艾滋病流行起源的新见解(英文)

Highly divergent subtypes and new recombinant forms prevail in the HIV/AIDS epidemic in Angola:New insights into the origins of the AIDS pandemic
Ine
?s Ba ′rtolo a ,Cheila Rocha a ,Jose ′Bartolomeu b ,Anto ′nio Gama c ,Rute Marcelino d ,Marlene Fonseca e ,Ana Mendes e ,Marta Epalanga b ,Patr?
′cia Cavaco Silva a ,f ,Nuno Taveira a ,d ,f ,*a
URIA,Centro de Patoge
′nese Molecular,Faculdade de Farma ′cia de Lisboa,Portugal b
Servic ?o Nacional de Sangue,Luanda,Angola c
Malongo -Medical Department,Cabinda,Angola d
GenoMed,Instituto de Medicina Molecular,Lisboa,Portugal e
Hospital Militar Principal,Luanda,Angola f
Instituto Superior de Cie
?ncias da Sau ′de Egas Moniz,Monte de Caparica,Portugal 1.Introduction
More than 22.5million people are living with HIV/AIDS in Sub-Saharan Africa,and this accounts for the fastest moving AIDS epidemic worldwide.In 2007,an estimated 1.7million people in the region became newly infected,while 1.6million adults and children died of AIDS (UNAIDS,2007).
Angola is a South-western African country bordered by Republic of Congo,Democratic Republic of Congo (DRC),Zambia
and Namibia.According to the UNAIDS epidemiological fact sheets,2006update,the estimated number of adults and children living with HIV/AIDS in Angola was 320,000,and the number of deaths due to AIDS 30,000(UNAIDS,2006a ).The HIV/AIDS prevalence was 3.7%in the adult population which is very low as compared to Southern Africa countries such as Republic of South Africa (18.8%,2005estimate)(UNAIDS,2006b )yet similar to the neighbouring country DRC (3.2%)(UNAIDS,2006c ).HIV-1prevalence in Angola has been decreasing since 1989as judged by the 6.1%prevalence detected at that time in a major nationwide seroprevalence study (Santos-Ferreira et al.,1990).
HIV-1genetic forms have been divided into three main groups,M (major),O (outlier)and N (new).Among HIV-1group M strains,responsible for the vast majority of HIV infections worldwide,there are 9genetic subtypes (A–D,F–H,J and K),6sub-subtypes
Infection,Genetics and Evolution 9(2009)672–682
A R T I C L E I N F O Article history:
Received 10January 2008
Received in revised form 23April 2008Accepted 6May 2008
Available online 9May 2008Keywords:Angola HIV-1
Molecular epidemiology Subtypes
Recombinants
A B S T R A C T
Angola,located in South-Western Africa,has a remarkably low HIV/AIDS prevalence in the adult population (3.7%).It is bordered in the North by the Democratic Republic of Congo (DRC)and Republic of Congo that are at the origin of human HIV-1infections.It is,therefore,likely that HIV-1strains circulating in Angola are genetically diverse and representative of the origin of the HIV/AIDS epidemic.The aim of this work was to investigate in detail the genetic diversity and molecular epidemiology of HIV-1in Angola.Almost 400sequences were obtained from the gag (p17),pol (PR and RT)and/or env (C2C3)genes of 159HIV-1infected patients living in eight provinces of Angola (Benguela,Cabinda,Cuanza Norte,
Luanda,Lunda Norte,Malange,U?
′ge,and Zaire)and their genotype was determined by phylogenetic analyses.Gene regions representing all HIV-1group M clades were found as well as unclassi?able sequences.In env and pol (RT),two groups of sequences forming distinct sub-clusters within the subtype A radiation were found and may de?ne new A5and A6sub-subtypes.Recombinant forms were found in almost half (47.1%)of the patients of which 36.0%were second-generation recombinants.Fifty-eight different patterns of recombination were found.The A subtype,including CRF02_AG,was represented in most recombinant viruses.Epidemiological data suggests that the AIDS epidemic in Angola has probably started as early as 1961,the major cause being the independence war,and spread to Portugal soon thereafter.The extraordinary degree of HIV-1group M genetic diversity and evolution in Angola may pose unprecedented challenges to diagnostic,treatment and prevention of HIV-1infection.
?2008Elsevier B.V.All rights reserved.
*Corresponding author at:Unidade dos Retrov?′rus e Infecc ?o
?es Associadas,Centro de Patoge ′nese Molecular,Faculdade de Farma ′cia de Lisboa,Avenida das Forc ?as
Armadas,1649-019Lisboa,Portugal.Tel.:+351217934212;fax:+351217986055.
E-mail addresses:ntaveira@mail.telepac.pt ,ntaveira@ff.ul.pt (N.Taveira).Contents lists available at ScienceDirect
Infection,Genetics and Evolution
journal homepage:https://www.360docs.net/doc/e311903465.html,/locate/meegid
1567-1348/$–see front matter ?2008Elsevier B.V.All rights reserved.doi:10.1016/j.meegid.2008.05.003
(A1,A2,A3and A4and F1and F2),37circulating recombinant forms(CRFs)and a variety of unique recombinant forms(URFs) (Los Alamos Sequence Database,2007;McCutchan,2006;Powell et al.,2007a).Second-generation recombinants combining one or more CRFs with different subtypes were?rst identi?ed in patients from Cameroon(Tscherning-Casper et al.,2000)and are becoming common in complex epidemics with multiple subtypes and recombinant forms such as Cuba(Sierra et al.,2007)and Cameroon (Powell et al.,2007a,b).
HIV-1group M arose from SIVcpz infecting the chimpanzee subspecies Pan troglodytes troglodytes in Cameroon,West Central Africa(Keele et al.,2006).The common ancestor of HIV-1group M in humans dates back to the1940s and the beginning of the HIV-1 group M epidemic is estimated to be the1960s(Lemey et al.,2006). However,the factors that have spurred worlwide HIV-1transmis-sion are still unknown.
The global distribution of HIV is complex and dynamic with regional epidemics representing only a subset of the global diversity(Geretti,2006;Buonaguro et al.,2007).HIV genetic forms differ signi?cantly in terms of global prevalence.As expected,the highest genetic diversity is observed in West Central Africa;for example,all HIV-1groups co-circulate in Cameroon(Konings et al., 2006;Luk et al.,2007;Ndongmo et al.,2006).The AIDS epidemic in Western DRC is caused by all HIV-1group M genetic forms (subtypes and recombinants).This epidemic is also characterized by high intra-subtype diversity,high proportion of unique recombinant forms,and a substantial number of genetic forms that cannot be classi?ed into the current subtypes(Kalish et al., 2004;Vidal et al.,2005,2006).High degree of HIV-1genetic diversity is also found in countries with former ties with Central Africa.For instance,the Cuban(Cuevas et al.,2002;Pe′rez et al., 2006;Sierra et al.,2007)and Portuguese(Esteves et al.,2002; Antunes et al.,2003;Palma et al.,2007)AIDS epidemics are characterized by high proportion of all non-B subtypes,CRFs and multiple recombinant forms between these variants.
The rapid evolution and redistribution of HIV pose a signi?cant challenge to the reliability of screening,diagnostic,and patient monitoring assays(Brennan et al.,2006;Buonaguro et al.,2007). The ability to anticipate and respond to this threat will be dictated to a signi?cant degree by our level of vigilance for newly emerging strains.The diversity of HIV-1genetic forms also challenges the prevention and treatment programs worldwide.The differences among HIV-1genetic forms may have a profound impact on clinical management and surveillance of drug resistance,particu-larly as treatment is expanded to non-subtype B viruses (Katzenstein,2006;Buonaguro et al.,2007).For instance, CRF02_AG may be more susceptible to nel?navir and ritonavir than other subtypes and this was associated with the70R polymorphism.Susceptibility to tipranavir may be lower among the subtype F and higher for subtype G(Abecasis et al.,2006).
Previous studies with a limited number of patients and restricted geographical and gene coverage indicated that most HIV-1subtypes are present in Angola(Abecasis et al.,2005;Ba′rtolo et al.,2005).The aim of this work was to perform a detailed follow up investigation of the genetic diversity and molecular epidemiol-ogy of HIV-1in Angola.
2.Materials and methods
2.1.Patients
Samples were collected from subjects with positive HIV serology in2001,except for seven samples that were collected in1993.Sequences were obtained from gag(p17),pol(PR and RT) and/or env(C2C3)genes of159HIV-1infected patients living in the
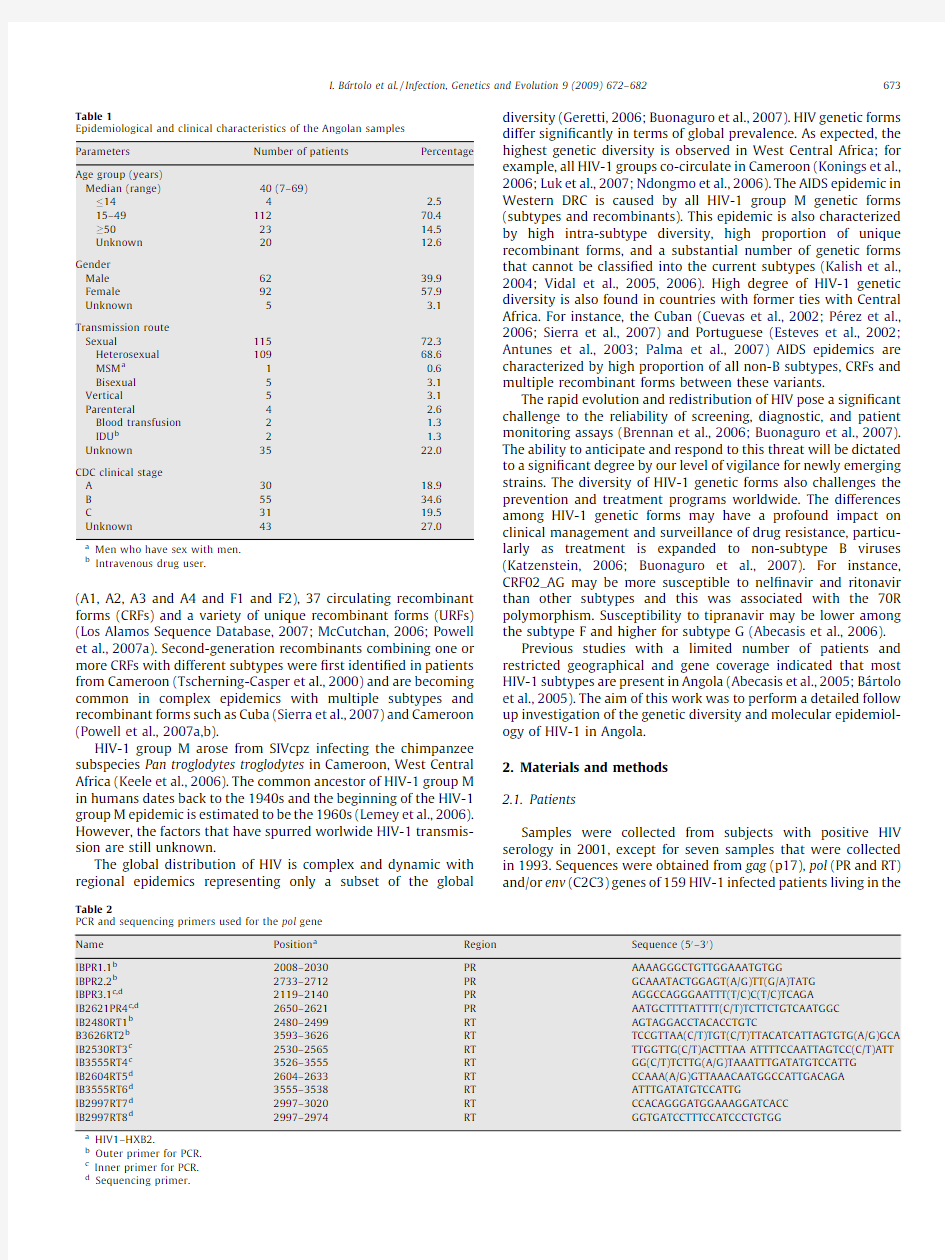
Table1
Epidemiological and clinical characteristics of the Angolan samples
Parameters Number of patients Percentage
Age group(years)
Median(range)40(7–69)
144 2.5
15–4911270.4
502314.5
Unknown2012.6
Gender
Male6239.9
Female9257.9
Unknown5 3.1
Transmission route
Sexual11572.3
Heterosexual10968.6
MSM a10.6
Bisexual5 3.1
Vertical5 3.1
Parenteral4 2.6
Blood transfusion2 1.3
IDU b2 1.3
Unknown3522.0
CDC clinical stage
A3018.9
B5534.6
C3119.5
Unknown4327.0
a Men who have sex with men.
b Intravenous drug user.
