Value
(OR,95%CI)
Case
(n?164)
Control
(n?231)
P Value(OR,
95%CI)
COX-1_rs1888943
Allele.69.51.38
C7246172326326461.35(0.03,3.92) T010221 2.83(0.26,31.32) Genotype.92.80.67
CC3623036162162230
CT010221
TT000000
COX-1_rs1330344
Allele.02a.05a0.66
A34282.56(0.34,0.93)34196.60(0.36,1.01)196282.94(0.70,1.25) G38178 1.77(1.07,2.92)38132 1.66(0.99,2.77)132178.07(0.80,1.43) Genotype.1.070.18
AA993.49(0.22,1.09)956.64(0.28,1.46)56930.76(0.50,1.16) AG1696 1.12(0.55,2.27)1684.76(0.37,1.57)8496.47(0.98,2.19) GG1141 2.03(0.92,4.45)1124 2.57(1.12,5.90)2441.79(0.46,1.37) COX-1_rs3842787
Allele.69.64.8
G72461723253254610.71(0.04,11.31) A010111.42(0.09,22.76) Genotype.92.9.97
GG3623036162162230.70(0.04,11.34) AG010111 1.42(0.09,22.87) A000000
COX-1_rs5787
Allele.69.34.08
A010441 5.73(0.64,51.48) G7246172322322461.17(0.02,1.57) Genotype.92.8.17
AA000220
AG010001
GG3623036161161230.35(0.032,3.90) COX-1_rs5789
Allele1.64.23
A000110
C7246272325325462
Genotype1.9.49
AA000000
AC000110
CC3623136162162231
COX-1_rs5794
Allele11
C72462723281328462
Genotype1
CC362311721641164231
COX-2_rs5277
Allele.1.28.46
C514 2.39(0.83,6.84)513 1.79(0.62,5.18)1314 1.34(0.62,2.89) G67448.49(0.15,1.20)67311.56(0.19,1.62)3114480.75(0.35,1.61) Genotype.24.54.75
CC000000
CG514 2.50(0.84,7.42)513 1.85(0.61,5.56)1314 1.35(0.62,3.00) GG31217.40(0.13,1.19)31149.54(0.18,1.63)149217.74(0.34,1.62)
(continued) Li et al517
rs1330344and allele frequencies were not consistent(Table3). The AA,AG,and GG genotypes showed no differences among the3groups.In a recessive genetic model,compared with semi-AR,the GG genotype was significantly associated with aspirin resistance,P?.0032,OR?2.57,CI?1.12-5.89, adjusted by age and sex,P?.031,OR?2.59,CI?1.12-5.98(Table4).
COX-1Haplotype Associated With AR
Six SNPs in COX-1were selected.Both rs1888943and rs1330344are in the promoter region of COX-1gene,the other 5SNPs in the exons of COX-1gene(information from http:// https://www.360docs.net/doc/b56474828.html,/SNP).Besides rs1330344,the other SNPs are rare in the Chinese Han population(Table5).The COX-1haplotype is dominated by rs1330344.Patients who car-ried the variant haplotype CGCGCG in COX-1gene compared with the COX-1wild-type haplotype were more likely to have AR.When patients with AS act as control,P?.032,OR?1.69,CI?1.05-2.71.When patients with semi-AR act as control, P?.044OR?1.72,CI?1.02-2.92(Table6).
COX-2Genetic Association With AR
The alleles and genotypes of rs5277and rs20417showed no differences among the3groups(Table3).The minor allele frequency of rs20417is also rare in the Chinese Han population.
https://www.360docs.net/doc/b56474828.html,rmation of Selected SNPs in COX-1Gene.
Ref SNP MAF MAF(NCBI)Position Protein Change rs18889430.0020.0715–8759C>T
rs13303440.4040.3362–1676A>G
rs38427870.0020.0636Exon2,50C>T p.Pro17Leu
rs57870.003Exon4,323G>A p.Arg108Gln rs57890.0010.0221Exon7,709C>A p.Leu237Met rs579400.011Exon10,1330G>A p.Val481Ile Abbreviations:Ref,reference;SNP,single-nucleotide polymorphism.
Table3(continued)
Ref SNP
Aspirin Resistance
vs Aspirin-Sensitivity
Aspirin Resistance vs
Semi-Aspirin Resistance
Semi-Aspirin Resistance
vs Aspirin-Sensitivity
Case
(n?36)
Control
(n?231)
P Value
(OR,95%CI)
Case
(n?36)
Control
(n?164)
P Value
(OR,95%CI)
Case
(n?164)
Control
(n?231)
P Value(OR,
95%CI)
COX-2_rs20417
Allele1.64.23
G000110
C7246272323323462
Genotype1.89.49
GG000000
CG000110
CC3623136161161231
HO-1_rs2071746
Allele.04a.05a.94
T39189 1.70(1.02,2.79)39134 1.68(1.00,2.80)134189 1.01(0.76,1.35) A33271.59(0.36,0.97)33190.60(0.36,0.99)190271.99(0.74,1.32) Genotype.04a.01a.21
TT839 1.40(0.59,3.30)835 1.04(0.43,2.48)3539 1.35(0.81,2.24) AT23111 1.90(0.92,3.93)2364 2.71(1.23,5.73)64111.70(0.47,1.05) AA580.30(0.11,0.81)563.25(0.09,0.68)6380 1.19(0.77,1.81) Abbreviations:Ref,reference;SNP,single-nucleotide polymorphism;OR,odds ratio;CI,confidence interval.
a P<0.05.
Table4.Genotype of rs2071746(A>T)Responses to Aspirin Resistance.
Group Genotype Control(%)Case(%)OR(95%CI)P Value OR Adjust(95%CI)P Value Adjust AR vs AS A>A80(34.8)5(13.90)1.00771.0058
A>T-T>T150(65.2)31(86.1) 3.31(1.24-8.83) 3.47(1.29-9.34)
AR vs semi-AR A>A63(38.9)5(13.9)1.00241.0022
A>T-T>T99(61.1)31(86.1) 3.95(1.46-10.68) 4.03(1.48-10.96)
Abbreviations:OR,odds ratio;CI,confidence interval;AR,aspirin resistance;AS,aspirin sensitivity;MAF,minor allele frequency.NCBI,National Center for Biotechnology Information.
518Clinical and Applied Thrombosis/Hemostasis19(5)
Discussion
There are plenty of reports about genetic susceptibility to AR.Genetic variants of uridine 5’-diphosphate-glucuronosyltrans-ferase (UGT1A6),cytochrome P4502C9(CYP2C9),acyl-CoAsynthetase medium-chain family member 2(ACSM2),COX-1,COX-2,platelet glycoproteins GPI a ,GPIb a ,GPIIIb a ,ADP platelet receptors P2RY 1and P2RY 12,coagulation factor XIII (FXIII ),and TXA 2receptor have been reported in AR.13-17How-ever,the results are poorly reproducible perhaps due to race and different diagnostic methods.To improve the diagnostic specificity of AR,AA-induced LTA combined with ADP-induced LTA was therefore used for this study.
