美国FDA批准说明书(原文)

HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use XARELTO? (rivaroxaban) safely and effectively. See full prescribing information for XARELTO
XARELTO (rivaroxaban) film-coated oral tablets
Initial U.S. Approval: 2011
WARNING: SURGICAL SETTINGS--
SPINAL/EPIDURAL HEMATOMA
Epidural or spinal hematomas may occur in patients who are anticoagulated and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
?use of indwelling epidural catheters
?concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, other anticoagulants
? a history of traumatic or repeated epidural or spinal punctures
? a history of spinal deformity or spinal surgery.
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary.
Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated for thromboprophylaxis [see Warnings and Precautions (5.1) and Drug Interactions (7)].
INDICATIONS AND USAGE
XARELTO is a factor Xa inhibitor indicated for the prophylaxis of deep vein thrombosis (DVT) which may lead to pulmonary embolism (PE) in patients undergoing knee or hip replacement surgery. (1)
DOSAGE AND ADMINISTRATION
?10 mg orally, once daily with or without food (2)
DOSAGE FORMS AND STRENGTHS
Tablet: 10 mg (3)
CONTRAINDICATIONS ?Hypersensitivity to XARELTO (4)
?Active major bleeding (4)
WARNINGS AND PRECAUTIONS
?Risk of bleeding: XARELTO can cause serious and fatal bleeding. Promptly evaluate signs and symptoms of blood loss. (5.2)
?Pregnancy related hemorrhage: Use XARELTO with caution in pregnant women due to the potential for obstetric hemorrhage and/or emergent delivery. Promptly evaluate signs and symptoms of blood loss. (5.3)
ADVERSE REACTIONS
The most common adverse reaction (>5%) was bleeding. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Pharmaceuticals, Inc. at 1-800-526-7736 or FDA at 1-800-FDA-1088 or https://www.360docs.net/doc/ce5398495.html,/medwatch.
To report SUSPECTED ADVERSE REACTIONS, contact at or FDA at 1-800-FDA-1088 or https://www.360docs.net/doc/ce5398495.html,/medwatch
DRUG INTERACTIONS
?Combined P-gp and strong CYP3A4 inhibitors: Avoid concomitant use unless the lack of a significant interaction is proven (7.1)
?Combined P-gp and weak or moderate CYP3A4 inhibitors: Avoid concomitant use unless the benefit outweighs the bleeding risk in patients with renal impairment (7.2)
?Combined P-gp and strong CYP3A4 inducers: Avoid concomitant use or consider an increased dose (2.1, 7.3)
?Anticoagulants: Avoid concomitant use (7.4)