Table2
PCR and sequencing primers used for the pol gene
Name Position a Region Sequence(50–30)
IBPR1.1b2008–2030PR AAAAGGGCTGTTGGAAATGTGG
IBPR2.2b2733–2712PR GCAAATACTGGAGT(A/G)TT(G/A)TATG
IBPR3.1c,d2119–2140PR AGGCCAGGGAATTT(T/C)C(T/C)TCAGA
IB2621PR4c,d2650–2621PR AATGCTTTTATTTT(C/T)TCTTCTGTCAATGGC
IB2480RT1b2480–2499RT AGTAGGACCTACACCTGTC
B3626RT2b3593–3626RT TCCGTTAA(C/T)TGT(C/T)TTACATCATTAGTGTG(A/G)GCA IB2530RT3c2530–2565RT TTGGTTG(C/T)ACTTTAA ATTTTCCAATTAGTCC(C/T)ATT IB3555RT4c3526–3555RT GG(C/T)TCTTG(A/G)TAAATTTGATATGTCCATTG
IB2604RT5d2604–2633RT CCAAA(A/G)GTTAAACAATGGCCATTGACAGA
IB3555RT6d3555–3538RT ATTTGATATGTCCATTG
IB2997RT7d2997–3020RT CCACAGGGATGGAAAGGATCACC
IB2997RT8d2997–2974RT GGTGATCCTTTCCATCCCTGTGG
a HIV1–HXB2.
b Outer primer for PCR.
c Inner primer for PCR.
d Sequencing primer.
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682673
Fig.1.Genetic subtypes and evolutionary relationships of the viruses sequenced in this study based on maximum likelihood phylogenetic trees of partial gag (p17)(A),pol PR
(B),pol RT (C)and partial env sequences (C2C3)(D).The phylogenetic trees were constructed under a Kimura three-parameters with unequal base frequencies (K81uf +I +G)model of evolution for the env gene and under GTR +I +G for gag and pol genes.The phylogenetic trees were constructed with reference sequences from all HIV-1subtypes and sub-subtypes as well as with the Angolan sequences (shown in coloured symbols)and DRC sequences (indicated with asterisks).Putative new A5and A6sub-subtypes
I.Ba
′rtolo et al./Infection,Genetics and Evolution 9(2009)672–682674
Fig.1.(Continued ).
are indicated with interrogation marks.The bootstrap values supporting each of the internal branches de?ning a subtype or a sub-subtype are shown.The scale represents
number of base substitutions per site.
I.Ba ′rtolo et al./Infection,Genetics and Evolution 9(2009)672–682675
following provinces of Angola:Benguela(1patient,0.6%),Cabinda (22,13.8%),Cuanza Norte(1,0.6%),Luanda(126,79.3%),Lunda Norte(3,1.9%),Malange(2,1.3%),U?′ge(1,0.6%),and Zaire(3,1.9%). The serological diagnostic of the patients was done in Angola and the results were con?rmed in our lab with GENSCREEN1PLUS HIV Ag-Ab(Bio-Rad).The epidemiological characterization of the patients is described in Table1.According to the CDC Classi?cation System for HIV Infection category A consists in asymptomatic HIV infection or acute(primary)HIV infection;category B consists of symptomatic conditions that are not included among conditions listed in clinical category C and that meet at least one of the following criteria:the conditions are attributed to HIV infection or are indicative of a defect in cell-mediated immunity or the conditions are considered by physicians to have a clinical course or to require management that is complicated by HIV infection;and category C includes the clinical conditions listed in the AIDS surveillance case de?nition(CDC,1993).
2.2.Viral RNA extraction,PCR ampli?cation and sequencing
Sequences were obtained from gag(p17),pol(PR and RT)and/or env(C2C3)genes of159HIV-1infected patients.RNA was extracted from200m l of plasma using Nuclisens Isolation Kit (BioMerieux).RT-PCR was performed with Titan One Tube RT-PCR System(Roche).Nested PCR was done to obtain a409bp fragment from the C2C3env region using outer primers JA167and JA170and inner primers JA168and JA169;to obtain a582bp fragment from the p17gag region we used outer primers JA152and JA155and inner primers JA153and JA154.Thermal cycling conditions for ampli?cation of C2C3env region and p17gag region and primer numbers and positions have been described previously(Leitner et al.,1995).Nested PCR was done to obtain a532bp fragment from the PR region using outer primers IBPR1.1and IBPR2.2and inner primers IBPR3.1and IB2621PR4;to obtain a1026bp fragment from the RT region we used outer primers IB2480RT1 and IB3626RT2and inner primers IB2530RT3and IB3555RT4.PCR and primer numbers and positions are described in Table2.DNA sequences were obtained with Big Dye Terminator Cycle Sequen-cing Kit(Applied Biosystems)using the primers described in Table2.
2.3.Phylogenetic and recombination analysis
Sequences were aligned with reference strains(Los Alamos Sequence Database,2007)from each subtype using ClustalX1.8 (Thompson et al.,1997).All sequences from neighbouring countries available in the databases,especially those from DRC and Republic of Congo,were included in the alignment.The genetic distances between sequences were calculated using the Kimura two parameter substitution model with pairwise gap deletion(Kimura,1997)as implemented in the MEGA3.1program (Kumar et al.,2004).Maximum likelihood phylogenetic analyses (Felsenstein,1981)were performed using the best-?t model of molecular evolution estimated by Modeltest v3.7under the Akaike information criterion(Posada and Crandall,1998).The chosen models were K81uf+I+G for the env gene and GTR+I+G for gag and pol genes.Tree searches were conducted in PAUP v4.0b10using a nearest-neighbor interchange(NNI)heuristic search strategy(Swofford,2001),and bootstrap resampling (Felsenstein,1985).Bootstrap values 70%were considered de?nitive for signi?cant clustering(Hillis and Bull,1993).To con?rm recombination events and identify recombination break-points,bootscanning analysis was performed using Simplot3.5.1 (Lole et al.,1999).Brie?y,SimPlot calculates and plots the percent identity of the query sequence to a panel of reference sequences from group M viruses in a sliding window,which is moved across the alignment with optimal step size.The window and step sizes are adjustable(Salminen et al.,1995).The simplot software performed bootscanning on neighbor joining trees by usind SEQBOOT,DNADIST(with Kimura′s two-parameter method and F84maximum likelihood model,transition/transversion ratio=2),NEIGHBOR,and CONSENSE from the PHYLIP package for a200bp window moved along the aligment in increments of 20bp.
2.4.Statistical analysis
Statistical analysis was performed in GraphPad Prism version 4.0(GraphPad Prism,2003)with a level of signi?cance of5%.Inter and intra-subtype genetic distances were compared using the unpaired Student’s t-test.
2.5.GenBank accession numbers
Sequences have been assigned the following GenBank accession numbers AY456278–AY456330,AY676573–AY67594,EU031839–EU031891and EU068199–EU068462.
3.Results
The majority of the patients analysed in this study were from Luanda(126,79.3%),the Capital city,followed by Cabinda(22, 13.8%).A few patients were from seven other Provinces located mostly in the northern part of the country,Benguela(1,0.6%), Cuanza Norte(1,0.6%),Lunda Norte(3,1.9%),Malange(2,1.3%), U?′ge(1,0.6%),and Zaire(3,1.9%)(Fig.3).The median age of the patients was40years(7–69years)and57.9%were women (Table1).Heterosexual contact was the most common transmis-sion route(68.6%).According to the CDC Classi?cation System for HIV Infection(CDC,1993),only18.9%of the patients were in an asymptomatic condition,CDC clinical stage A,34.6%were in clinical stage B and19.5%were in clinical stage C(AIDS),at the time of sampling.These results are consistent with the fact that none of these patients were taking antiretroviral drugs.
A total of390sequences were produced from p17(30),PR(141), RT(123)and C2C3(96)and phylogenetic analysis was used to genotype the sequences(Fig.1).Table3summarizes the genetic forms found in each patient and each gene region.No group N or O viruses were found.Gene regions representing all HIV-1group M clades were found,as well as unclassi?able(7.5%)sequences.The following pure subtypes and sub-subtypes were identi?ed:A1 (8.8%),A2(4.4%),A3(0.6%),C(11.3%),D(5.0%),F1(8.2%),G(5.7%),H (5.7%)and J(3.1%).Two or more genomic regions were sequenced in122patients.Discordant phylogenies among the different genes indicating recombination were found in75(47.1%)patients (Table3).Fifty-eight different patterns of recombination were found.There were27(36.0%)second generation recombinant viruses,of which the most prevalent was A3/CRF02_AG/A1(PR/RT/ C2C3)(3,11.1%).A1,A2and A3sub-subtypes and CRF02_AG were involved in most of the recombinant events(53.3%).Bootscaning analysis of concatenated genes con?rmed the recombination events and enabled the identi?cation of some recombination breakpoints.Fig.2presents three examples of the results obtained with the bootscaning analysis.The isolate from patient 01AOSNS03is a recombinant between subtype C(in p17)and sub-subtype A2(in PR,RT and C2C3)(Fig.2A).In the isolates 01AOSNS09and01AOHDP29besides the recombination between genetic regions,we found evidence of recombination within regions.Thus,in the RT region01AOSNS09(Fig.2B)is a U/J/U recombinant and has recombination breakpoints in the1340and
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682 676
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682677
Table3
HIV-1genetic forms found in this study in Angolan patients
Isolate Genotype Isolate Genotype
p17PR RT C2C3p17PR RT C2C3
01AOSNS01U a G H H01AOSNS35–A1–A1
01AOSNS02–G––01AOSNS36–A2A A
01AOSNS03C A2A2A201AOSNS37–G G–
01AOSNS04–A2A1–01AOHSL38–A1A–
01AOHJM06A1A1H H01AOSNS39–A1A1A1
01AOSNS09C G U a C01AOSNS40A102AG02AG A1
01AOSNS10––05DF–01AOSNS41––F1–
01AOLFA11A1G02AG A101AOSNS47–G G G
01AOLFA12–––A101AOSNS48–F1F1F1
01AOLFA13–F1F1–01AOSNS49–A302AG A1
01AOLFA14A2A2A2A201AOSNS50–J J–
01AOLFA15C C C C01AOSNS51–H H H
01AOLFA16–C C C01AOSNS52–G G H
01AOLFA17A1A1A1A101AOSNS53–A1––
01AOLFA18–A2A2–01AOSNS54–G––
01AOLFA19A1A1A1A101AOSNS55C C C C
01AOHSL20–F1F1–01AOSNS56–H H H
01AOSNS21–C C C01AOSNS59C C C C
01AOSNS22A1U a H H01AOHJM60–C––
01AOSNS23A1G C H01AOHJM61–13cpx U a A2
01AOSNS24–A3A A01AOHJM62–09cpx09cpx11cpx 01AOSNS25–A1A1A101AOHJM63–G02AG H
01AOSNS27––02AG A101AOHJM64C C C C
01AOSNS28––D–01AOHDP65–02AG––
01AOHDP29–U a H H01AOHDP66–02AG02AG02AG 01AOHJM31–A2––01AOHDP67A102AG G A1
01AOSNS32–U a09cpx A401AOHDP68–C C A1
01AOSNS33––D–01AOHDP69–C––
01AOHDP70–C H H01AOHSN102––02AG–
01AOHDP71–C C C01AOSNS104–F1––
01AOHDP72–A1A1J01AOSNS106–A3A1A1
01AOHDP73–A1H02AG01AOSNS107–02AG U A1
01AOHDP74–A1––01AOSNS108––02AG–
01AOHDP75A102AG02AG A301AOSNS110–G–G
01AOHDP76–U a––01AOHDP111–––G
01AOHDP78–A1––01AOHDP112–A1A H
01AOHAB79–G H H01AOHJM113–D––
01AOHAB80–C H C01AOHJM114–D–J
01AOHAB81–A2–A101AOHJM115–C C C
01AOHAB82–02AG–A01AOCSE116–F1C F1
01AOHAB83–F1C C01AOCSE117–A1A1A1
01AOHAB84–––A01AOCSE118–A302AG A1
01AOHAB85–F1C F101AOCSE120–02AG U H
01AOHAB86–F1F1–01AOCSE121–D D D
01AOHAB87–A2––01AOCSE122–C C C
01AOHAB89G13cpx–B01AOCSE123–C C C
01AOHAB90–A302AG A101AOCSE124–A2A A
01AOHAB91G G G G01AOCSE125–02AG02AG A3
01AOHAB92G13cpx–J01AOCSE126–F1F1F1
01AOHAB93–A2––01AOCSE127–U a H H
01AOLFA94–A2A A01AOCSE128–F1––
01AOLFA95–U a02AG H01AOCSE129–C––
01AOLFA96–A1J A101AOCSE130–J––
01AOLFA97–02AG02AG A101AOCSE133––G–
01AOLFA98–A1–U a01AOCSE134–C G11cpx 01AOLFA99–U a––01AOCSE135––A1–
01AOHDP100–G G G01AOCSE136–A1A302AG 01AOHJM101–02AG–G01AOCSE140–––A1
01AOCSE141–––G01AOHDC229A1G H G
01AOML143––F1–01AOHDC230H H H H
01AOINSP145–––D01AOHDC231A1–––
01AOLFA146––F1–01AOHDC232G G G H
01AOHM176–D D–01AOHDC233–H H–
01AOHM180–C C–01AOHDC234H H––
01AOHM182–C C–01AOHDC235A1A102AG A1
01AOHM183–C C–01AOHDC236J J J J
01AOHM184–G H–01AOHDC237–H H H
01AOHM185–A1A1–01AOHDC238–D D–
01AOHM186–F1F1–01AOHDC239D05DF D D
01AOHM187–F1F1–01AOHDC240F1F1F1F1
01AOHM189–U a H–01AOHDC241–A1J J
01AOHM191–A2A2–01AOHDC242–G A02AG 01AOHM192–C C–93AOHDC247–J J J
1550bp positions;01AOHDP29(Fig.2C)is a recombinant A3/U in the PR region,with the recombination breakpoint in the position 200bp.The genetic classi?cation of each region was con?rmed by phylogenetic analysis performed with a sliding window around the recombination breakpoints (data not shown).