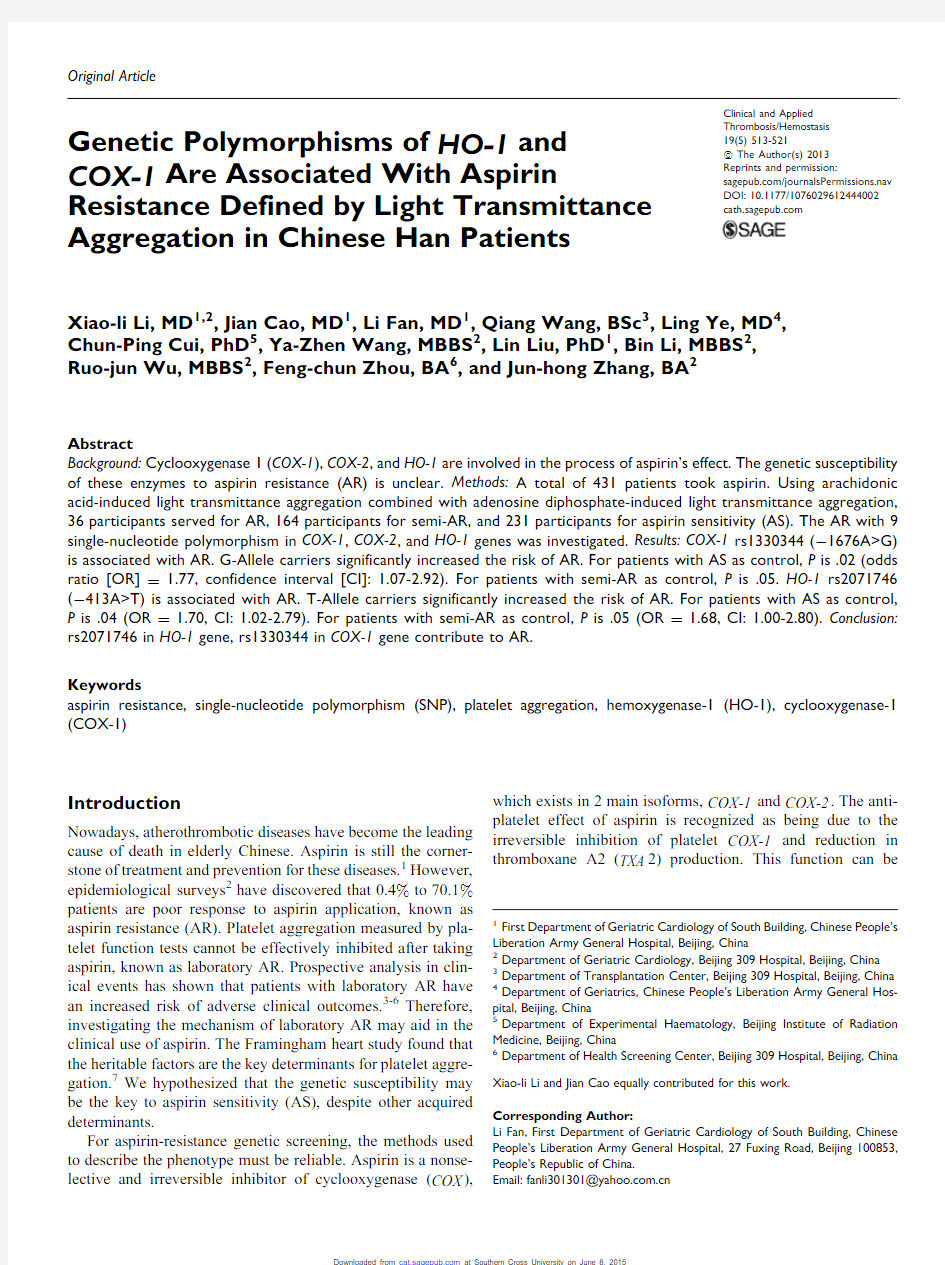
Platelet aggregation at the sites of atherosclerotic plaque plays a role in the thrombosis.COX-1,COX-2,and HO-1are overexpressed in atherosclerotic lesions,mainly by macro-phages and endothelial cells 18,19and are involved in the process of arterial thrombosis.Due to the lack of a nuclear structure in platelets and the inducible expression properties of HO-1and COX-2,platelets do not generate COX-2and generate trace HO-1in the adult.20The COX-1,COX-2,and HO-1are all target molecules of aspirin.The difference is that COX-1is constitutively expressed in many tissues and cells
including platelets.The sites of action of aspirin on COX-2were deduced to be in the vascular wall,especially in athero-sclerotic plaques (Figure 1).The present study aimed to deter-mine whether previously identified SNPs of COX-1,COX-2,and HO-1are associated with laboratory AR,which was diag-nosed through platelet function test methods in vitro.
The highly conserved COX-1gene serves as house-keeping gene and the function is important to life.The human COX-1gene encodes more than 20SNPs,and most of them are rare.21The COX-1gene polymorphisms are of potential importance because individual SNPs or their haplotypes may affect the action of the enzyme as well as its interaction with aspirin.22We investigated 6common SNPs of COX-1and found that the rs1330344(à1676A>G)polymorphism of the COX-1gene promoter and COX-1haplotype are significantly associated with the development of AR.The promoter à1676G allele appears to contribute significantly to an AR haplotype.The other 5SNPs are rare in Chinese Han population.The genetic differences associated with AR significantly vary with race.Data from a review by Agu ′ndez et al suggested that the alleles of COX-1associated with AR are rs3842787and rs5789for European individuals and rs3842789and rs3842792for
Table 6.COX-1Haplotype Responses to Aspirin Resistance.
rs1888943
rs1330344
rs3842787
rs5787rs5789rs5794Case,Control Freq.
OR (95%CI)P -Value AR vs AS C A C G C G 0.472,0.6131
.032C G C G C G 0.528,0.383 1.69(1.05-2.71)AR vs semi-AR
C A C G C G 0.472,0.5951
.044
C
G
C
G
C
G
0.528,
0.393
1.72(1.02-
2.92)
Abbreviations:OR,odds ratio;CI,confidence interval;AR,aspirin resistance;AS,aspirin
sensitivity.
Figure 1.Effects of aspirin via HO-1,COX-1,and COX-2pathways on platelet aggregation.HO-1indicates hemoxygenase-1;COX-1/2:cyclooxygenase-1/2.