?Clopidogrel: Avoid concomitant use unless the benefit outweighs the bleeding risk (7.6)
USE IN SPECIFIC POPULATIONS
?Nursing mothers: discontinue drug or discontinue nursing (8.3)
?Renal impairment: Avoid use in patients with severe impairment (CrCl <30 mL/min). Use with caution in moderate impairment (CrCl 30 to <50 mL/ min) (8.7)
?Hepatic impairment: Avoid use in patients with moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment or in patients with any degree of hepatic disease associated with coagulopathy (8.8)
See 17 for PATIENT COUNSELING INFORMATION
Revised: 07/2011
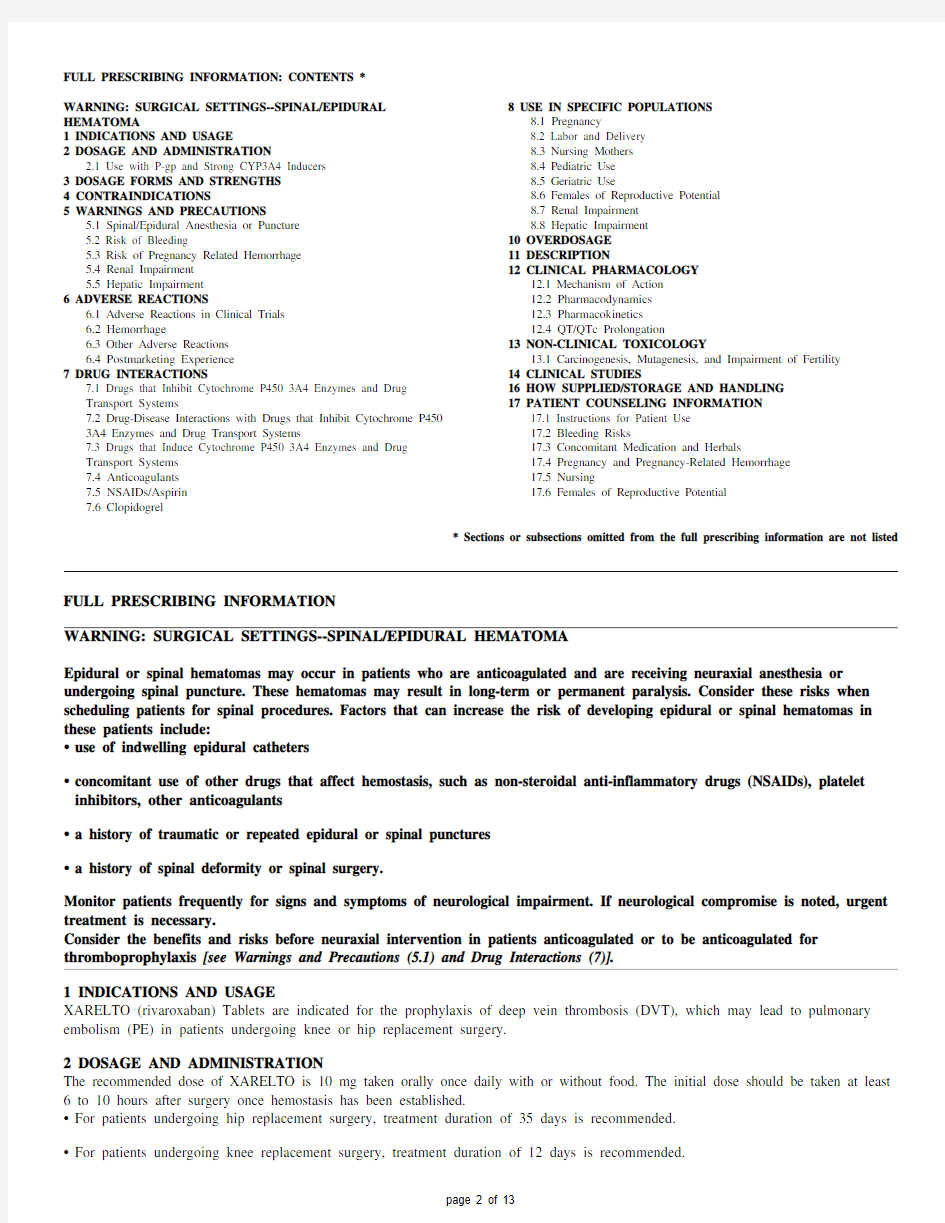
FULL PRESCRIBING INFORMATION: CONTENTS *
WARNING: SURGICAL SETTINGS--SPINAL/EPIDURAL HEMATOMA
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Use with P-gp and Strong CYP3A4 Inducers
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Spinal/Epidural Anesthesia or Puncture
5.2 Risk of Bleeding
5.3 Risk of Pregnancy Related Hemorrhage
5.4 Renal Impairment
5.5 Hepatic Impairment
6 ADVERSE REACTIONS
6.1 Adverse Reactions in Clinical Trials
6.2 Hemorrhage
6.3 Other Adverse Reactions
6.4 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Drugs that Inhibit Cytochrome P450 3A4 Enzymes and Drug
Transport Systems
7.2 Drug-Disease Interactions with Drugs that Inhibit Cytochrome P450
3A4 Enzymes and Drug Transport Systems
7.3 Drugs that Induce Cytochrome P450 3A4 Enzymes and Drug
Transport Systems
7.4 Anticoagulants
7.5 NSAIDs/Aspirin
7.6 Clopidogrel
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Females of Reproductive Potential
8.7 Renal Impairment
8.8 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 QT/QTc Prolongation
13 NON-CLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, and Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Instructions for Patient Use
17.2 Bleeding Risks
17.3 Concomitant Medication and Herbals
17.4 Pregnancy and Pregnancy-Related Hemorrhage
17.5 Nursing
17.6 Females of Reproductive Potential
* Sections or subsections omitted from the full prescribing information are not listed
FULL PRESCRIBING INFORMATION
WARNING: SURGICAL SETTINGS--SPINAL/EPIDURAL HEMATOMA
Epidural or spinal hematomas may occur in patients who are anticoagulated and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
?use of indwelling epidural catheters
?concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, other anticoagulants
?a history of traumatic or repeated epidural or spinal punctures
?a history of spinal deformity or spinal surgery.