In the env and RT,two groups of sequences forming distinct sub-clusters within the subtype A radiation were found (Fig.1C and D).Genetic distances to sub-subtype A1,A2and A3varied from 19.3to 25.2%and 16.4to 22.7%for the two sub-clusters in the env gene and from 8.3to 10.6%for the sub-cluster in the RT region.The high genetic distances suggest that these sequences may de?ne new A5and A6sub-subtypes.4.Discussion
This is the ?rst work to document the genetic diversity of HIV-1in a large number of patients living in multiple Angolan Provinces.In a signi?cant amount of seropositive samples (52)we could not amplify viral DNA.This is not uncommon in this region of Africa and is probably related to the tremendous genetic variability of HIV-1(Kalish et al.,2004;McCutchan,2006;Brennan et al.,2006).A total of 159samples were directly sequenced in gag (p17),pol (PR and RT)and env (C2C3)genes.The phylogenetic analyses showed extremely high genetic diversity among Angolan HIV-1strains.In Angola all HIV-1group M subtypes and sub-subtypes co-circulate as well as the following CRFs:02_AG,05_DF,06_cpx,09_cpx,11_cpx and 13_cpx.Only 53%of viruses were pure subtypes,subtype A and its sub-subtypes predominating over the other subtypes (13.8%).If we consider that CRF02_AG is indeed an A sub-subtype and G is a recombinant between the A and J subtypes (Abecasis et al.,2007)then these ?gures will be even higher (19.5%adding subtype G and 22.0%adding CRF02_AG).This was not surprising because the countries in the Northern border of Angola have a predominance of the A subtype:46–48%in DRC (Kalish et al.,2004;Vidal et al.,2005)and 37–48%in Republic of Congo (Bikandou et al.,2004;Niama et al.,2006)(Fig.3).In Zambia,subtype C prevails over the other subtypes (98%)(Trask et al.,2002)so the signi?cant proportion of subtype C that was found in our patients (11.3%)was also expected.Finally,of note was the detection of the rare H (5.7%)and J (3.1%)subtypes and almost 8%of unclassi?able sequences.
In the env and pol (RT)genes,two groups of sequences forming distinct sub-clusters within the subtype A radiation were found (Fig.1).The values that we found for the genetic distances to sub-subtype A1,A2and A3sequences for the two sub-clusters in the env gene and for the sub-cluster in the RT region are similar to the ones observed within the other sub-subtypes for the same regions (Meloni et al.,2004).These sequences may,therefore,de?ne new A5and A6sub-subtypes.
Like in DRC,we found that a number of our sequences fall at basal positions on the phylogenetic trees (pre-subtype branches)(Archer and Robertson,2007;Rambaut et al.,2001;Kalish et al.,2004).In addition,some strains from Angola have little organized substructure and form weaker clusters within phylogenetic trees than the global reference sequences,not allowing a clear distinction between subtypes.As a consequence,the current global subtype classi?cation may not re?ect the extent of diversity in this region (Rambaut et al.,2004).Further analyses with genomic sequences will be needed to clarify whether these Angolan strains are ancestor viruses,pure subtypes or represent new genetic forms of HIV-1.Overall,these results indicate that Angola,like DRC,is one of the epicenters of the epidemic,with the global subtypes resulting from the export of some Angolan strains to other geographical regions.
Viral recombination takes place in geographic regions where several subtypes and CRFs circulate in the population.In these regions,8–24%of the infections may be due to inter-subtype recombinants (Meloni et al.,2004;Osmanov et al.,2002).In this study the percentage of recombinant strains was almost twice that amount (47.1%).Moreover,the Angolan recombinants are extre-mely complex since 58different patterns of recombination were identi?ed and 36.0%of these were second-generation recombi-nants.Second-generation recombinants were described for the ?rst time in patients from Cameroon (Tscherning-Casper et al.,2000).Recent studies performed in this country have led to the discovery of two new CRFs,CRF36_cpx and CRF37_cpx,which combine two CRFs,CRF01_AE and CRF02_AG (Powell et al.,2007a,b ).High number of recombinant strains imply high rate of co-infections and super-infections which is surprising given the current low prevalence of HIV-1in Angola.It may be that the current HIV/AIDS epidemic in Angola is mostly driven by a subpopulation of highly exposed individuals (such as sex workers)that are more prone to superinfection and give rise to higher incidences of recombination than could be expected from overall prevalence only.On the other hand,our results would be easy to explain if recombinant strains were the ancestors of the current subtypes as it has been recently demonstrated for CRF02_AG and subtype G (Abecasis et al.,2007).
There is a direct association between HIV-1genetic diversity,origin and infection time,so that older epidemics with multiple focus of infection,like HIV-1infection in Africa,are characterized by viruses with high genetic diversity (Kalish et al.,2004;Luk et al.,2007;Niama et al.,2006;Vidal et al.,2000,2005,2006),while recent infections originated by a single viral population are characterized by viruses with low among-host genetic diversity (Bobkov et al.,1997,2001;Roudinskii et al.,2004;Yu et al.,2001,2002).In this context,the high genetic diversity of HIV-1found in Angola suggests that,on one hand,HIV-1is circulating in Angola for a long time and,on the other hand,that there is intense population mobility between Angola,DRC and Republic of Congo (Santos-Ferreira et al.,1990).Two major events may have contributed signi?cantly to the pronounced genetic complexity of HIV-1in Angola:the colonial war with the Portuguese and the
Table 3(Continued )Isolate
Genotype Isolate
Genotype p17
PR RT C2C3p17PR RT C2C301AOHM193–A 2A 2–93AOHDC248–H H –01AOHM194–C C –93AOHDC249–A 3A –01AOHM195–02AG A 2–93AOHDC250–A 3––01AOHM198–H H –93AOHDC251–H H –01AOHM199–D D –93AOHDC252–A 3A –01AOHM200–F 1F 1–93AOHDC253
–
J
J
–
01AOHDC228F 1
F 1
F 1
B
(–)Unknown.a
Untypable.
I.Ba
′rtolo et al./Infection,Genetics and Evolution 9(2009)672–682678
civil war following Portuguese decolonisation.During the?rst years of the colonial war,starting in March1961and ending in April1974,thousands of people temporarily?ed from Angola to the neighbouring countries,especially to DRC and Republic of Congo.HIV-1group M has been circulating in DRC probably since the1940s(Zhu et al.,1998;Lemey et al.,2006).It is,therefore, likely that an important number of Angolan subjects become infected with HIV-1in1961in the South of DRC and Republic of Congo bringing back into Angola the different genetic forms of HIV-1present in those countries at the end of1961beginning of1962, when the population returned to Angola(Fig.3).This implies that the HIV-1epidemic in Angola is coincident with the beginning of the HIV-1/AIDS group M epidemic,which is estimated to be the 1960s(Lemey et al.,2006).Importantly,the independence war in Angola may have been the exact extrinsic factor that started the HIV-1/AIDS epidemic worldwide,much like the independence
war
Fig.2.Sliding window bootscanning analysis(window200bp;step20bp)of Angolan isolates01AOSNS03(A),01AOSNS09(B)and01AOHDP29(C).Bootscanning analysis was done as described in the text.The dashed line indicates the cut-off of70%.
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682679
in Guinea-Bissau (1963–1974)was the extrinsic factor that started
the HIV-2epidemic (Lemey et al.,2006).The epidemiologic data and the very high intra-subtype divergence of Angolan HIV-1isolates are consistent with a long-standing HIV-1epidemic in this country (Santos-Ferreira et al.,1990).On the other hand,the ?nding that the AIDS epidemic in Portugal is caused by a high proportion of highly divergent non-B subtypes and recombinant forms,strongly suggests that non-subtype B strains have been present in Portugal for a long time (Esteves et al.,2002;Antunes et al.,2003;Palma et al.,2007).The combined data,therefore,suggest that the intense people displacements during the colonial war with Angola may have had a decisive contribution to start the AIDS epidemic in Angola and Portugal,possibly in the mid-1960s.The civil war following Portuguese decolonisation,starting in April 1974and ending 2002,again prompted delocalization of large number of people within Angola and from Angola to the neighbouring countries specially DRC and Republic of Congo (Santos-Ferreira et al.,1990;Kapuscinski,2001).This may also have helped to spread HIV-1variants from DRC and Republic of Congo into Angola (Fig.3).As it has happened in Portugal during the independence war,the presence of Cuban soldiers in Angola in the civil war probably contributed signi?cantly to shape the current AIDS epidemic in Cuba,which is in part caused by highly divergent non-B HIV-1isolates and recombinant forms of African
origin (Cuevas et al.,2002;Kapuscinski,2001;Pe
′rez et al.,2006).In conclusion,the extraordinary degree of HIV-1genetic diversity in Angola is probably related to its close geographical proximity with several countries in Central Africa with old human HIV-1infections such as the DRC and Republic of Congo.The HIV/AIDS epidemic in Angola probably started in 1961,the major cause being the independence war,and subsequently spread to Portugal.
The fast rate of HIV-1group M genetic evolution detected in Angola may pose unprecedented challenges to diagnostic,treatment and prevention of HIV-1infection.Acknowledgments
This work was supported by grants from Fundac ?a
?o GlaxoS-mithKline das Cie ?ncias da Sau ′de and Fundac ?a
?o Calouste Gulben-kian,Portugal.Pedro Borrego is gratefully acknowledged for help in
some of the phylogenetic analysis presented in this paper.Ine
?s Ba ′rtolo is the recipient of a PhD scholarship from Fundac ?a
?o para a Cie
?ncia e Tecnologia (FCT),Portugal.Part of this work was presented in the 13th International Bioinformatics Workshop on Virus Evolution and Molecular Epidemiology,9–14September 2007,Lisbon,Portugal.References
Abecasis,A.,Paraskevis,D.,Epalanga,M.,Fonseca,M.,Burity,F.,Bartolomeu,J.,
Carvalho,A.P.,Gomes,P.,Vandamme,A.-M.,Camacho,R.,2005.HIV-1genetic variants circulation in the North of Angola.Infect.Genet.Evol.5(3),231–237.Abecasis,A.B.,Deforche,K.,Bacheler,L.T.,McKenna,P.,Carvalho,A.P.,Gomes,P.,
Vandamme,A.-M.,Camacho,R.,2006.Investigation of baseline susceptibility to protease inhibitors in HIV-1subtypes C,F,G and CRF02_AG.Antivir.Ther.11(5),581–589.
Abecasis,A.B.,Lemey,P.,Vidal,N.,de Oliveira,T.,Peeters,M.,Camacho,R.,Shapiro,
B.,Rambaut,A.,Vandamme,A.-M.,2007.Recombination confounds the early evolutionary history of human immunode?ciency virus type 1:subtype G is a circulating recombinant form.J.Virol.81(16),8543–8551.
Antunes,R.,Figueiredo,S.,Ba ′rtolo,I.,Pinheiro,M.,Rosado,L.,Soares,I.,Lourenc ?o,H.,
Taveira,N.,2003.Evaluation of the clinical sensitivities of three viral load assays with plasma samples from a pediatric population predominantly infected with human immunode?ciency virus type 1subtype G and BG recombinant forms.J.Clin.Microbiol.41(7),
3361–3367.
Fig.3.Possible origins of the Angolan HIV-1genetic forms and estimated dates of their dissemination to Portugal and Cuba.
I.Ba
′rtolo et al./Infection,Genetics and Evolution 9(2009)672–682680
Archer,J.,Robertson,D.L.,2007.Understanding the diversi?cation of HIV-1groups M and O.AIDS21(13),1693–1700.