Li et al
519
African individuals.13Our research shows that rs1330344has a high prevalence in the Chinese population.The frequency of the minor allele,à1676G is0.40.The GG homozygosity is associated with AR and occurs in17.67%of the Chinese Han population(Table3).In the Japanese population,rs1330344 is also highly prevalent,theà1676C allele has a protective function against functional dyspepsia in Japanese women23 andà676A is a risk factor for aspirin-induced peptic ulcer in Japanese.24On the other hand,the T-1676C promoter poly-morphism was reported to be essential for COX-1transcription. It is,therefore,proposed that G-allele carriers upregulate COX-1expression and that low-dose aspirin may be an ineffec-tive therapy for GG homozygotes.Another SNP of COX-1, rs3842787(C50T),which demonstrates complete linkage dise-quilibrium with the other polymorphism A-842G,is found with minor frequency in Caucasians(8.6%).The C50T Pr –Leu allele, which is present in the signal peptide at position17,has been depicted as a determinant of pharmacological response to aspirin treatment.However,our study showed the frequency of the minor allele in rs3842787(50C>T),which was markedly lower(0.2%)in Chinese than in Caucasians.The same result was reported in the Japanese.In our study,the frequency of the minor allele in rs5789(709C>A)was also markedly lower (0%).Moreover,between the Chinese and Japanese popula-tions,the gene differences for COX-1are highly consistent. Thus,rs1330344may be a common tag SNP in COX-1gene associated with aspirin resistance in Asians.
Unlike COX-1,COX-2is an induced enzyme,and COX-2 messenger RNA and protein synthesis are induced in a time-and dose-dependent manner in inflammation by endothelial cells and macrophages.Atherosclerosis is now understood to be a disease characterized by inflammation,with chronic inflammation involved at every stage,from initiation to pro-gression and,eventually,plaque rupture.25Aspirin is known to exert its anti-inflammatory effects via COX-2.A study by Patrignani et al26found that COX-2is not involved in throm-boxane biosynthesis by activated human platelets and conse-quently argue against the involvement of COX-2-dependent pathway in AR.Our results showed that2common genetic var-iations rs5277and rs20417in COX-2gene are not associated with AR in the Chinese Han population.The rs5277is also a tag SNP for COX-2,as aspirin is a weak COX-2inhibitor and the low-dose aspirin perform antiplatelet effect than anti-inflammation.So we deduced that COX-2gene may not con-tribute to the pathogenesis of AR in Chinese Han population.
Similar to COX-2,HO-1is the inducible enzyme that is ubi-quitously distributed in mammalian tissues and is upregulated by diverse stimuli,which include inflammatory cytokines and factors that promote oxidative stress.Recent studies have found that HO-1is a target in the mediation of aspirin-dependent cytoprotective and anti-inflammatory effects.27-29The HO-1 is the rate-limiting enzyme in the oxidative degradation of heme to biliverdin,free iron,and carbon monoxide.The effects of HO-1are mediated by its metabolites.30The HO-1plays an important role in many aspects of human physiology as well as in pathological events such as atherosclerosis.Reports have demonstrated that the c-Jun N-terminal kinase/activator protein-1(AP-1)signaling pathway is crucially involved in the anti-inflammatory mechanism of HO-1associated with aspirin27and that the cytoprotective action of HO-1associated with aspirin is mediated by the nitric oxide/Cyclic Guanosine Monophosphate(NO/cGMP).system in the endothelium.31 Aspirin induces HO-1expression in endothelial cells in a COX-independent manner.28In2004,Peng et al showed that the induction of HO-1expression inhibited platelet-dependent thrombosis through its metabolite.Our study sug-gests that HO-1has an impact on platelet aggregation and that a genetic polymorphism is associated with AR.
Studies have shown that the major mammalian stress-responsive transcription factors,heat-shock factor,nuclear factor-erythroid2,AP-1,and the nuclear factor-k B family mem-bers,all regulate the HO-1gene through binding with the sites located within the HO-1promoter region and increase HO-1 transcription.32,33These findings suggest that the structure of the promoter region is vital to gene expression of HO-1.Determin-ing the association between HO-1polymorphism and AR was a focus of this study.At present,2functional polymorphisms in the HO-1promoter region,a(GT)n microsatellite and rs2071746(à413T>A)can regulate transcription capability of HO-1.33Both a short(GT)n allele and the A-allele have been associated with increased HO-1promoter activity.Our data for the first time have shown that AT and TT genotypes of the HO-1promoter polymorphism rs2071746(à413A>T)are asso-ciated with susceptibility to AR.In fact,gene changes in the HO-1promoter that impact on aspirin responsiveness are not unique;many studies have demonstrated their impact in a variety of disease states,such as CAD,Alzheimer disease,Parkinson disease,cancer,organ transplantation,infection,diabetes mel-litus,autoimmune disorder,and acute respiratory distress syn-drome.We presume that more evidence will be discovered about the associations of the HO-1gene polymorphism and dis-ease,owing to the property of HO-1being a ubiquitous cell-defensive enzyme.The HO-1seems to be an integral part of the stress response,34and the failure to respond to stressful stimuli via HO-1induction leads to increased susceptibility to diseases. Conclusion
We examined the association of genetic polymorphisms with laboratory aspirin resistance determined by AA-induced LTA combined with ADP-induced LTA.Our study demonstrated for the first time that rs2071746(à413A>T)gene polymorphism in HO-1and rs1330344(à1676A>G)gene polymorphism in COX-1are significantly associated with AR in the elderly Chi-nese Han population.The rs1330344is a fairly common allele in the Han population.We were unable to find an association with a COX-2polymorphism.These findings may guide aspirin antithrombotic therapy in China.
Declaration of Conflicting Interests
The author(s)declared no potential conflicts of interest with respect to the research,authorship,and/or publication of this article.
520Clinical and Applied Thrombosis/Hemostasis19(5)
Funding
The author(s)disclosed receipt of the following financial support for the research,authorship and/or publication of this article:supported by the Healthcare Fund(07BJZ01)and the National Science and Technology Support Project(2009BAI86B04).
References
1.Baigent C,Blackwell L,Collins R,et al.Aspirin in the primary
and secondary prevention of vascular disease:collaborative meta-analysis of individual participant data from randomised https://www.360docs.net/doc/b56474828.html,ncet.2009;373(9678):1849-1860.
2.Rafferty M,Walters MR,Dawson J.Anti-platelet therapy and
aspirin resistance clinically and chemically relevant?Curr Med Chem.2010;17(36):4578-4586.
3.Feher G,Feher A,Pusch G,et al.Clinical importance of aspirin
and clopidogrel resistance.World J Cardiol.2010;2(7):171-186.
4.Bhatt DL.Aspirin resistance:more than just a laboratory curios-
ity.J Am Coll Cardiol.2004;43(6):1127-1129.
5.Krasopoulos G,Brister SJ,Beattie WS,et al.Aspirin‘‘resistance’’
and risk of cardiovascular morbidity:systematic review and meta-analysis.BMJ.2008;336(7637):195-198.
6.Snoep JD,Hovens MM,Eikenboom JC,et al.Association
of laboratory-defined aspirin resistance with a higher risk of recur-rent cardiovascular events:a systematic review and meta-analysis.
Arch Intern Med.2007;167(15):1593-1599.
7.O’Donnell CJ,Larson MG,Feng D,et al.Genetic and environ-
mental contributions to platelet aggregation:the Framingham heart study.Circulation.2001;103(25):3051-3056.
8.Sneader W.The discovery of aspirin:a reappraisal.BMJ.2000;
321(7276):1591-1594.