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary.
Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated for thromboprophylaxis [see Warnings and Precautions (5.1) and Drug Interactions (7)].
1 INDICATIONS AND USAGE
XARELTO (rivaroxaban) Tablets are indicated for the prophylaxis of deep vein thrombosis (DVT), which may lead to pulmonary embolism (PE) in patients undergoing knee or hip replacement surgery.
2 DOSAGE AND ADMINISTRATION
The recommended dose of XARELTO is 10 mg taken orally once daily with or without food. The initial dose should be taken at least 6 to 10 hours after surgery once hemostasis has been established.
?For patients undergoing hip replacement surgery, treatment duration of 35 days is recommended.
?For patients undergoing knee replacement surgery, treatment duration of 12 days is recommended.
If a dose of XARELTO is not taken at the scheduled time, the dose should be taken as soon as possible on the same day and continued on the following day with the once daily intake as recommended.
Administration via GI feeding tube:
Rivaroxaban absorption is dependent on the site of drug release in the gastrointestinal (GI) tract (gastric versus small intestine). When administering XARELTO as a crushed tablet via a feeding tube, confirm gastric placement of the tube [see Clinical Pharmacology (12.3)].
2.1 Use with P-gp and Strong CYP3A4 Inducers
Concomitant use of XARELTO with drugs that are combined P-gp and strong CYP3A4 inducers (e.g., carbamazepine, phenytoin, rifampin, St. John's wort) should be avoided. A XARELTO dose increase to 20 mg (i.e., two 10 mg tablets) should be considered
if these drugs must be coadministered. The 20 mg dose should be taken with food [see Drug Interactions (7.3) and Clinical Pharmacology (12.3)].
3 DOSAGE FORMS AND STRENGTHS
XARELTO 10 mg tablets are round, light red, biconvex and film-coated with a triangle pointing down above a "10" marked on one side and "Xa" on the other side.
4 CONTRAINDICATIONS
XARELTO is contraindicated in patients with:
?hypersensitivity to XARELTO
?active major bleeding [see Warnings and Precautions (5.2)]
5 WARNINGS AND PRECAUTIONS
5.1 Spinal/Epidural Anesthesia or Puncture
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents for prevention of thromboembolic complications are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis [see Boxed Warning].
An epidural catheter should not be removed earlier than 18 hours after the last administration of XARELTO. The next XARELTO dose is not to be administered earlier than 6 hours after the removal of the catheter. If traumatic puncture occurs, the administration of XARELTO is to be delayed for 24 hours.
5.2 Risk of Bleeding
XARELTO increases the risk of bleeding and can cause serious and fatal bleeding. Major hemorrhages including intracranial, epidural hematoma, gastrointestinal, retinal, and adrenal bleeding have been reported. Use XARELTO with caution in conditions with increased risk of hemorrhage.
Concomitant use of drugs affecting hemostasis increases the risk of bleeding. These include platelet aggregation inhibitors, other antithrombotic agents, fibrinolytic therapy, thienopyridines and chronic use of non-steroidal anti-inflammatory drugs (NSAIDs) [see Drug Interactions (7.4), (7.5), (7.6)].
Bleeding can occur at any site during therapy with XARELTO. An unexplained fall in hematocrit or blood pressure should lead to a search for a bleeding site. Promptly evaluate any signs or symptoms of blood loss.
5.3 Risk of Pregnancy Related Hemorrhage
XARELTO should be used with caution in pregnant women and only if the potential benefit justifies the potential risk to the mother and fetus. XARELTO dosing in pregnancy has not been studied. The anticoagulant effect of XARELTO cannot be monitored with standard laboratory testing nor readily reversed. Promptly evaluate any signs or symptoms suggesting blood loss (e.g., a drop in hemoglobin and/or hematocrit, hypotension, or fetal distress).
5.4 Renal Impairment
Avoid the use of XARELTO in patients with severe renal impairment (creatinine clearance <30 mL/min) due to an expected increase in rivaroxaban exposure and pharmacodynamic effects in this patient population.
Observe closely and promptly evaluate any signs or symptoms of blood loss in patients with moderate renal impairment (CrCl 30 to <50 mL/min). Patients who develop acute renal failure while on XARELTO should discontinue the treatment [see Use in Specific Populations (8.7)].