Ba′rtolo,I.,Epalanga,M.,Bartolomeu,J.,Fonseca,M.,Mendes,A.,Gama,A.,Taveira, N.,2005.High genetic diversity of human immunode?ciency virus type1in Angola.AIDS Res.Hum.Retroviruses21(4),306–310.
Bikandou,B.,Ndoundou-Nkodia,M.Y.,Niama,F.R.,Ekwalanga,M.,Obengui,O., Taty-Taty,R.,Parra,H.J.,Saragosti,S.,2004.Genetic subtyping of gag and env regions of HIV type1isolates in Republic of Congo.AIDS Res.Hum.Retroviruses 20(9),1005–1009.
Bobkov,A.,Cheingsong-Popov,R.,Selimova,L.,Ladnaya,N.,Kazennova,E.,Krav-chenko,A.,Fedotov,E.,Saukhat,S.,Zverev,S.,Pokrovsky,V.,Weber,J.,1997.An HIV type1epidemic among injecting drug users in the former Soviet Union caused by a homogeneous subtype A strain.AIDS Res.Hum.Retroviruses13
(14),1195–1201.
Bobkov,A.F.,Samokhvalov,E.I.,Lvov,D.K.,Bobkova,M.R.,Povkrovsky,V.V.,Weber, J.N.,2001.Absence of viral transmission in injecting drug users in https://www.360docs.net/doc/e311903465.html,ncet 358(9286),1016–1017.
Brennan,C.A.,Bodelle,P.,Coffey,R.,Harris,B.,Holzmayer,V.,Luk,K.C.,Swanson,P., Yamaguchi,J.,Vallari,A.,Devare,S.G.,Schochetman,G.,Hackett Jr,J.,2006.HIV global surveillance:foundation for retroviral discovery and assay development.
J.Med.Virol.78(Suppl.1),S24–S29.
Buonaguro,L.,Tornesello,M.L.,Buonaguro,F.M.,2007.Human immunode?ciency virus type1subtype distribution in the worldwide epidemic:pathogenetic and therapeutic implications.J.Virol.81(19),10209–10219.
CDC,1993.Revised classi?cation system for HIV infection ad expanded surveillance case de?nition for AIDS among adolescents and adults.JAMA269,729–730. Cuevas,M.T.,Ruibal,I.,Villahermosa,M.L.,D?′az,H.,Delgado,E.,Parga,E.V.,Pe′rez-Alvarez,L.,de Armas,M.B.,Cuevas,L.,Medrano,L.,Noa,E.,Osmanov,S.,Na′jera, R.,Thomson,M.M.,2002.High HIV-1genetic diversity in Cuba.AIDS16(12), 1643–1653.
Esteves,A.,Parreira,R.,Venenno,T.,Franco,M.,Piedade,J.,Germano De Sousa,J., Canas-Ferreira,W.F.,2002.Molecular epidemiology of HIV type1infection in Portugal:high prevalence of non-B subtypes.AIDS Res.Hum.Retroviruses18
(5),313–325.
Felsenstein,J.,1981.Evolutionary trees from DNA sequences:a maximum like-lihood approach.J.Mol.Evol.17(6),368–376.
Felsenstein,J.,1985.Con?dence limits on phylogenies:an approach using the bootstrap.Evolution39(4),783–791.
Geretti,A.M.,2006.HIV-1subtypes:epidemiology and signi?cance for HIV manage-ment.Curr.Opin.Infect.Dis.19(1),1–7.
Graph Pad Software Inc.,2003.Prism4,version4.
Hillis,D.,Bull,J.,1993.An empirical test for bootscanning as a method for assessing viral sequence relatedness.Syst.Biol.42,182–192.
Kalish,M.,Robbins,K.,Pieniazek,D.,Schaefer,A.,Nzilambi,N.,Quinn,T.,Louis,M., Youngpairoj,A.,Phillips,J.,Jaffe,H.,Folks,T.,2004.Recombinant viruses and early global HIV-1epidemic.Emerg.Infect.Dis.10(7),1227–1234. Kapuscinski,R.,2001.Another Day of Life.Penguin Books.
Katzenstein,D.,2006.Diversity,drug resistance,and the epidemic of subtype C HIV-1in Africa.J.Infect.Dis.194(Suppl.1),S45–S50.
Keele,B.F.,Van Heuverswyn,F.,Li,Y.,Bailes,E.,Takehisa,J.,Santiago,M.L.,Bibollet-Ruche,F.,Chen,Y.,Wain,L.V.,Liegeois,F.,Loul,S.,Ngole,E.M.,Bienvenue,Y., Delaporte,E.,Brook?eld,J.F.,Sharp,P.M.,Shaw,G.M.,Peeters,M.,Hahn,B.H., 2006.Chimpanzee reservoirs of pandemic and nonpandemic HIV-1.Science313 (5786),523–526.
Kimura,M.,1997.A simple method for estimating evolutionary rate of base substitution through comparative studies of nucleotide sequences.J.Mol.Evol.
16,111–120.
Konings,F.A.,Haman,G.R.,Xue,Y.,Urbanski,M.M.,Hertzmark,K.,Nanfack,A., Achkar,J.M.,Burda,S.T.,Nyambi,P.N.,2006.Genetic analysis of HIV-1strains in rural eastern cameroon indicates the evolution of second-generation recombi-nants to circulating recombinant forms.J.Acquir.Immune De?c.Syndr.42(3), 331–341.
Kumar,S.,Tamura,K.,Nei,M.,2004.MEGA3:integrated software for molecular evolutionary genetics analysis and sequence alignment.Brief.Bioinform.5(2), 150–163.
Leitner,T.,Escanilla,D.,Marquina,S.,Wahlberg,J.,Brostrom,C.,Hansson,H.B., Uhlen,M.,Albert,J.,1995.Biological and molecular characterization of subtype D,G,and A/D recombinant HIV-1transmissions in Sweden.Virology209,136–146.
Lemey,P.,Rambaut,A.,Pybus,O.G.,2006.HIV evolutionary dynamics within and among hosts.AIDS Rev.8(3),125–140.
Lole,K.S.,Bollinger,R.C.,Paranjape,R.S.,Gadkari,D.,Kulkarni,S.S.,Novak,N.G., Ingersoll,R.,Sheppard,H.W.,Ray,S.C.,1999.Full-length human immuno-de?ciency virus type genomes from subtype C-infected seroconverters in India,with evidence of intersubtype recombination.J.Virol.73(1),152–160.
Los Alamos Sequence Database,2007.Los Alamos National Laboratory,Los Alamos, New Mexico.https://www.360docs.net/doc/e311903465.html,/.
Luk,K.C.,Holzmayer,V.,Yamaguchi,J.,Swanson,P.,Brennan,C.A.,Ngan-sop,C.,Mbanya,D.,Gayum,H.,Djuidje,M.N.,Ndembi,N.,Kamdem,D., Kaptue′,L.,Gu¨rtler,L.,Devare,S.G.,Hackett,J.,2007.Near full-length genome characterization of three additional HIV Type1CRF13_cpx strains from Cameroon.AIDS Res.Hum.Retroviruses23(2),297–392.
McCutchan,F.,2006.Global epidemiology of HIV.J.Med.Virol.78,S7–S12.Meloni,S.T.,Kim,B.,Sankale,J.L.,Hamel,D.J.,Tovanabutra,S.,Mboup,S.,McCutchan,
F.E.,Kanki,P.J.,2004.Distinct human immunode?ciency virus type1subtype A
virus circulating in West Africa:sub-subtype A3.J.Virol.78(22),12438–12445. Ndongmo,C.B.,Pieniazek,D.,Holberg-Petersen,M.,Holm-Hansen,C.,Zekeng,L., Jeansson,S.L.,Kaptue,L.,Kalish,M.L.,2006.HIV genetic diversity in Cameroon: possible public health importance.AIDS Res.Hum.Retroviruses22(8),812–816.
Niama, F.R.,Toure-Kane, C.,Vidal,N.,Obengui,P.,Bikandou, B.,Ndoundou Nkodia,M.Y.,Montavon, C.,Diop-Ndiaye,H.,Mombouli,J.V.,Mokondzi-mobe,E.,Diallo,A.G.,Delaporte,E.,Parra,H.J.,Peeters,M.,Mboup,S.,2006.
HIV-1subtypes and recombinants in the Republic of Congo.Infect.Genet.
Evol.6(5),337–343.
Osmanov,S.,Pattou,C.,Walker,N.,Schwardla¨nder,B.,Esparza,J.,2002.WHO-UNAIDS network for HIV isolation and characterization.Estimated global distribution and regional spread of HIV-1genetic subtypes in the year2000.
J.Acquir.Immune De?c.Syndr.29(2),184–190.
Palma, A.C.,Arau′jo, F.,Duque,V.,Borges, F.,Paixa?o,M.T.,Camacho,R.,2007.
Portuguese SPREAD Network.Molecular epidemiology and prevalence of drug resistance-associated mutations in newly diagnosed HIV-1patients in Portugal.
Infect.Genet.Evol.7(3),391–398.
Pe′rez,L.,Thomson,M.M.,Bleda,M.J.,Aragone′s,C.,Gonza′lez,Z.,Pe′rez,J.,Sierra,M., Casado,G.,Delgado,E.,Na′jera,R.,2006.HIV Type1molecular epidemiology in cuba:high genetic diversity,frequent mosaicism,and recent expansion of BG intersubtype recombinant forms.AIDS Res.Hum.Retroviruses22(8),724–733 (Erratum in:AIDS Res.Hum.Retroviruses22(11),1198).
Posada,D.,Crandall,K.A.,1998.MODELTEST:testing the model of DNA substitution.
Bioinformatics14,817–818.
Powell,R.L.,Zhao,J.,Konings,F.A.,Tang,S.,Ewane,L.,Burda,S.,Urbanski,M.M.,Saa,
D.R.,Hewlett,I.,Nyambi,P.N.,2007a.Circulating recombinant form(CRF)
37_cpx:an old strain in Cameroon composed of diverse,genetically distant lineages of subtypes A and G.AIDS Res.Hum.Retroviruses23(7),923–933. Powell,R.L.,Zhao,J.,Konings,F.A.,Tang,S.,Nanfack,A.,Burda,S.,Urbanski,M.M., Saa,D.R.,Hewlett,I.,Nyambi,P.N.,2007b.Identi?cation of a novel circulating recombinant form(CRF)36_cpx in Cameroon that combines two CRFs(01_AE and02_AG)with ancestral lineages of subtypes A and G.AIDS Res.Hum.
Retroviruses23(8),1008–1019.
Rambaut,A.,Robertson,D.L.,Pybus,O.G.,Peeters,M.,Holmes,E.C.,2001.Human immunode?ciency virus.Phylogeny and the origin of HIV-1.Nature410(6832), 1047–1048.
Rambaut,A.,Posada,D.,Crandall,K.A.,Holmes,E.C.,2004.The causes and con-sequences of HIV evolution.Nat.Rev.Genet.5(1),52–61.
Roudinskii,N.I.,Sukhanova, A.L.,Kazennova, E.V.,Weber,J.N.,Pokrovsky,V.V., Mikhailovich,V.M.,Bobkov,A.F.,2004.Diversity of human immunode?ciency virus type1subtype A and CRF03_AB protease in Eastern Europe:selection of the V77I variant and its rapid spread in injecting drug user populations.J.Virol.
78(20),11276–11287.
Salminen,M.O.,Carr,J.K.,Burke, D.S.,McCutchan, F.E.,1995.Identi?cation of breakpoints in intergenotypic recombinants of HIV type1by bootscanning.
AIDS Res.Hum.Retroviruses11(11),1423–1425.
Santos-Ferreira,M.O.,Cohen,T.,Lourenc?o,M.H.,Almeida,M.J.,Chamaret,S.,Mon-tagnier,L.,1990.A study of seroprevalence of HIV-1and HIV-2in six provinces of People’s Republic of Angola:clues to the spread of HIV infection.J.Acquir.
Immune.De?c.Syndr.3(8),780–786.
Sierra,M.,Thomson,M.M.,Posada,D.,Pe′rez,L.,Aragone′s,C.,Gonza′lez,Z.,Pe′rez,J., Casado,G.,Na′jera,R.,2007.Identi?cation of3phylogenetically related HIV-1 BG intersubtype circulating recombinant forms in Cuba.J.Acquir.Immune De?c.Syndr.45(2),151–160.
Swofford,D.L.,2001.PAUP*phylogenetic analysis using parsimony(*and other Methods).Version4.Sinauer-Associates,Sunderland,Massachusetts. Thompson,J.,Gibson,T.,Plewniak,F.,Jeanmougin,F.,Higgin,D.,1997.The CLUS-TALX windows interface:?exible strategies for multiple sequence alignment aided by quality analysis tools.Nucleic Acids Res.25,4876–4882.