9.Frelinger A,Furman MI,Linden MD,et al.Residual AA-induced
platelet activation via an adenosine diphosphate-dependent but COX-1-and COX-2-independent pathway:a700-patient study of aspirin resistance.Circulation.2006;113(25):2888-2896. 10.Peng L,Mundada L,Stomel JM,et al.Induction of heme
oxygenase-1expression inhibits platelet-dependent thrombosis.
Antioxid Redox Signal.2004;6(4):729-735.
11.Gurbel P,Bliden K,DiChiara J,et al.Evaluation of dose-related
effects of aspirin on platelet function:results from the Aspirin-Induced Platelet Effect(ASPECT)study.Circulation.2007;
26(115):3156-3164.
12.Gabriel S,Ziaugra L,Tabbaa D.SNP genotyping using the Seque-
nom MassARRAY iPLEX platform.Curr Protoc Hum Genet.
2009;2:2.12.
13.Agu′ndez JA,Mart?′nez,Pe′rez-Sala D,et al.Pharmacogenomics in
aspirin intolerance.Curr Drug Metab.2009;10(9):998-1008. 14.Lev EI,Patel RT,Guthikonda S,et al.Genetic polymorphisms of
the platelet receptors P2Y(12),P2Y(1)and GP IIIa and response to aspirin and clopidogrel.Thromb Res.2007;119(3):355-360.
15.Szczeklik A,Musia?J,Undas A,et al.Aspirin resistance.
J Thromb Haemost.2005;3(8):1655-1662.
16.Fujiwara T,Ikeda M,Esumi K,et al.Exploratory aspirin resis-
tance trial in healthy Japanese volunteers(J-ART)using platelet aggregation as a measure of thrombogenicity.Pharmacogenomics J.2007;7(6):395-403.17.Oh SH,Kim YH,Park SM,et al.Association analysis of thrombox-
ane A synthase1gene polymorphisms with aspirin intolerance in asthmatic patients.Pharmacogenomics J.2011;12(3):351-363. 18.Song J,Sumiyoshi S,Nakashima Y,et al.Overexpression of heme
oxygenase-1in coronary atherosclerosis of Japanese autopsies with diabetes mellitus:Hisayama study.Atherosclerosis.2009;
202(2):573-581.
19.McGeer PL,McGeer EG,Yasojima K.Expression of COX-1and
COX-2mRNA in atherosclerotic plaques.Exp Gerontol.2002;
37(7)925-929.
20.Nowell SA,Leakey JE,Warren JF,et al.Identification of
enzymes responsible for the metabolism of heme in human plate-lets.J Biol Chem.1998;273(50):33342-33346.
21.Maree AO,Curtin RJ,Chubb A.Cyclooxygenase-1haplotype
modulates platelet response to aspirin.Thromb Haemost.2005;
3(10):2340-2345.
22.Goodman T,Sharma P,Ferro A.The genetics of aspirin resis-
tance.Int J Clin Pract.2007;61(5):826-834.
23.Arisawa T,Tahara T,Shibata T,et al.Genetic polymorphisms of
cyclooxygenase-1(COX-1)are associated with functional dyspep-sia in Japanese women.J Womens Health.2008;17(6):1039-1043.
24.Arisawa T,Tahara T,Shibata T,et al.Association between
genetic polymorphisms in the cyclooxygenase-1gene promoter and peptic ulcers in Japan.Int J Mol Med.2007;20(3):373-378.
25.Eldika N,Yerra L,Chi DS,et al.Atherosclerosis as an inflammatory
disease:implications for therapy.Front Biosci.2004;9:2764-2777.
26.Patrignani P,Sciulli M,Manarini S,et al.COX-2is not involved
in thromboxane biosynthesis by activated human platelets.J Phy-siol Pharmacol.1999;50(4):661-667.
27.Fu¨rst R,Blumenthal SB,Kiemer AK,et al.Nuclear factor-kappa
B-independent anti-inflammatory action of salicylate in human endothelial cells:induction of heme oxygenase-1by the c-jun N-terminal kinase/activator protein-1pathway.J Pharmacol Exp Ther.2006;318(1):389-394.
28.Grosser N,Abate A,Oberle S,et al.Heme oxygenase-1induction
may explain the antioxidant profile of aspirin.Biochem Biophys Res Commun.2003;308(4):956-960.
29.Pae HO,Lee YC,Chung HT.Heme oxygenase-1and carbon mon-
oxide:emerging therapeutic targets in inflammation and allergy.
Recent Pat Inflamm Allergy Drug Discov.2008;2(3):159-165. 30.Stocker R,Perrella MA.Heme oxygenase-1:a novel drug target for
atherosclerotic diseases?Circulation.2006;114(20):2178-2189. https://www.360docs.net/doc/b56474828.html,vrovsky Y,Schwartzman ML,Levere RD,et al.Identification
of binding sites for transcription factors NF-kappa B and AP-2in the promoter region of the human heme oxygenase1gene.Proc Natl Acad Sci USA.1994;91(13):5987-5991.
32.Alam J,Cook JL.How many transcription factors does it take to
turn on the heme oxygenase-1gene?Am J Respir Cell Mol Biol.
2007;36(2):166-174.
33.Exner M,Minar E,Wagner O,et al.The role of heme oxygenase-
1promoter polymorphisms in human disease.Free Radic Biol Med.2004;37(8):1097-1104.
34.Levonen AL,Va¨ha¨kangas E,Koponen JK,et al.Antioxidant gene
therapy for cardiovascular disease:current status and future per-spectives.Circulation.2008;117(16):2142-2150.