5.5 Hepatic Impairment
Clinical data in patients with moderate hepatic impairment indicate a significant increase in rivaroxaban exposure and pharmacodynamic effects. No clinical data are available for patients with severe hepatic impairment. Avoid use of XARELTO in patients with moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment or with any hepatic disease associated with coagulopathy [see Use in Specific Populations (8.8)].
6 ADVERSE REACTIONS
6.1 Adverse Reactions in Clinical Trials
In three randomized, controlled clinical trials (RECORD 1–3) in elective joint replacement surgery, 4487 patients received XARELTO 10 mg orally once daily. The mean duration of XARELTO treatment was 11.9 days in the total knee replacement study and 33.4 days in the total hip replacement studies. Overall, the mean age of the patients studied in the XARELTO group was 64 years, 59% were female and 82% were Caucasian. Twenty-seven percent (1206) of patients underwent knee replacement surgery and 73% (3281) underwent hip replacement surgery.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In the RECORD clinical trials, the overall incidence rate of adverse reactions leading to permanent treatment discontinuation was
3.7% with XARELTO.
6.2 Hemorrhage
The most common adverse reactions with XARELTO were bleeding complications [see Warnings and Precautions (5.2)]. The rates of major bleeding events and any bleeding events observed in patients in the RECORD clinical trials are shown in Table 1.
Table 1: Bleeding Events* in Patients Undergoing Hip or Knee Replacement Surgeries (RECORD 1–3)
XARELTO 10 mg Enoxaparin?
Total treated patients N = 4487
n (%)N = 4524 n (%)
Major bleeding event 14 (0.3) 9 (0.2) Fatal bleeding 1 (<0.1) 0
Bleeding into a critical organ 2 (<0.1) 3 (0.1) Bleeding that required re-operation 7 (0.2) 5 (0.1) Extra-surgical site bleeding requiring transfusion
of >2 units of whole blood or packed cells
4 (0.1) 1 (<0.1) Any bleeding event?261 (5.8) 251 (5.6)
Hip Surgery Studies N = 3281
n (%)N = 3298 n (%)
Major bleeding event 7 (0.2) 3 (0.1) Fatal bleeding 1 (<0.1) 0
Bleeding into a critical organ 1 (<0.1) 1 (<0.1) Bleeding that required re-operation 2 (0.1) 1 (<0.1) Extra-surgical site bleeding requiring transfusion
of >2 units of whole blood or packed cells
3 (0.1) 1 (<0.1) Any bleeding event?201 (6.1) 191 (5.8)
Knee Surgery Study N = 1206
n (%)N = 1226 n (%)
Major bleeding event 7 (0.6) 6 (0.5)
Fatal bleeding 0 0
Bleeding into a critical organ 1 (0.1) 2 (0.2)
Bleeding that required re-operation 5 (0.4) 4 (0.3)
Extra-surgical site bleeding requiring transfusion
of >2 units of whole blood or packed cells
1 (0.1) 0
Any bleeding event?60 (5.0) 60 (4.9)
*Bleeding events occurring any time following the first dose of double-blind study medication (which may have been prior to administration of active drug) until two days after the last dose of double-blind study medication. Patients may have more than one event.
?Includes the placebo-controlled period for RECORD 2, enoxaparin dosing was 40 mg once daily (RECORD 1–3)
?Includes major bleeding events
Following XARELTO treatment, the majority of major bleeding complications (≥60%) occurred during the first week after surgery.
6.3 Other Adverse Reactions
Table 2 shows other adverse drug reactions (ADRs) reported in ≥1% of XARELTO-treated patients in the RECORD clinical studies. Table 2: Other Adverse Drug Reactions* Reported by ≥1% of XARELTO-Treated Patients in RECORD 1–3 Studies
System/Organ Class Adverse Reaction XARELTO
10 mg
(N = 4487)
n (%)
Enoxaparin?
(N = 4524)
n (%)
Injury, poisoning and procedural complications
Wound secretion 125 (2.8) 89 (2.0) Musculoskeletal and connective tissue disorders
Pain in extremity 74 (1.7) 55 (1.2)
Muscle spasm 52 (1.2) 32 (0.7)
Nervous system disorders
Syncope 55 (1.2) 32 (0.7)
Skin and subcutaneous tissue disorders
Pruritus 96 (2.1) 79 (1.8)
Blister 63 (1.4) 40 (0.9)
drug, until two days after the last dose of double-blind study medication.