Trask,S.A.,Derdeyn,C.A.,Fideli,U.,Chen,Y.,Meleth,S.,Kasolo,F.,Musonda,R., Hunter,E.,Gao,F.,Allen,S.,Hahn,B.H.,2002.Molecular epidemiology of human immunode?ciency virus type1transmission in a heterosexual cohort of dis-cordant couples in Zambia.J.Virol.76(1),397–405.
Tscherning-Casper, C.,Dolcini,G.,Mauclere,P.,Fenyo, E.M.,Barre-Sinoussi, F., Albert,J.,Menu, E.,2000.Evidence of the existence of a new circulating recombinant form of HIV type1subtype A/J in Cameroon.The European Network on the Study of In Utero Transmission of HIV-1.AIDS Res.Hum.
Retroviruses16(13),1313–1318.
UNAIDS,2006a.Epidemiological Fact Sheets on HIV/AIDS and Sexual Transmitted Infections.Angola,2006Update,December,Geneva.
UNAIDS,2006b.Epidemiological Fact Sheets on HIV/AIDS and Sexual Transmitted Infections.Republic of South Africa,2006Update,December,Geneva. UNAIDS,2006c.Epidemiological Fact Sheets on HIV/AIDS and Sexual Transmitted Infections.Democratic Republic of Congo,2006Update.December,Geneva. UNAIDS,2007.Global summary of the AIDS epidemic.December,Geneva. Vidal,N.,Peeters,M.,Mulanga-Kabeya,C.,Nzilambi,N.,Robertson,D.,Ilunga,W., Sema,H.,Tshimanga,K.,Bongo,B.,Delaporte,E.,2000.Unprecedented degree of human immunode?ciency virus type1(HIV-1)group M genetic diversity in the Democratic Republic of Congo suggests that the HIV-1pandemic originated in Central Africa.J.Virol.74(22),10498–10507.
Vidal,N.,Mulanga,C.,Bazepeo,S.E.,Mwamba,J.K.,Tshimpaka,J.W.,Kashi,M., Mama,N.,Laurent,C.,Lepira,F.,Delaporte,E.,Peeters,M.,2005.Distribution of
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682681
HIV-1variants in the Democratic Republic of Congo suggests increase of subtype C in Kinshasa Between1997and2002.J.Acquir.Immune De?c.Syndr.
40(4),456–462.
Vidal,N.,Mulanga,C.,Bazepeo,S.,Mwamba,J.K.,Tshimpaka,J.W.,Kashi,M.,Mama, N.,Laurent,C.,Lepira,F.,Delaporte,E.,Peeters,M.,2006.Identi?cation and molecular characterization of subsubtype A4in Central Africa.AIDS Res.Hum.
Retroviruses22(2),182–187.
Yu,X.F.,Liu,W.,Chen,J.,Kong,W.,Liu,B.,Yang,J.,Liang,F.,McCutchan,F., Piyasirisilp,S.,Lai,S.,2001.Rapid dissemination of a novel B/C recombi-
nant HIV-1among injection drug users in southern China.AIDS15(4), 523–525.
Yu,X.F.,Liu,W.,Chen,J.,Kong,W.,Liu, B.,Zhu,Q.,Liang, F.,McCutchan, F., Piyasirisilp,S.,Lai,S.,2002.Maintaining low HIV type1env genetic diversity among injection drug users infected with a B/C recombinant and CRF01_AE HIV type1in southern China.AIDS Res.Hum.Retroviruses18(2),167–170. Zhu,T.,Korber,B.T.,Nahmias,A.J.,Hooper,E.,Sharp,P.M.,Ho,D.D.,1998.An African HIV-1sequence from1959and implications for the origin of the epidemic.
Nature391,594–597.
I.Ba′rtolo et al./Infection,Genetics and Evolution9(2009)672–682 682
第三章艾滋病
第三章病毒感染性疾病 第十五节艾滋病 一、学习要点 ㈠掌握艾滋病的流行病学特点 艾滋病(AIDS)的传染源是艾滋病人和无症状病毒携带者;通过性接触、注射途径、母婴及器官移植等医疗行为进行传播;男同性恋者性乱交者、静脉药瘾者、血友病和多次输血者为高发人群。 ㈡掌握艾滋病的临床特征 艾滋病毒(HIV)感染人体后经2~10年潜伏期发展为艾滋病,在临床上分为四期:急性感染期、无症状感染期、持续性全身淋巴结肿大期、艾滋病期。在艾滋病期临床谱十分广泛,主要表现有①体质性疾病;②神经系统表现;③机会性感染;④继发肿瘤;⑤免疫缺陷并发的其它疾病,如慢性淋巴性间质性肺炎。 ㈢掌握HIV感染的实验室诊断 主要依靠检查抗-HIV来建立实验室诊断,常用酶联免疫(ELISA)方法做初筛试验,而以免疫印迹法(Western blot)做确诊试验。在某些情况下可用检测P 24抗原、用Northern blot 或RT-PCR法检测HIVRNA来明确HIV感染。 ㈣熟悉艾滋病的发病机制 艾滋病的发病机制主要是CD4+T细胞在HIV直接和间接作用下,细胞功能受损和大量破坏,导致细胞免疫缺陷,由于其他免疫细胞均不同程度受损,因而促使并发各种严重的机会性感染和肿瘤发生。 二、复习题及答案 (一)名词解释 1.母婴传播 2.肺孢子虫肺炎 3.卡波氏肉瘤 名词解释答案: 1.母婴传播:已感染HIV的孕妇可通过胎盘、产程中及产后血性分泌物或喂奶等将HIV传播给婴儿,此称之为母婴传播。 2.肺孢子虫肺炎(PCP):由肺孢子虫引起的肺炎,主要表现为慢性咳嗽及短期发热,呼吸急促和紫绀,动脉血氧分压降低,肺部少有罗音,X线胸片表现为间质性肺炎,痰或支气管灌洗液等检出肺孢子虫可作出诊断。 3.卡波氏肉瘤(Kaposi’s sarcoma)是HIV与人庖疹病毒8型共同感染所导致的恶性肿瘤,常侵犯皮肤或黏膜。 (二)填空题 1. HIV感染后使人体CD4+T细胞的受损的方式及表现有①-------------------------②----------------------------------③-------------------------------------④------------------------------- 2. 艾滋病患者常见临床表现的受累系统和器官通常是①----------------②---------------- ③-------------------④------------------⑤------------------ 3. 目前抗HIV的药物可分为三大类①-----------------②-------------------③----------------- 填空题答案: 1.HIV感染后使人体CD4+T细胞的受损的方式及表现有①病毒直接损伤②非感染的CD4+细胞受累③HIV感染干细胞④免疫损伤。
2020年世界艾滋病日是哪一天
2020年世界艾滋病日是哪一天 篇一:世界艾滋病日活动策划书2020 世界艾滋病日活动策划书2020 世界艾滋病日活动策划书2020 一、活动主题:平等倾听关爱艾滋孤儿二、活动目的: 1.通过一系列的和主题相关的活动让学生关注河南艾滋病问题及艾滋病孤儿生活及教育的现状。 2.通过募捐等形式为孩子们提供物质上的帮助。 3.使黑大成为在全国高校推广1+1救助模式的试点。三、活动时间:11月27日——12月1日四、活动方式:通过征集签名、与艾滋病相关图片展览、何建章在东珍作为志愿者的经历报告会、与艾滋病主题相关的电影《费城故事》放映等活动让同学了解艾滋病的危害以及在中国的现状,关注艾滋孤儿,达到此次活动的目的五、活动内容:第一阶段:活动前期宣传时间:11月27日-11月30日地点:a区、b区、c区食堂方式:以海报的形式,告知同学活动主题和日程安排。宣传:用主题海报和传单的形式、校广播在中午、下午时段播报的形式让同学了解活动安排。第二阶段:电影的放映,使同学初步对艾滋病有所认识。时间:11月30日18:00 地点:多媒体教室(待定)方式:放映《费城故事》,宣传:于11月30号早(2020网络文化节活动策划书)上在a区、b区、c区食堂张贴关于电影内容的海报
第三阶段:签名活动、图片展、报告会,此活动为重点,分为两部分进行: 时间:12月1日9:00----17:00 地点:3、4号楼大厅或图书馆方式:展版活动内容一:通过11月30号晚上的电影让同学融入到我们的活动当中,举办“平等倾听关爱”为主题,长12.1米的横幅签名活动,活动内容二:艾滋病相关图片展,展板内容暂定为六部分 1. 活动主题海报主题:平等倾听关爱艾滋孤儿 2. 活动序言主题:无 3. 艾滋病的影响和危害;艾滋病村现状—卢广的照片主题:绝望气息的弥漫 4.中国艾滋孤儿的生活及学习现状—孩子的照片主题:他们渴望阳光 5.目前艾滋孤儿的救助形式—东珍学校、阳光家园、1+1 主题:让我们给他们一双翅膀 6.受到救助孩子的生活—10.1的照片附:1+1救助宣传主题:沐浴晨光的天使活动内容三:在图片展边设立募捐箱,所筹集的款项均用在孩子的学习和生活上。可由活动工作人员配合展版进行讲解。世界艾滋病日活动策划书2020世界艾滋病日活动策划书2020。活动内容四:对到场的同学发放红丝带及东珍宣传明信片宣传:第一阶段的主题海报不撤消,造成规模效应,邀请哈尔滨当地的媒体进行报道、校广播站进行宣传、活动工作人员对现场活动采用录像、摄影等形式跟踪报道,在校园网、sohu网、、东珍网站等进行宣传。活动内容五:时间:12月1日19:30—21:00 地点:多媒体教
艾滋病的起源