Li et al521
关于阿司匹林抵抗的研究论文
关于阿司匹林抵抗的研究论文 1.1阿司匹林抵抗的定义 Bhatt[2]等将阿司匹林抵抗分为临床性及生化性。临床性为患者口服阿司匹林后仍发生缺血性血管疾病;生化性为口服阿司匹林后,未能改变血小板功能试验结果。有研究[3]将生化性阿司匹林抵抗分为3型:(1)Ⅰ型阿司匹林抵抗(药动学型):口服同样剂量的阿司匹林,体内血栓素(TX)合成和胶原诱导血小板聚集均未被抑制。而体外富血小板血浆中加入100μmol/L阿司匹林后可被抑制,提示使用小剂量阿司匹林有相当大的药动学差异。(2)Ⅱ型阿司匹林抵抗(药效学型):无论体内及体外,口服阿司匹林后,TX合成和胶原诱导血小板聚集均未被抑制,提示该型阿司匹林抵抗的机制与环氧化酶(COX)的遗传多态性有关。(3)Ⅲ型阿司匹林抵抗(假性阿司匹林抵抗):口服阿司匹林后能抑制TX合成,但不能抑制胶原诱导的血小板聚集。该型患者之所以被冠以“假性抵抗”,因为阿司匹林已抑制了TX合成,而不能抑制其他物质如胶原诱导的血小板聚集。 2阿司匹林抵抗机制 大量证据表明,GP受体多态性是动脉血栓形成的遗传危险因素,它能造成黏附受体成分的表达、功能和免疫遗传学的多样性。血小板激动剂(如TXA2)通过细胞内信号激活GPⅡb/Ⅲa受体,介导纤维蛋白原及其受体结合,然后促进血小板聚集。阿司匹林通过干扰COX非依赖性细胞内信号转导并使GPⅡb和GPⅢa 分子乙酰化来抑制GPⅡb/Ⅲa的活化。尽管还未完全弄清,但目前所知的COX 非依赖性信号转导途径可能包括跨膜蛋白受体、磷脂酶、Ca2+释放、腺苷酸环化酶、鸟苷酸环化酶和蛋白激酶C等。某些弱的激动剂(如ADP、肾上腺素和胶原
阿司匹林“抵抗”及处理策略
阿司匹林“抵抗”及处理策略 北京大学人民医院刘靖 一、阿司匹林是心脑血管疾病预防及治疗的基石 心脑血管疾病在全球范围内已形成流行趋势,极大程度地威胁公众健康,并带来严重的社会负担。50年代末至今,我国心脑血管疾病发病率上升了4倍,占全年死亡人口的1/3。据估计,每年由此造成的医疗费用,心肌梗死和脑卒中分别高达19亿和196亿元。因此,积极控制危险因素,选用安全、有效、经济的药物,是减少死亡、降低医疗费用的关键。WHO指南指出,心脑血管病的预防应以所有人群和高危人群相结合的策略。简单有效的预防方法,包括联合应用阿司匹林,就可以控制50%的致死或致残率。 阿司匹林的抗血小板作用被发现至今已近40年,大量的研究奠定了阿司匹林在心脑血管疾病防治中的基石地位。新近的抗栓试验协作组(ATC)汇总分析显示,阿司匹林使心肌梗死、脑卒中等高危患者的血栓性血管事件和非致死性卒中分别减少四分之一,非致死性心肌梗死减少三分之一,血管性死亡减少六分之一。阿司匹林的抗栓效果显而易见。然而仍有部分服用阿司匹林的患者会出现血管事件。针对这种现象,一些学者提出了阿司匹林“抵抗” (Aspirin Resistance)的概念。
二、阿司匹林“抵抗”的定义 阿司匹林“抵抗”,又被称为“耐药”或“治疗反应变异”等,目前尚无确切而统一的定义。阿司匹林“抵抗”通常用来描述如下两种现象。一是服用阿司匹林不能预防缺血性血管事件的发生,被称作“临床阿司匹林抵抗”。根据ATC的数据,其发生率估计在 10.9%~17.3%之间。阿司匹林“抵抗”也被描述为针对一种或多种血小板功能试验,阿司匹林无法产生预期效应,如抑制血栓素的生物合成等,被称作“生化阿司匹林抵抗”。根据不同的研究人群和所采用的血小板功能测定方法,其发生率估计在5%~20%之间。 关于阿司匹林“抵抗”的实验室检测,目前尚无公认的方法。主要采用测定皮肤出血时间、光镜下检测或采用血小板功能分析仪PFA-100检测血小板聚集力及通过尿中的血栓素排泄产物反映体内血栓素生成情况等,但由于特异性、敏感性、与临床的相关性不确定,以及可重复性差等原因,未广泛应用于临床。 大家比较关注“临床”与“生化”阿司匹林“抵抗”之间有无关联。实际上,针对这一问题已进行了大量的研究。但迄今为止,仅有2002年Eikelboom和2003年Gum等报道的两项研究显示阿司匹林“抵抗”与临床预后有一定的关系。这两项研究中,前者是回顾性研
阿司匹林抵抗及治疗
阿司匹林抵抗及治疗策略 【关键词】阿司匹林抵抗;应对策略;心脑血管病 阿司匹林自1897年问世以来已在临床应用100多年,当初只是用作解热、镇痛和消炎,20世纪70年代后发现其抗血小板作用以后,便广泛应用于心脑血管疾病的二级预防及某些病人的一级预防。阿司匹林是缺血性心脑血管疾病治疗领域中抗血小板药物的基石,大量循证医学证据表明,阿司匹林用于心脑血管疾病高危患者,可使多数心脑血管病事件大幅降低[1]。然而,阿司匹林的抗血小板作用存在着个体差异,在口服常规剂量(75~325mg/d)的患者中,有部分患者无明显疗效,仍发生血栓栓塞事件,这些患者可能存在阿司匹林抵抗(AR),其发生率约5%~45%[2]。 1 阿司匹林抵抗 阿司匹林抵抗(aspirin resistance,AR),是指阿司匹林不能预防血栓形成事件的发生,或不能有效抑制血小板聚集和血栓素形成的一种现象。AR具有三方面的意义:第一、阿司匹林不能保护患者免于血栓性并发症;第二、不能使出血时间延长;第三、不能在体外抑制血小板聚集或不能抑制血栓烷的形成。目前用来评价AR的实验技术虽然较多,但尚未形成规范。当前采用最多的是AR定义为符合下列3条标准中2或3条:(1)快速血小板功能分析仪所测ASA得分≥500;(2)5μmol/L二磷酸腺苷(ADP)诱导的血小板聚集≥70%;(3)0.5mg/ml花生四烯酸诱导的血小板聚集≥20%。AR可诱导不良心脑血管病事件,因此对于AR者应高度重视。 2 阿司匹林抵抗的应对策略 AR的发生率相对较高,多存在于缺血性心脑血管疾病二级预防病例中,如不及时发现并加以治疗,则很有可能酿成恶果。对于已经出现AR的人群,应联合其他抗血小板药物或以其他药物替代。但其他抗血小板聚集药物也存在着类似AR的现象,如氯吡格雷抵抗。在防治缺血性血管病事件中,COX-1一直被用做阿司匹林作用的靶部位,而现在看来仍然不够,巨噬细胞中COX-2也应成为干预的目标。此外,为了延缓动脉粥样硬化的进程或减少血栓事件,TP受体拮抗剂也是一种十分重要的治疗手段。因此,未来较为理想的治疗方案可能是COX-2与TP受体拮抗剂的联合应用,这一方面避免了阿司匹林抵抗现象的发生,同时在防治动脉粥样硬化方面也更加有效。另外,在处理AR方面还需要注意患者个体的情况,如年龄、性别、体重指数、手术、血红蛋白水平、高脂血症、精神紧张、吸烟、冠心病、非类固醇类抗炎药(如布洛芬等)、应激及阿司匹林的剂量等有关[3]。对血小板更新频率快的患者可考虑大剂量给药,给药方式可实行晚上给药,或间断给予大剂量阿司匹林用药,也可选用血小板ADP受体拮抗剂氯吡格雷,以减少AR现象,并发挥抗血小板效应。AR 可伴氯吡格雷抵抗。美国休斯顿Methodist DeBakey心脏中心LeV等报告AR者可伴发存在氯吡格雷抵抗,因而使此类患者在经皮冠脉介入术(PCI)后发生血栓栓塞事件的危险增加。该中心研究结果显示阿司匹林与氯吡格雷双重抵抗为26.9%,双重抵抗的最可能机制是血小板应性全面增加,这提示应该引起警惕的是一部分接受高危PCI的患者即使已经给予了阿司匹林和氯吡格雷双重抗血小板治疗,但仍可能不具有抗凝保护作用,因而这类患者为发生血栓栓塞事件的高危人群。对于这类患者,在环氧化酶-1(COX-1)抑制剂(如阿司匹林)和P2Y12拮抗剂(如氯吡格雷)之外,作用于其他位点的抗血小板药物可能会有所裨益。AR替代药物包括噻氯匹啶、潘生丁加用阿司匹林或者华法令加阿司匹林,或加用氯吡格雷等。不管如何应用抗血小板制剂,均应重视其效果。 【参考文献】 1 中华医学会心血管病分会、中华心血管病杂志编委会.阿司匹林在动脉硬化性心血管疾病中的应用:中国专家共识(2005).中华心血管病杂志,2006,34(3):281.
阿司匹林抵抗的概念及其临床意义
阿司匹林抵抗的概念及其临床意义 阿司匹林在防治血栓栓塞性血管疾病方面有着广泛的应用。抗血小板试验协作组(Antip latelet Trialists Collaboration)认为,阿司匹林用于心脑血管疾病高危患者,可分别使心脑血管病事件如死亡、心肌梗死(MI)或卒中降低25%,冠状动脉搭桥及动脉栓塞事件降低48%,肺栓塞减少67%,深静脉血栓形成减少23%。 然而阿司匹林的抗血小板作用存在着个体差异。有的患者尽管长期服用常规剂量(75~325mg/d)的阿司匹林,但实验室检测发现其血小板聚集能力未被很好地抑制,有的患者仍发生血栓栓塞事件;这些患者可能存在阿司匹林抵抗(aspirin resistance,AR),前者称为生化阿司匹林抵抗,后者称为临床阿司匹林抵抗。 临床阿司匹林抵抗(Clinical Aspirin Resistance)指阿司匹林不能使患者免于缺血性心血管病事件,临床表现为在服用阿司匹林情况下仍然发生了心血管病事件。生化阿司匹林抵抗(Biochemical Aspirin Resistance)指服用阿司匹林后不能引起血小板功能试验的预期改变:①延长出血时间;②抑制血栓素A2(TXA2)的生物合成;或③在体外对血小板功能检测指标产生预期的影响。 根据临床阿司匹林抵抗的定义,如果不发生阿司匹林抵抗,患者只要服用阿司匹林,就不会发生心血管病事件之虞;按照这一定义,阿司匹林抵抗发生率≥75%(汇总分析显示,阿司匹林减少心血管病事件20%~25%),然而事实是心血管疾病的发生发展涉及诸多的因素,阿司匹林治疗只能减少、而不可能根绝心血管病事件,而且根据被研究人群的临床特点、样本数量和随访时间长短,“临床阿司匹林抵抗”的发生率可以从0~100%不等。因此临床阿司匹林的定义缺乏临床意义。 临床阿司匹林抵抗可能与血小板激活的替代途径、阿司匹林对血栓素的生物合成不敏感、药物间的相互作用以及阿司匹林剂量过低、同时服用与阿司匹林有不利相互作用的药物如布洛芬、血小板加速更新、血小板组分或花生四烯酸代谢酶的基因多态性、非动脉粥样硬化因素引起心血管病事件等因素相关。到目前为止,很难用某一种机制解释清楚所有的AR 现象,但不可否认的是,AR存在一定的群体特征,也就是在不同的人群当中,不同的原因可能导致相同的特征结果。 生化阿司匹林抵抗,因目前大多数试验缺乏特异性,未针对阿司匹林的作用机制,“生化阿司匹林抵抗”发生率变化太大,令人无所适从,体外进行的试验其结果是否与体内实际发生的血小板聚集或抑制状态相关,目前并不清楚。目前用来评价阿司匹林及其他抗血小板药物的实验技术虽然较多,但尚未形成规范,达成共识的检测方法和技术更少。 有临床使用价值的实验室指标必须具备以下特点:有统一公认的检测方法和评价标准;前瞻性研究证实其与发生心血管病事件独立相关;随机试验显示逆转异常指标能显著改善临床转归;评价生化阿司匹林抵抗的现有血小板功能试验,无一具备上述任一特点,因此均无肯定临床实用价值。 目前阿司匹林抵抗概念的临床意义仍有待进一步明确,根据2005年中国专家共识,建议阿司匹林用于抗血小板治疗获益/风险比良好的所有临床情况,长期使用阿司匹林的剂量为100mg/d(75~150mg/d),阿司匹林价格低、使用方便、疗效确切,应当进一步加大宣传,在有适应证的人群中尽量提高应用率,减少心脑血管事件发生率。
阿司匹林用药指导的基因检测
阿司匹林用药指导的基 因检测 集团企业公司编码:(LL3698-KKI1269-TM2483-LUI12689-ITT289-
阿司匹林用药指导的基因检测 (阿司匹林抵抗基因筛查) 阿司匹林是治疗急性冠状动脉综合征和经皮冠状动脉介入术后抗栓的基础药物,广泛应用于心脑血管疾病一级和二级预防。临床发现部分患者尽管长期低剂量服用阿司匹林仍不能有效抑制血小板的活性,即阿司匹林抵抗,其发生率约50%~60%且存在明显种族差异性。研究表明,基因多态性在阿司匹林抵抗中起着重要作用,主要集中在 GPIIIaP1A1/A2、PAI-14G/5G和PEAR1基因多态性。GPIIIaP1A2是阿司匹林抵抗主要基因,该基因突变使得GPIIb/IIIa受体结构发生改变,使血小板之间发生交叉连接,导致血小板聚集。研究发现,发生阿司匹林抵抗患者携带P1A2等位基因的频率明显高于阿司匹林敏感患者,且P1A2/A2纯合突变型患者服用阿司匹林后疗效均不良。携带突变型P1A2等位基因患者行支架术后,其亚急性血栓事件发生率是P1A1纯合野生型患者的5倍,需要更高剂量的阿司匹林才能达到抗凝效果。PAI-1是血浆中组织纤溶酶原激活物的主要抑制剂,PAI-1基因研究较多是PAI-14G/5G插入或缺失多态性。4G等位基因与PAI-1血浆水平升高有关,导致血小板聚集趋势增加,导致心肌梗死和冠心病发生风险增加,携带4G 等位基因的患者比5G心肌梗死风险高5倍,需要更高剂量的阿司匹林。PEAR1GG等位基因对阿司匹林应答好,AA或AG基因型患者支架植入术后服用阿司匹林(或结合氯吡格雷),其心肌梗死和死亡率高。因此,建议在使用阿司匹林前检测GPIIIaP1A1/A2、PAI-14G/5G和PEAR1,临床药师将针对患者基因型对患者进行疗效预测,并对高风险患者提前干预,以降低患者用药风险,保障临床用药安全、有效。 该项目收费为1200元(医保、新农合报销),每个患者只需检测1次即可。临床医生可按照相应流程提出检测申请,并采用EDTA抗凝真空采血管(紫色帽头)采集外周静脉血2ml(无需空腹,无论是否用药,随时抽取血标本),检测人员将在2个工作日内出具基因检测报告,并提供个体化给药建议供临床参考。 目前我院在用的阿司匹林:
阿司匹林精准治疗指南
阿司匹林的精准治疗20150425 阿司匹林单药,用于心血管疾病的二级预防; 阿司匹林与氯吡格雷或替格瑞洛联用,用于预防心脑血管支架血栓的发生等。
一、阿司匹林基因位点: 1、GPIIIaPlA1/A2 2、PEAR1 3、PTGS1 4、GP1BA 5、GSTP1 6、LTC4S 二、警告: 1、LTC4S:AC、CC基因型,使用阿司匹林发生荨麻疹的风险较高。建议不用阿司匹林。 2、GSTP1:GG和AG型,使用阿司匹林,消化道出血风险较高,建议不用阿司匹林。 3、易出血人群,消化系统溃疡史,活动性消化性溃疡,肝肾功能衰竭,痛风患者禁用阿司匹林 4、妊娠期后三个月禁用。 5、同时使用其他非甾体抗炎药物,激素类药物,大剂量维生素C会加重粘膜刺激造成出血等不良反 应。 6、服药期间禁止饮酒或摄入酒精。 三、出具个体化治疗报告时,还应注意: 阿司匹林个体化治疗,在临床常面临以下情况: 报告结尾,还应写明以下两点: 1、应关注药物相互作用等因素的影响。 2、本结论仅根据基因检测结果和循证医学证据得出,具体用药方案,尚需结合患者血小板反应等 具体情况综合判断。