艾滋病的起源 艾滋病病毒(HIV)来自何方,是通过什么渠道到达人体并感染人类的等等,一直让入迷惑不解。研究人员通过调查、研究和分析推理,终于对其中的一种假说给予了更多的肯定,而且艾滋病的发展也出现了种种新的迹象。 起源与假说 1981年6月5日,美国疾病控制和预防中心(CDC)报道,洛杉矶地区5名健康的男同性恋者患了卡氏肺囊虫肺炎(PCP)。后来美国其他地区也相继发现了相似的病人,CDC重新谨慎地评估这种疾病后,认为这是一种新的疾病在流行。到1982底,仅美国就有30多个州报道了800多名类似的病例,相关的症状还包括卡波济肉瘤(KS)、黏膜白色念珠菌病和播散性巨细胞病毒感染等。此后这种新疾病在全球蔓延,病人有一个共同的特征,免疫系统尤其是胸腺T淋巴细胞受到严重破坏。直到1982年,专业人员才把这种主要损害人体免疫系统的疾病命名为获得性免疫缺陷综合征(Acquired Immune DeficiencySyndrome,AIDS),因HIV破坏人体免疫力造成各种临床症状。 HIV起源何方?主要有三种假说,即自然说、医源说和人为说。自然说认为,HIV是自然演变而产生的,在偶然的机会感染了人类。比较流行的观点是HIV 来源于非洲的黑猩猩或绿猴等,医源说认为,人类在生产小儿麻痹症疫苗时使用了被污染的黑猩猩器官组织,在疫苗接种时被感染。人为说又有几种观点,一是认为HIV是美国中央情报局制造的生物武器,二是认为它是基因工程带来的灾难,三是认为HIV是纳粹的残渣余孽或者某个疯狂的科学家企图进行种族灭绝、建立世界新秩序的产物。 但是,随着研究和调查的深入,专业人员否认了后两种说法,而肯定前一种说法。在HIV是自然演化的假说中,研究人员又认为HIV—1来自于非洲黑猩猩,而HIV-2来自于非洲黑白眉猴。 起源时间与HIV-2 被HIV感染的人类早期标本一共有三个。它们是1959年收集的一位生活在刚果民主共和国的成年男性的血浆,1969年收集的在美国圣·路易斯死亡的一位非洲后裔的人体组织标本,还有一位是1976年死亡的挪威海员的人体组织标本。 1998年美国著名华裔科学家何大一领导的阿伦·戴蒙艾滋病研究中心对1959年采集的血浆标本进行了研究分析。他们认为,在这位生活在非洲班图部落的男性体内所发现的HIV是目前在全世界传播的HIV亚型的祖先。从它的进
世界艾滋病日宣传主题
世界艾滋病日宣传主题 引导语:世界艾滋病日的目的是号召世界各国和国际组织在这一天举办相关活动,宣传和普及预防艾滋病的知识。下面是历届世界艾滋病日的主题,一起来看一下吧! xx年:“行动起来,向‘零’艾滋迈进”(英文主题为Getting to Zero),副标题为“凝聚力量,攻坚克难,控制艾滋”。意在说明我国艾滋病防治工作到了关键时期,面临很多困难和挑战,需要动员各级政府、部门、社会组织和志愿者,集中各方面力量,解放思想、开拓创新、破解防治工作难题,控制艾滋病流行。 xx年:活动主题仍为“行动起来,向‘零’艾滋迈进”(英文主题Getting to Zero),副标题是“共抗艾滋,共担责任,共享未来”。 xx年:与xx年相同,副标题是“共抗艾滋,共担责任,共享未来”。旨在号召全社会积极投身于艾滋病防治工作,共同承担防治责任和义务,群策群力,各展所长,遏制艾滋病的流行。 xx年:与xx年相同,仍为“行动起来,向‘零’艾滋迈进”(英文主题Getting to Zero),副标题是“全民参与,全力投入,全面预防”。中国确定的副题是:全民参与,全力投入,全面预防。 xx年:行动起来,向“零”艾滋迈进(Getting to Zero)。 xx年世界艾滋病日主题:正视艾滋,重视权益,点亮反歧视之光(Keep the lighton HIV and human rights)我国主标题为“遏制艾滋,履行承诺”副标题为“权益,责任,落实”。
xx年:主题为“普遍可及和人权” (Universal Aess and Human Rights)。艾滋病防控在撒哈拉以南非洲地区仍任重道远。 xx年:主题是“领导”,宣传口号为“遏制艾滋、履行承诺”(stop AIDS,keep the promise)。 xx年:主题是“领导”,宣传口号为“遏制艾滋、履行承诺”(stop AIDS,keep the promise),意在突出领导者在艾滋病防治中的作用。 xx年:遏制艾滋,履行承诺(stop AIDS,keep the promise)。 xx年:遏制艾滋,履行承诺(stop AIDS,keep the promise)。 xx年:关注妇女,抗击艾滋(Women,Girls,HIV and AIDS)。 xx年:沿用去年“相互关爱,共享生命” (Live,let Live)的宣传主题,强调以消除歧视、倡导关爱的精神来鼓励全社会积极行动,采取更为有效的措施,为艾滋病病毒感染者和病人创造更为宽松和谐的生活环境。 xx年:相互关爱,共享生命(Live,let Live)。 xx年:预防艾滋病,你我同参与(I care,and You?)。 2000年:预防艾滋病,男士责无旁贷(Men Make a Difference)。 1999年:关注青少年,预防艾滋病——倾听、学习、尊重(Listen,Learn,Live!)。 1998年:青少年:迎战艾滋病的生力军(Force for Change:World AIDS Campaign with Young People)。
世界艾滋病日的由来
世界艾滋病日的由来 1981年6月,美国洛杉矶发现5名年轻男性,因患少见的肺囊肺炎而死亡;几乎同时,纽约也发现20名因少见的卡波西式肉瘤去逝的年轻男性。后来经美国国立疾病管制局(CDC)研究并证实:他们均死于一种免疫系统机能丧失的同一类症候群,并于1982年将 这种疾病正式命名为A(Acquired后天)I(Immune免疫)D(Deficiency缺乏)S (Syndrome症候群),简称为AIDS。 会因为爱滋病死亡,主要是感染了一种造成身体免疫功能丧失的病毒─H(Human人类)I(Immunodeficiency免疫)V(Virus病毒),HIV即是人类免疫缺乏病毒,俗称爱滋病毒;这些病毒会攻击身体的免疫系统,后天免疫缺乏症候群(爱滋病)则是感染人类免疫 缺乏病毒的末期表现。 为了保障日益增多的爱滋感染者的人权,联合国世界卫生组织于1988年元月全球高 峰会议中提出了「爱滋病防治方案」,并且明订每年的12月1日为「世界爱滋病日」, 协助世界各国发展爱滋疫情防治策略,同时每年订定一个宣导主题,提出对爱滋人权的呼吁。 根据世界卫生组织的统计,超过70%的爱滋感染者是经由异性间的性行为传染所致,另外10%则是由男性传染给男性,而男性比女性较少主动寻求健康咨询,也比较喜欢尝试些危险行为,其中尤以酗酒、药物滥用及嫖妓等,都是导致本身或是他们的性伴侣成为爱 滋病毒高危险群的主要原因;所以,今年世界卫生组织将爱滋病日宣导主题定为「Menmakeadifference」,期望男性应主动避免各项高危险性行为并采取适当的防护措施 以降低爱滋病对全人类的威胁。 感谢您的阅读。 祝语:流泻的月光,笼罩着浓浓的思念,倾泻了一地的氤氲,洁白的光辉,是我真切的祝福,轻轻洒落在你的四周,愿平安,好运包围着你,愿快乐,幸福伴随着你。
2016年艾滋病全球与全国流行情况梳理汇总贴(by-BD最新)
2016年艾滋病全国流行状况 据联合国驻华机构公布的数据,目前中国艾滋病病毒感染者约84万人,加上已经染病死亡的24万人,总数应该在100万人左右。根据世界卫生组织统计,目前中国艾滋病病毒感染者占总人口的比例虽然很低,但感染人数在亚洲位居第2位,在全球居第14位。(此为06年的数据,而且应该为估计的,仅仅作为参考不可当真) 《2013年中国艾滋病疫情估计工作报告》报道,截止2013年底,中国存活艾滋病病毒感染者和艾滋病病人有436 817例,死亡136 274例,现存活的艾滋病病人173 825例,艾滋病感染者262 992例。 截止2014年12月,全国报告现存活HIV/AIDS病例500679例,死亡15873例。2014年新发现HIV/AIDS病例103501例。 截至2015年底,我国报告存活艾滋病感染者和病人57.7万;估计我国存活艾滋病感染者和病人85万(72万-102万)。2016年6月,国家卫计委出台新政,艾滋病毒感染者抗病毒治疗标准修订为:"对所有HIV感染者提供治疗",为实现为90%HIV感染者提供抗病毒治疗的目标提供了政策保证。 截至2016年8月31日,全国报告现存活艾滋病病毒(HIV)感染者/AIDS病人645541例,报告死亡198523例。现存活HIV感染者379543例,AIDS病人265998例。2016年8月,新发现HIV感染者/AIDS病人12130例,既往HIV感染者本月转化为AIDS病人2587例。本月报告死亡2206例中,本月死亡952例,既往死亡1254例。本月新发现的HIV感染者/AIDS病人中,HIV感染者男女之比为 3.6∶1,AIDS病人男女之比为3.6∶1;15岁以下HIV感染者90例,AIDS病人11例。 2016年8月,新发现的HIV感染者/AIDS病人中, 异性性传播7963例(65.6%); 同性性传播3093例(25.5%); 注射毒品传播577例(4.8%); 母婴传播79例(0.7%); 性接触加注射毒品传播43例(0.4%); 输血及使用血制品传播9例(0.1%);
艾滋病流行病学特征
艾滋病流行病学特征 了解南充市高坪区艾滋病流行病学特征,为制定控制策略提供依据。方法对南充市高坪区1999—2010年HIV/AIDS疫情报告、综合监测、自愿咨询、流行病学调查资料收集统计,采用描述性流行病学方法进行分析研究。结果1999—2010年高坪区共报告HIV/AIDS 74例,感染率为12.76/10万。男女之比为2.21∶1;传播途径以性接触传播为主,占总例数的58.11%;年龄分布以20~39岁最高,占总例数的71.62%;职业分布以无业人员居多,占40.54%;发现途径以咨询检测为主,占总数的29.73%,其次为专题调查检测,占20.27%。2005-2010年共报70例,占总数的94.59%,年均感染率为1.10/10万,呈快速增长高峰。结论南充市高坪区艾滋病感染者2005-2010年为快速增长期,以性接触传播为主要方式,应针对高危人群和高危行为,采取综合监测干预措施,控制艾滋病的流行。 随着艾滋病在全球迅速蔓延,其流行所造成的危害已成为严重的公共卫生问题,严重影响各国的经济和社会进步[1]。南充市高坪区自1999年发现首例艾滋病感染者以来,截至2010-12-31,全区累计报告HIV感染者74例,其中,艾滋病患者18例,死亡13例。为了有效地控制艾滋病流行,现将1999—2010年南充市高坪区HIV/ADIS流行病学特征与控制对策分析报告如下。 1. 资料与方法 1.1 资料来源南充市高坪区1999—2010年HIV/AIDS疫情报告、综合监测、咨询检测、专题调查检测资料。 1.2 方法以HIV确认检测报告为依据,收集整理资料,并将数据录入Epi-data 2.1数据库统计,然后采用描述性流行病学方法分析研究。 2. 结果 2.1 HIV/AIDS流行强度1999—2010年南充市高坪区共报告HIV感染者74例,感染率为12.82/10万,其中AIDS患者18例,死亡13例,病死率为72.22%。其间2005年感染者最多,占历年总数的24.32%(18/74)(表1)。 2.5 传播途径HIV感染者以性接触传播为主,占总数的58.11%(43/74),其中,夫妻婚内传播的14例,占性传播总数的32.56%,男性同性传播5例,占性传播的11.63%;其次为注射吸毒传播,占感染者总数(27/74)的36.49%,输血传播最低,占总数的1.35%(表5)。 2.6 发现途径HIV感染者发现途径以咨询检测为主,占感染者总数(22/74)的29.73%,其次为专题调查,占20.27%,专科性病门诊最低,占1.35%(表6)。 3. 讨论 南充市高坪区自1999年发现首例HIV感染者以来,截至2010-12-31,共报告HVV/AIDS 74例,年均感染率为12.76%,2005年以来,疫情呈快速增长高峰,6年间,共报告HIV/AIDS 70例,占总数的94.59%,且以性传播为主,占历年总数的58.11%,其中,婚内夫妻传播占性传播总数的32.56%,男性同性传播占11.63%,表明高坪区近年来HIV/AIDS进入快速增长期,性传播成为主要传播途径[2],存在家庭内配偶之间相互传染[3],通过性途径从高危人群向一般人群扩散,配偶间的性传播起着不可忽视的作用[4]。年龄分布以20~39岁青壮年为主,占总数的71.92%,男女之比为2.2:1,与王永梅等[5]报道相符。 同艾滋病作斗争的最大希望就是通过健康教育等干预形式,帮助人们了解预防艾滋病知识,选择比较安全的行为,从而阻断艾滋病的传播[6],健康教育是行为干预的重要理论基础[7]。高坪区自2008年以来,在中国-默沙东艾滋病防治合作项目的支持下,探索适合高危人群监测干预和大众人群健康教育模式,深入开展艾滋病综合防治工作:一是进村入户宣传、巡回放映电影,使农村群众和城镇居民喜闻乐见、直观体验并感觉到艾滋病就在身边,但这
历年世界艾滋病日的主题
历年世界艾滋病日的主题 世界艾滋病日自设立以来,每年都有一个明确的宣传主题。围绕主题,联合国艾滋病规划署、世界卫生组织及其成员国都要开展各种形式的宣传教育活动。 【1988年】全球共讨,征服有期(Join the Worldwide Effort) 【1989年】我们的生活,我们的世界——让我们相互关照 Our Lives,Our World----Let's Take Care of Each Other 【1990年】妇女和艾滋病"(Women and AIDS) 【1991年】共同迎接艾滋病的挑战(Sharing the Challenge) 【1992年】预防艾滋病,全社会的责任(A Community Commitment) 【1993年】时不我待,行动起来(Time to Act) 【1994年】家庭与艾滋病(AIDS and the Family) 【1995年】共享权益,同担责任(Shared Right, Shared Responsibilites)【1996年】一个世界,一个希望(One World, One Hope) 【1997年】艾滋病与儿童(Children Living in a World with AIDS)【1998年】青少年--迎战艾滋病的生力军 Force for Change: World AIDS Campaign with Young People 【1999年】倾听、学习、尊重(Listen, Learn, Live!) 【2000年】男士责无旁贷(Men Make a Difference) 【2001年】你我同参与(I care, and You?) 【2002年】相互关爱,共享生命(Live, let Live) 【2003年】主题仍为相互关爱,共享生命(Live, let Live) 【2004年】关注妇女,抗击艾滋(Women, Girls, HIV and AIDS) 【2005年】遏制艾滋履行承诺(stop AIDS,keep the promise ) 【2006年】仍然是“遏制艾滋,履行承诺”。 【2007年】宣传主题仍然是遏制艾滋,履行承诺。 【2008年】主题仍为“遏制艾滋,履行承诺”。 【2009年】普遍可及和人权(Universal Access and Human Rights) 【2010年】正视艾滋,重视权益,点亮反歧视之光
艾滋病的来源和起因
有人说是德国在二次世界大战时,人工研究出来的一种病毒;也有人说是日本人研究出来的;还有人说是上帝为了惩罚人类的性乱而使之降临的人类的。等等诸如此类的说法,大部分是没有实质根据的。了解人类对于艾滋病发展的历史,其实是非常必要的一件事情,有助于人类预防并攻克爱滋病。最近,由美国、欧洲和喀麦隆科学家组成的一个国际研究小组说,他们通过野外调查和基因分析证实,人类艾滋病病毒HIV-1起源于野生黑猩猩,病毒很可能是从猿类免疫缺陷病毒SIV进化而来。其实,艾滋病的起源应该是在非洲。1959年的刚果,还是法属殖民地。一个自森林中走出的土人,被邀请参与一项和血液传染病有关的研究。他的血液样本经化验后,便被予以冷藏,就此尘封数十年。万没想到的是,数十年后,这血液样本竟然成为解开艾滋病来源的重要线索。 艾滋病起源于非洲,后由移民带入美国。1981年6月5日,美国亚特兰大疾病控制中心在《发病率与死亡率周刊》上简要介绍了5例艾滋病病人的病史,这是世界上第一次有关艾滋病的正式记载。1982年,这种疾病被命名为"艾滋病"。不久以后,艾滋病迅速蔓延到各大洲。1985年,一位到中国旅游的外籍青年患病入住北京协和医院后很快死亡,后被证实死于艾滋病。这是我国第一次发现艾滋病(见曾毅:爱滋病的流行趋势、研究进展及遏制策略)。 艾滋病严重地威胁着人类的生存,已引起世界卫生组织及各国政府的高度重视。艾滋病在世界范围内的传播越来越迅猛,严重威胁着人类的健康和社会的发展,已成为威胁人们健康的第四大杀手。联合国艾滋病规划署2006年5月30日宣布自1981年6月首次确认艾滋病以来,25年间全球累计有6500万人感染艾滋病毒,其中250万人死亡。到2005年底,全球共有3860万名艾滋病病毒感染者,当年新增艾滋病病毒感染者410万人,另有280万人死于艾滋病。2006年11月联合国艾滋病规划署和世界卫生组织(WHO)在日内瓦共同发布2006年艾滋病全球流行的最新情况。该报告显示,全球艾滋病流行仍呈增长态势:目前共有3950万人感染了艾滋病病毒,比2004年增加了260万人,其中15岁以下儿童感染人数达到230万。2006年全球共有290万人死于艾滋病,其中15岁以下儿童死亡数为38万;同年还新增了430万感染者,其中65%(约280万人)出现在南撒哈拉非洲。呼吁各国政府对防止艾滋病蔓延予以充分重视,以防止这一状况进一步恶化。据专家介绍,艾滋病病毒感染者从感染初期算起,要经过数年、甚至长达10年或更长的潜伏期后才会发展成艾滋病病人。艾滋病病人因抵抗能力极度下降会出现多种感染,如带状疱疹、口腔霉菌感染、肺结核,特殊病原微生物引起的肠炎、肺炎、脑炎等,后期常常发生恶性肿瘤,直至因长期消耗,全身衰竭而死亡。 虽然全世界众多医学研究人员付出了巨大的努力,但至今尚未研制出根治艾滋病的特效药物,也没有可用于预防的有效疫苗。目前,这种病死率几乎高达100%的"超级癌症"已被我国列入乙类法定传染病,并被列为国境卫生监测传染病之一。故此我们把其称为"超级绝症"。
我国艾滋病的流行现状(一)
我国艾滋病的流行现状(一) 【关键词】艾滋病 艾滋病是一种严重危害人类健康的传染病,在近27年的时间里,艾滋病已经波及到全球200多个国家和地区,感染者总数已超过6000万,2000万人死于艾滋病。目前,它已经不再仅仅是众多公共卫生问题中的一个,而成为了与气候改变和极度贫困等同的非传统威胁。由于该病潜伏期长、隐蔽性强、传播途径多样化、病死率高,目前即无能治愈的药物也无有效的疫苗预防,给防治工作带来了严重困难。 1艾滋病的病原学特点 艾滋病即获得性免疫缺陷综合征(acquiredimmunodeficiencysyndrome,AIDS)。这是一种慢性致死性传染病,由人类免疫缺陷病毒(humanimmunodeficiencyvirus,HIV)引起。HIV感染后导致人体免疫机能缺陷,从而发生机会性感染和肿瘤等一系列临床综合征,病死率几乎达100%。 2我国艾滋病的流行情况 我国于1985年发现首例艾滋病感染病例。截至2008年底,累计报告艾滋病感染者/艾滋病病人276335人,其中艾滋病病人82322例,死亡38150例;2008年报告HIV45572例,AIDS14509例(其中由HIV发展为AIDS3844例),死亡9748例。平均每月新报告HIV约3800例。31个省(自治区、直辖市)已全部发现HIV感染者。在我国艾滋病已成为一个严重的社会和公共卫生问题,其流行病学特点主要表现为:
2.1时间分布特点 我国HIV/AIDS的流行历史可分为三个时期:1985~1988年被称为输入散发期,病例多数为境外输入性。1989~1994年被称为局部流行期,以云南省德宏州的瑞丽等个别地区发现静脉注射吸毒者中HIV感染呈聚集性为标志。1995年至今被称广泛流行期,其特征是:静脉注射吸毒人群中的HIV流行已在云南、四川等更多的地区出现,快速发展到大部分省;以中部数省为主的非法采供血人群中发生HIV感染,并经人口流动和二代传播扩散至更广大的地区;部分沿海地区和中心城市的性乱人群中HIV感染率越来越高。目前,由于政府采取了一系列坚决的措施,已经有效地控制了非法采供血行为,用血安全性得到最大限度的保障,但是经静脉注射吸毒和经性传播HIV的势头并未得到很好的控制,尤其是性传播已成为主要传播方式,其中又以男男同性恋人群为主,而且在一些地区已出现HIV感染者的第二代传播(母婴传播、家庭内性传播等),对全国HIV/AIDS的流行蔓延无疑起到推波助澜之作用。 2.2地区分布特点 艾滋病疫情在地区分布上很不均衡,2000年报告HIV感染者最多的4个省份:云南、新疆、广西和广东,合计报告人数占全国报病总数76.7%(3989/5201),经静脉注射毒品感染HIV是其主要的传播途径。而海南、福建等南部及东南沿海省份,以性传播为主。河南、山西、安徽等中部地区,感染者主要为有偿采供血人员及流动人口,感染途径多不详。
世界艾滋病日宣传标语
世界艾滋病日宣传标语 世界艾滋病日宣传标语 1、遏制艾滋,履行承诺 2、外出打工,预防艾滋 3、全民动员,遏制艾滋,共建和谐 4、政府主导,全民参与,共抗艾滋 5、预防艾滋,咨询检测,利己利人 6、远离毒品,预防艾滋,珍爱生命 7、同心携手,遏制艾滋,共建和谐 8、预防艾滋,主动咨询,检测 9、奉献爱心携手同行共抗艾滋 10、预防艾滋病,你我同参与 1 1、预防艾滋病,健康全家人 1 2、遏制艾滋病预防是关键 1 3、情系农民工,共抗艾滋病 1 4、爱心呵护生命,行动抵御艾滋 1 5、携手遏制艾滋,共建和谐社会 1
6、预防艾滋病,主动去咨询,做检测 1 7、正确使用安全套,避免共用注射器,有效预防艾滋病 1 8、深入贯彻落实科学发展观,依法推进艾滋病防治工作 1 9、依法推广使用安全套,有效预防性病艾滋病 20、关注艾滋病问题,关爱艾滋病病人 2 1、日常生活接触不会传播艾滋病 2 2、艾滋病经性接触、血液、母婴三条途径传播 2 3、防治艾滋病,国家有政策,艾滋病自愿咨询检测可 2 4、不安全性行为和共用注射器吸毒是促使艾滋病病毒传播的高危行为 附送: 世界读书日书香活动总结 世界读书日书香活动总结 201X世界读书日书香活动总结
书,是人类伟大的精神产物。鼓励孩子及家庭多读书、读好书,去发现读书的乐趣,唤起大家对这些为人类和社会文化进步做出不可替代贡献的伟人的再次敬仰,我们幼儿园组织了关于世界读书日的系列活动。 在4月23日这天,二楼的平台上搭建起了图书市场这些图书都是全园小朋友平日看过了的,或小时候看过的书。它们带到幼儿园,摆进了图书市场,进行第二次交易,使没看过的更多的小朋友受益。受书的是大班的二十一位小朋友,他们都对这个工作兢兢业业,认真的和收费。全园的其他小朋友,每人从自己积攒的零用钱中抽出几元钱,选购每本仅受一元的旧书,看着他们精挑细选、公平交易的表情,让我们对孩子的世界肃然起敬每一个孩子在他们的世界里他们都是大人。 通过这次活动,我们共募集到241本图书,售出207本,收到207元钱。孩子们由自己的亲身体验经历到的购买、阅读的过程,使他们更爱书、更爱护书 家长们更是对幼儿园的活动进行了支持。办这样的活动,不仅大家都非常理解和同,而且还有许多家长互相了使自己受益的图书,写出了读后感与大家分享。孩子们也用自己稚嫩的小手和简洁的语言,用拼音拼出自己看书的感受。读着这样一篇篇的文章,不由的内心非常感动: 正是由于家园间对教育的一致和相互的配合,才让孩子在活动中的到良好的锻炼和爱书、爱学的品质。 最后,我们评选出了这次系列活动中表现突出的孩子和家长,用图书义卖所募集到的207元,购买了新的好的图书奖励给他们,鼓励
2017艾滋病、性与健康智慧树期末考试90分
艾滋病、性与健康教程考试 名称艾滋病、性与健康 对应章节 成绩类型分数制 截止时间2017-01-08 23:59 题目数50 总分数100 说明: 提示:选择题选项顺序为随机排列,若要核对答案,请以选项内容为准 第1部分 总题数:50 1 【判断题】(2分) 各地设立的自愿咨询检测门诊能够提供资源咨询检测服务,且完全保密受检者的个人信息及检测结果。 A. 错 B. 对 2 【判断题】(2分) 在婚姻的前提下,成熟的性行为允许未经一方同意的强行性行为。 A. 错 B. 对 3 【多选题】(2分) 性别由哪些因素可以决定?
A. 第二性征 B. 社会行为 C. 基因 D. 心理特点 E. 社会文化 F. 性器官 4 【多选题】(2分) 弗洛伊德把性心理发展分为以下哪些阶段? A. 口腔期 B. 两性期 C. 性器期 D. 婚恋期 E. 潜伏期 F. 肛门期 5 【多选题】(2分) 性侵害的法律责任主要包括: A.