四、阿司匹林单药个体化治疗建议(心血管疾病二级预防): 1、在无阿司匹林抵抗的前提下,可使用常规剂量阿司匹林治疗,但需高度关注出血风险。尤其是 消化系统出血(应根据既往史、GSTP1基因及临床反应判断)。 2、如存在出血高危因素(如既往出血史、GSTP1基因的GG和AG型、严重贫血、血小板数量和功能降 低、低白蛋白血症或低凝血因子血症者),则: (1)换用其他抗血小板药物,如氯吡格雷(但需关注不同基因型对氯吡格雷药效的影响),或换用双嘧达莫; (2)联合使用增强胃黏膜屏障功能的药物,如米索前列醇等或使用H2受体阻断剂如法莫替丁或PPI类药物(如患者使用氯吡格雷应建议使用雷贝拉唑)。 3、上述结论仅根据基因检测结果和循证医学证据得出,具体用药方案,尚需结合患者血小板反应等具体情况综合判断。 五、阿司匹林联合用药个体化治疗建议 (一)如基因未发生突变,可按正常剂量使用。 (二)如发生突变尤其为突变纯合型 1、GP IIIa Pl A2(T > C)CC基因型,行支架术后,其亚急性血栓事件发生率是TT型的5倍,需要增加阿司匹林剂量才能达到抗凝效果。但由于高剂量阿司匹林会增加出血风险,一旦出血,可能会被认为是用药不当,故首选建议换用标准剂量的双嘧达莫。若抗血小板强度不足,可加用西洛他唑,行双抗治疗。应联合使用增强胃黏膜屏障功能的药物,如米索前列醇等或使用H2受体阻断剂如法莫替丁或PPI类药物。建议同时关注血小板凝集等数据。(首选PPI类药物) 2、PEAR1 (G>A):GG等位基因对阿司匹林抗血小板应答好; GA型可使用单应密切关注血小板等检测,如抵抗,及时调整方案AA基因型,用阿司匹林心梗和死亡率高可换用双嘧达莫。如仍不能达到抗凝效果可加用西洛他唑进行双联治疗。 3、PTGS1(-842A>G):PTGS1:GG基因型,阿司匹林抵抗风险高(HR:10),心血管事件发生率高(HR:2.55)。AG基因型风险中等应密切关注阿司匹林治疗效果;AA基因型阿司匹林较敏感,心血光事件发生率较低。如发生突变建议同上。 4、GP1BA:CC基因型,阿司匹林抵抗风增加;CT和TT型,抵抗风险降低。发生突变用药建议同上 5、GSTP1:GG和AG型,使用阿司匹林,消化道出血风险,是AA型的2.08倍如发生基因突变应在长期使用阿司匹林时应同时服用PPI类药物,以预防消化系统出血。 6、LTC4S:AA基因型,使用阿司匹林发生荨麻疹的风险较AC,CC型低。突变患者应注意药源性皮疹的发生。 六、个体化建议格式及顺序 1. 首先确定患者基因类型,个体情况如年龄,病史,出血风险等等。综合评判患者阿司匹林应答水平如何,如上述“五(二)之1、2、3、4”项中有突变型,则首选建议更换双嘧达莫进行抗凝治疗,如使用阿司匹林建议上调100-200mg但应注意出血风险,可配伍PPI等药物进行消化系统粘膜保护。 2.确定患者5 6项中的出血风险及皮疹风险。如出血高风险即使正常剂量长期使用仍应建议配伍PPI 类等药物或提示患者高度关注出血风险。 3.确认患者服药期间不服用其他造成不良反应的药物或服用其他易造成出血的抗血凝类药物。 4.在治疗期间检测血小板聚集率或血栓弹力图来进一步评价抗血小板疗效。高危患者应较普通患者缩短血液检测间隔,以确定治疗效果。 5、上述结论仅根据基因检测结果和循证医学证据得出,具体用药方案,尚需结合患者血小板反应等具体情况综合判断。
阿司匹林用药指导的基因检测
阿司匹林用药指导的基因检测 (阿司匹林抵抗基因筛查) 阿司匹林是治疗急性冠状动脉综合征和经皮冠状动脉介入术后抗栓的基础药物,广泛应用于心脑血管疾病一级和二级预防。临床发现部分患者尽管长期低剂量服用阿司匹林仍不能有效抑制血小板的活性,即阿司匹林抵抗,其发生率约50%~60%且存在明显种族差异性。研究表明,基因多态性在阿司匹林抵抗中起着重要作用,主要集中在GPIIIa P1A1/A2、PAI-1 4G/5G和PEAR1基因多态性。GPIIIa P1A2是阿司匹林抵抗主要基因,该基因突变使得GPIIb/IIIa受体结构发生改变,使血小板之间发生交叉连接,导致血小板聚集。研究发现,发生阿司匹林抵抗患者携带P1A2等位基因的频率明显高于阿司匹林敏感患者,且P1A2/A2纯合突变型患者服用阿司匹林后疗效均不良。携带突变型P1A2等位基因患者行支架术后,其亚急性血栓事件发生率是P1A1纯合野生型患者的5倍,需要更高剂量的阿司匹林才能达到抗凝效果。PAI-1是血浆中组织纤溶酶原激活物的主要抑制剂,PAI-1基因研究较多是PAI-1 4G/5G插入或缺失多态性。4G等位基因与PAI-1血浆水平升高有关,导致血小板聚集趋势增加,导致心肌梗死和冠心病发生风险增加,携带4G等位基因的患者比5G心肌梗死风险高5倍,需要更高剂量的阿司匹林。PEAR1 GG等位基因对阿司匹林应答好,AA或AG基因型患者支架植入术后服用阿司匹林(或结合氯吡格雷),其心肌梗死和死亡率高。因此,建议在使用阿司匹林前检测GPIIIa P1A1/A2、PAI-1 4G/5G和PEAR1,临床药师将针对患者基因型对患者进行疗效预测,并对高风险患者提前干预,以降低患者用药风险,保障临床用药安全、有效。 该项目收费为1200元(医保、新农合报销),每个患者只需检测1次即可。临床医生可按照相应流程提出检测申请,并采用EDTA抗凝真空采血管(紫色帽头)采集外周静脉血2ml(无需空腹,无论是否用药,随时抽取血标本),检测人员将在2个工作日内出具基因检测报告,并提供个体化给药建议供临床参考。 目前我院在用的阿司匹林:
阿司匹林抵抗与基因多态性
2012年12月第9卷第35期 ·综述· CHINA MEDICAL HERALD 中国医药导报阿司匹林作为一种有效的抗血小板聚集药,可抑制血小板活化、聚集,防止血栓形成,在心脑血管病的一、二级防治中,起着至关重要的作用。然而,临床发现部分长期服用阿司匹林的患者,心脑血管事件的发生率并未降低,即可能在一定程度上存在阿司匹林抵抗(Aspirin resistance ,AR )现象。目前,AR 的发生机制尚不明确,但新近研究发现,基因多态性与AR 的发生有重要的关系。现对近年来AR 与基因多态性的相关性研究结果作一综述。1AR 定义及分型 Bhatt 等[1]将AR 分为实验室型和临床型。实验室型指虽长期服用常规剂量的阿司匹林(75~325mg ),但实验室检测发现血小板聚集能力未被抑制;临床型指口服阿司匹林,仍发生缺血性心脑血管事件;Gum 等[2]则将10μmol/L ADP 诱导的血小板聚集率超过70%,或0.5mg/mL 花生四烯酸(arachidonic ,AA )诱导的血小板聚集率超过20%作为AR 的实验室诊断标准。 Weber 等[3]应用体内(口服阿司匹林100mg/d 至少5d )和体外试验(体外血浆中加入100μmol/L 阿司匹林),通过联合检测血栓素B 2(thromboxane B 2,TXB 2)浓度与胶原诱导血小板聚集率,将AR 分为三型:①药代动力学型(Ⅰ型):在体内试验中,TXB 2的合成和胶原诱导血小板聚集均未被抑制;而在体外试验中,TXB 2的合成和胶原诱导血小板聚集可被抑制,推测其原因可能与个体间的药代动力学差异有关。②药效学型(Ⅱ型):在体内试验及体外实验中,TXB 2的合成和血小板聚集均未受抑制,可能机制与血小板COX 的基因 多态性有关。③假性抵抗型(Ⅲ型):在体内试验及体外实验中,阿司匹林仅可抑制TXB 2合成,但不能抑制胶原诱导的血小板聚集。 2AR 的作用机制 AR 的作用机制尚未明确,可能与药物剂量不足、肠道吸收能力的差别、非甾体抗炎药的使用、血小板活化路径及基因多态性等多种因素有关。目前,关于血小板活化路径及基因多态性研究结果表明,AR 主要与环氧合酶(cycloxygenase ,COX )、纤维蛋白原受体、ADP 受体和胶原受体、血管性假血友病因子(von wilebrand factor ,vWF )受体等的基因多态性相关。 2.1COX 基因多态性 COX 包括COX-1和COX-2两种亚型。人体COX-1基因位于染色体9q32~9q33.3上,长约22kb ,包含11个外显子,共编码576个氨基酸。研究表明,COX-1基因单核苷酸多态性(single nucleotide polymorphisms ,SNP )可引起碱基替换及启动子连接部位的变化,显著影响内含子或外显子的功能,改变COX-1蛋白的构象,使阿司匹林对COX-1的敏感性不均一,从而影响阿司匹林的抗血小板聚集作用。Maree 等[4]观察144例口服阿司匹林(75~300mg )治疗的爱尔兰心血管病患者2周,采用TaqMan SNP 基因分型检测技术对COX -1基因5个SNPs (rs10306114、rs1236913、rs3842788、rs5788和rs5789)进行基因分型,结果显示单体型A-C-G-C-C 与AA 诱导的AR 密切相关(P =0.004)。Lepantalo 等[5]对101例芬兰动脉血栓疾病患者COX -1基因4个SNPs (rs10306114、rs1236913、rs5788和rs5789)进行检测,经多因素Logistic 回归分析发现,60%伴有AR 的患者携带 阿司匹林抵抗与基因多态性 徐旭陈忠云李晓峰梁国威杨旭▲ 航天中心医院北京大学航天临床医学院神经内科,北京100049 [摘要]阿司匹林作为一种有效的抗血小板聚集药,在心脑血管病防治中方面发挥着重要作用。然而,阿司匹林抗血小板作用个体差异较大,部分患者存在阿司匹林抵抗(Aspirin resistance ,AR ),其发生机制尚未明确。新近研究表明,AR 与环氧合酶、纤维蛋白原受体、ADP 受体和胶原受体等的基因多态性密切相关。因此,基因多态性的检测不仅有助于阐明AR 的发生机制,同时也将为实现个体化治疗策略以及临床转归的评估提供理论基础。[关键词]阿司匹林抵抗;基因多态性;抗血小板聚集[中图分类号]R973.2[文献标识码]A [文章编号]1673-7210(2012)12(b )-0061-03 Aspirin resistance and single nucleotide gene polymorphism XU Xu CHEN Zhongyun LI Xiaofeng LIANG Guowei YANG Xu ▲ Department of Neurology,Aerospace Center Hospital Aerospace Clinical Medical College Affiliated to Peking University,Beijing 100049,China [Abstract]Aspirin is an effective anti-platelet aggregation of medicine which is playing a vital role in the prevention and treatment of cardio cerebral vascular disease.However,there exists individual difference in its anti-platelet effect,Aspirin resistance is presented in some of patients and the occurrence mechanism is still unknown.New clinical trials suggest that Aspirin resistance is closely related to the genetic polymorphism of cycloxygenase,fibrinogen receptor,adenosine diphos -phate receptor,glycoprotein,and so on.Therefore,detection of gene polymorphism not only contributes to the elucidation of the mechanism,but also provides the theory basis to the strategy individualized treatment and clinical outcome.[Key words]Aspirin resistance;Gene polymorphism;Anti-platelet aggregation [基金项目]航天中心医院院级基金资助项目(201210)。 ▲ 通讯作者 61