刑事责任 B. 违宪责任 C. 行政责任 D. 民事责任 6 【单选题】(2分) 我国每年新报告青少年学生艾滋病感染的主要传播途径是: A. 以静脉注射吸毒为主 B. 以同性传播为主 C. 以异性传播为主 7 【多选题】(2分) 以下样品中,可以用于进行HIV抗体检测的有: A. 唾液 B. 汗液 C. 血浆 D. 全血 E. 尿液 F. 血清 8
【多选题】(2分) 现代社会性别中男女共有的性别内容特点? A. 善解人意 B. 刚强 C. 温柔 D. 独立 E. 智慧 F. 细腻 9 【判断题】(2分) 性行为带来的后果,仅与性行为相关者的健康有关,不会涉及其他方面。 A. 对 B. 错 10 【判断题】(2分) 血液中的CD4+淋巴细胞低于500/微升是HIV感染者已经发病的标志。 A. 错 B. 对 11 【判断题】(2分) 通过网络、微信等新媒体实施的一些间接的性骚扰,不属于性暴力。 A. 对
艾滋病防治知识培训测试试题 (3)
艾滋病防治知识培训测试试题 (一)单选题 1、当HlV侵入机体后,未进入发病期者被称之为 A、艾滋病病人 B、艾滋病病毒感染者 C、窗口期 2、艾滋病病毒,是一种能生存于人的血液中并攻击的病毒。 A、免疫系统 B、神经系统 C、骨酪系统 D、肌肉系统 3、艾滋病病毒通过血液和血液制品传播的概率,大约是 %。 A、40 B、60 C、80 D、100 4、对艾滋病病毒易感的人群是。 A、静脉吸毒者 B、性乱者 C、同性恋者 D、每个人 5、对于HIV/AIDS的诊断最重要的是根据 A、临床表现 B、经确认HIV抗体阳性 C、具有高危行为 6、下列哪个不是艾滋病的传播途径: A、性接触 B、血、血制品、器官移植和污染的注射器 C、蚊虫叮咬 D、母婴垂直传播 7、下例哪项不是急性HIV感染的临床表现 A、发热 B、咽痛 C、淋巴结肿大 D、口腔真菌感染 8、艾滋病常见合并症有: A、PCPP B、隐球菌脑膜炎 C、弓形体感染 D、以上都是 9、HIV感染的确证实验是: A、免疫印迹法查HIV抗体 B、酶联免疫法查HTV抗体 C、PDR法检测HIV RNA D、流式细胞仪检测CD4细胞数 10、PCP首选治疗是: A、氟康唑 B、复万新诺明 C、戊烷脒 D、乙胺嘧啶 11、HIV感染人体后主要导致下列哪个系统损害: A、消化系统 B、免疫系统 C、循环系统 D、骨胳系统 12、HlV不可以用下列哪种方法杀灭: A、37度,10%漂白粉处理30分钟 B、56度,30分钟 C、焚烧 D、温室,3天 13、艾滋病毒不可以通过下列哪种方式传播 A、共用针头或注射器 B、性接触 C、日常生活接触 D、母婴传播
2016年世界艾滋病日宣传资料
2016年世界艾滋病日宣传资料 1. 什么是艾滋病? 艾滋病是由艾滋病病毒引起的一种慢性致死率极高的严重传染病,目前还没有彻底治愈的药物和方法,但可以预防。艾滋病的全称叫获得性免疫缺陷综合征。aids是艾滋病英文名的缩写。艾滋病是译音。艾滋病病毒侵入人体后,不断破坏人体的免疫功能,使人体发生多种难以治愈的感染和肿瘤,最终导致死亡。 2. 艾滋病是怎么发现的? 3. 艾滋病病毒是何时发现的? 起初只了解到,免疫缺陷是艾滋病的病理表现,对它的病因并不清楚。到1983年法国科学家蒙坦尼尔报告,从艾滋病前期患者的淋巴腺分离出一种病毒,命名为淋巴结病相关病毒。1986 年国际病毒命名委员会将此新病毒命名为人类免疫缺陷病毒,英文简称h iv,即艾滋病病毒。4. 艾滋病病毒有哪些主要特点? (1) 主要攻击机体的t淋巴细胞; (2) 一旦侵入机体细胞,病毒就与机体细胞的遗传物质整合在一起,终生难以消除; (3) 病毒基因多变; (4) 广泛存在于感染者的血液、精液、阴道分泌物以及乳汁、脑脊液和有神经症状者的脑组织中,尤以血液、精液、阴道分泌物中的浓度高; 唾液、尿液也可能有少量存在。 (5) 对乙肝病毒有效的消毒方法均可对艾滋病病毒有效;
(6) 感染者潜伏期长,病死率高; (7) 病毒基因组比已知的任何逆转录病毒基因都复杂。 5. 全球艾滋病流行情况 全球有290万人死于艾滋病,有430万人感染上艾滋病病毒。全球感染人数已达3950万人,其中230万是15岁以下的儿童。 6. 我国艾滋病疫情情况中国艾滋病流行具五大特点:——范围广,地区差异大。截至2014年11月底,报告艾滋病病毒感染人数累计超过3万例的有:河南和云南省;超过1万例的有广西、新疆自治区和广 东省;宁夏、青海、西藏三省(区)报告数低于100例。不同地区的吸毒、暗娼人群感染率存在较大差异。新疆、云南、四川等省(区)部分地区的注射吸毒人群感染率超过50%;而江苏、浙江、内蒙古、辽宁等省、区注射吸毒人群感染率低于5%。云南、重庆、湖南、广东、广西、四川等省(区、市)的一些地区暗娼人群的感染率超过1%。——艾滋病由高危行为人群向一般人群扩散。艾滋病正由吸毒、卖淫、嫖娼等高危行为人群向一般人群扩散。云南、河南、新疆等省(区)的部分地区,孕产妇、婚检及临床检测人群中的艾滋病病毒感染率已经达到或超过1%,已达到联合国艾滋病规划署界定的高流行水平。 ——存在艾滋病疫情进一步蔓延的危险。公众对艾滋病的了解依然很低,很多人不知道如何保护自己免受艾滋病侵害。国家疫情监测数据表明,有45.5%的注射吸毒者共用注射器,11%的吸毒者有危险性行为。艾滋病在吸毒人群和暗娼、嫖客人群之间的传播加剧。感染者的流动成为艾滋病疫情加快传播的重要因素。此外,大量人口流动、性乱行为增加以及很多城市增长的性病发病,也都成为促进艾滋病蔓延的重要因素。 联合国艾滋病规划署(un7. 全球艾滋病迅速传播的主要原因
艾滋病背景知识
艾滋病(AIDS)的定义 艾滋病,医学全名为“获得性免疫缺陷综合症”(Acquired Immune Deficiency Syndrome -- AIDS),是人体感染了人类免疫缺陷病毒(HIV),又称艾滋病病毒所导致的传染病。值得一提的是,HIV本身并不会引发任何疾病,而是当免疫系统被HIV破坏后,人体由于失去抵抗能力而感染其他的疾病导致死亡!通俗地讲,艾滋病就是人体的免疫系统被艾滋病病毒破坏,使人体对威胁生命的各种病原体丧失了抵抗能力,从而发生多种感染或肿瘤,最后导致死亡的一种严重传染病。这种病毒终生传染,破坏人的免疫系统,使人体丧失抵抗各种疾病的能力。当艾滋病病毒感染者的免疫功能受到病毒的严重破坏、以至不能维持最低的抗病能力时,感染者便发展为艾滋病病人。随着人体免疫力的降低,人会越来越频繁地感染上各种致病微生物,而且感染的程度也会变得越来越严重,最终会因各种复合感染而导致死亡。艾滋病主要通过血液、不正当的性行为、吸毒和母婴遗传四种途径传播。国际医学界至今尚无防治艾滋病的有效药物和疗法。因此,艾滋病也被称为“超级癌症”和“世纪杀手”。 艾滋病病毒简称HIV,是一种能攻击人体免疫系统的病毒。它把人体免疫系统中最重要的T4淋巴细胞作为攻击目标,大量吞噬、破坏T4淋巴细胞,从而破坏人的免疫系统,最终使免疫系统崩溃,使人体因丧失对各种疾病的抵抗能力而发病并死亡。科学家把这种病毒叫做“人类免疫缺陷病毒”。艾滋病病毒在人体内的潜伏期平均为12年至13年。在发展成艾滋病病人以前外表看上去正常,他们可以没有任何症状地生活和工作很多年。 艾滋病的英文缩写词AIDS的音译,曾译为“爱滋病”、“爱死病”。1981年在美国首次发现和确认。病毒侵入后,人体即丧失免疫功能,容易感染其它疾病而死亡。一般通过性接触、静脉注射及输血等途径传染。被称为“20世纪的瘟疫”。 艾滋病病毒与艾滋病的区别 HIV (艾滋病病毒)代表人类免役缺陷病毒。一个人感染了HIV 以后,此病毒就开始攻击人体免役系统,人体免役系统的一个功能是击退疾病。经过几年,HIV 削弱了免役系统,这个时候,人体就会感染上机会性感染病,如,肺炎,脑膜炎,肺结核。一旦有机会性感染发生,这个人就被认为是患了艾滋病。艾滋病(AIDS )代表获得性免役缺陷综合征。艾滋病本身不是一种病,而是一种无法抵抗其它疾病的状态或综合征状。人不会死于艾滋病,而是会死于与艾滋病相关的疾病。 艾滋病病毒感染者和艾滋病人的区别 艾滋病病毒感染者是指已经感染了艾滋病病毒,但是还没有表现出明显的临床症状,没有被确诊为艾滋病的人;艾滋病病人指的是已经感染了艾滋病病毒,并且已经出现了明显的临床症状,被确诊为艾滋病的人。二者之间的相同之处在于都携带艾滋病病毒,都具有传染性。不同之处在于艾滋病病人已经出现了明显的临床症状,而艾滋病病毒感染者还没有出现明显的临床症状,外表看起来跟健康人一样。这一时期叫做潜伏期,潜伏期为无症状感染期,本期除HIV抗体阳性外,无自觉症状和阳性体征。潜伏期长短不一,半年到12年不等,少数可达20年以上。艾滋病病毒在人体内的潜伏期平均为6年。 艾滋病的起源和发展 关于艾滋病的起源有很多传说,有人说是德国在二次世界大战时,人工研究出来的
2021年世界艾滋病日宣传知识
xx年世界艾滋病日宣传知识 xx年12月1日是第30个“世界艾滋病日”。活动主题为“共担防艾责任,共享健康权利,共建健康中国”。借此时机,向同学们宣传下艾滋病防治知识,以提高同学们防艾控艾的意识,提高防控艾滋病的能力。 一、艾滋病流行概况 自艾滋病病毒开始流行以来,在全世界已经有超过6000万人感染了艾滋病毒,其中2200万人已经死亡。近几年来全球每年有将近500万例艾滋病新感染者,每天有14000-15000例新的艾滋病病毒感染者,有8000人因艾滋病而死亡。我国自xx年发现首例艾滋病病人以来,艾滋病的流行不仅在蔓延,而且进入了快速增长阶段。 二、艾滋病迅速传播的主要原因 科学研究表明,艾滋病在当今世界各地迅猛传播,并不是艾滋病病毒突然变得强大了,而是由于人们生活方式在改变。主要有以下几点: (1)在同性恋人群中迅速传播; (2)广泛的世界性旅行,带病毒者很可能将艾滋病病毒从一个地方传播到另一个地方; (3)静脉吸毒者大量增加; (4)输血需求者增加; (5)人群的城乡流动频繁; (6)卖淫、数量增加,性乱行为增加。 三、艾滋病有哪些主要传播途径
主要传播途径有三种:经性接触传播、经血液传播和母婴传播。 四、不会传播HIV的途经 HIV不会通过空气及日常生活接触传播,如握手、拥抱、礼节性接吻、咳嗽、打喷嚏、一起喝茶、共同进餐、共用工具或办公用具、共用马桶、共用电话、一起游泳等均不会传播HIV,蚊虫叮咬也不会传播。 五、艾滋病的预防 目前艾滋病虽无法治愈,但因其传播途经明确,且易控制,对于一个真正懂得珍惜自己生命的人来说,要避免感染HIV并不困难。 1.预防性传播 (1)洁身自好,遵守性道德是预防HIV经性传播的关键措施。(2)提倡安全性行为。 (3)正确使用质量合格的安全套,可以有效减少感染艾滋病、性病的危险,每次性交都应使用。 2.预防血液传播 (1)注射毒品可因共用注射器引起HIV传染,因此绝对不可尝试吸毒。 (2)剃须刀、修脚刀和一些美容器械经常会使皮肤发生不易觉察的轻微擦伤,因此不要去消毒不严格的理发店、美容院、公共浴池等场所。 内容仅供参考
世界艾滋病日历届主题作文
世界艾滋病日历届主题作文 世界艾滋病日历届主题作文 导语:只有认识艾滋病,才能更好地防治,让我们行动起来,共同学习有关知识,使大家能尽快认识HIV这个人类的大敌,远离艾滋,同艾滋抗战到底。下面是小编整理的一些关于艾滋病的优秀作文,欢迎查阅,谢谢! 预防艾滋病 近年来,我们对艾滋病这个词可以说是即”熟悉”又”陌生”,熟悉是因为我们听到这个词的名字太多了,陌生是因为我们对艾滋病的了解和认识极少。 艾滋病是什么,说实话我并不太了解,但是我知道艾滋病并不像传闻中的那样可怕,这几天和同学们在一起研读了
一些关于艾滋病方面的内容,使我受益匪浅。 艾滋病是英文Acquirdmmumo---Deficioney Synderome 的缩写,中文全称为”获得性免疫缺陷综合病”,在很多国家艾滋病被称为”世界瘟疫”或现代的”黑死病”,尽管从发现到现在只有20余年的时间,但其已在全球大规模流行,其实已经证实一点艾滋病是可以预防的,日常生活接触并不能传染艾滋病,艾滋病传播有三条途径:”性传播、母婴传播、血液传播”,只要我们牢记就好,同时也要知道:共用游泳池、拥抱、同桌吃饭、共用餐具、共用办公办学用具等途径是不传播艾滋病的,因此艾滋病患者不应该被歧视。 艾滋病患者在生活中应被我们呵护关心,我相信他们的心里也同样害怕,假使我们不给他们关怀还歧视他们,那么他们还怎么有和病魔做斗争的勇气呢?我们应给予他们的是更多的鼓励,对他们所遭受的痛苦给予同情和帮助。这种宽容可以赢得社会各种人群的协作,使社会力量集中起来减少艾滋病的危害。
艾滋病是一个严重的传染家,关于艾滋病的问题不仅仅是复杂的医学问题,也是社会问题,需要我们每个人提高警惕,认真关注,关注艾滋病给人类造成的危害,并把我们通过研究性学习得到的知识向身边的人宣传,让更多的人意识到它的严重性。 只有认识艾滋病,才能更好地防治,让我们行动起来,共同学习有关知识,使大家能尽快认识HIV这个人类的大敌,远离艾滋,同艾滋抗战到底。 预防艾滋病作文800字 你,如同一粒尘土,悄悄地侵临在不幸者的身上。你,如同一个恶魔,凶恶地使不幸者悲痛绝望。你,如同一位死神,无情地剥夺了绝望者的灵魂。......虽然你如同死神一般恐怖,但你也是如死神害怕光明一样,是有弱点的。我们虽不能面对面地将你击倒,但我们知道,你降临于人的身上,也需要一定的途径。那么,我们就能在这些途径中,把你拒之门外。......但也许是因一部分人的堕落和疏忽,被你毁灭