?Includes the placebo-controlled period of RECORD 2, enoxaparin dosing was 40 mg once daily (RECORD 1–3)
The following ADR occurred in <1% of XARELTO-treated patients in the clinical studies:
Renal and urinary disorders: dysuria
The laboratory abnormalities in Table 3 were observed in clinical studies:
Table 3: Laboratory Abnormalities in RECORD 1–3 Clinical Studies
Laboratory Abnormality XARELTO
10 mg
Enoxaparin*
Alanine aminotransferase >3 × ULN 114/4441 (2.6%) 167/4456 (3.8%) Aspartate aminotransferase >3 × ULN 122/4441 (2.8%) 152/4456 (3.4%)
Total bilirubin >1.5 × ULN 140/4442 (3.2%) 128/4456 (2.9%) Gamma-glutamyltransferase >3 × ULN 292/4442 (6.6%) 391/4457 (8.8%) Platelet counts <100,000/mm3 or <50% of baseline
value
116/4425 (2.6%) 131/4447 (3.0%)
*Includes the placebo-controlled period of RECORD 2, enoxaparin dosing was 40 mg once daily (RECORD 1–3)
6.4 Postmarketing Experience
The following additional adverse reactions have been reported in countries where XARELTO has been marketed. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: agranulocytosis
Gastrointestinal disorders: retroperitoneal hemorrhage
Hepatobiliary disorders: jaundice, cholestasis, cytolytic hepatitis
Immune system disorder: hypersensitivity, anaphylactic reaction, anaphylactic shock
Nervous system disorders: cerebral hemorrhage, subdural hematoma, epidural hematoma, hemiparesis
Skin and subcutaneous tissue disorders: Stevens-Johnson syndrome
7 DRUG INTERACTIONS
Rivaroxaban is a substrate of CYP3A4/5, CYP2J2, and the P-gp and ATP-binding cassette G2 (ABCG2) transporters. Inhibitors and inducers of these CYP450 enzymes or transporters may result in changes in rivaroxaban exposure.
7.1 Drugs that Inhibit Cytochrome P450 3A4 Enzymes and Drug Transport Systems
In drug interaction studies evaluating the concomitant use with drugs that are combined P-gp and CYP3A4 inhibitors, increases
in rivaroxaban exposure and pharmacodynamic effects (i.e., factor Xa inhibition and PT prolongation) were observed. Significant increases in rivaroxaban exposure may increase bleeding risk.
?Ketoconazole (combined P-gp and strong CYP3A4 inhibitor): Steady-state rivaroxaban AUC and C max increased by 160% and 70%, respectively. Similar increases in pharmacodynamic effects were also observed.
?Ritonavir (combined P-gp and strong CYP3A4 inhibitor): Single-dose rivaroxaban AUC and C max increased by 150% and 60%, respectively. Similar increases in pharmacodynamic effects were also observed.
?Clarithromycin (combined P-gp and strong CYP3A4 inhibitor): Single-dose rivaroxaban AUC and C max increased by 50% and 40%, respectively. The smaller increases in exposure observed for clarithromycin compared to ketoconazole or ritonavir may be due to the relative difference in P-gp inhibition.
?Erythromycin (combined P-gp and moderate CYP3A4 inhibitor): Both the single-dose rivaroxaban AUC and C max increased by 30%.
Avoid concomitant administration of XARELTO with combined P-gp and strong CYP3A4 inhibitors (e.g., ketoconazole, itraconazole, lopinavir/ritonavir, ritonavir, indinavir/ritonavir, and conivaptan) which cause significant increases in rivaroxaban exposure that may increase bleeding risk.
When clinical data suggest a change in exposure is unlikely to affect bleeding risk (e.g., clarithromycin, erythromycin), no precautions are necessary during coadministration with drugs that are combined P-gp and CYP3A4 inhibitors.
7.2 Drug-Disease Interactions with Drugs that Inhibit Cytochrome P450 3A4 Enzymes and Drug Transport Systems
Based on simulated pharmacokinetic data, patients with renal impairment receiving XARELTO with drugs that are combined P-gp and weak or moderate CYP3A4 inhibitors (e.g., erythromycin, azithromycin, diltiazem, verapamil, quinidine, ranolazine, dronedarone, amiodarone, and felodipine), may have significant increases in exposure compared with patients with normal renal function and no inhibitor use, since both pathways of rivaroxaban elimination are affected. Since these increases may increase bleeding risk, use XARELTO in this situation only if the potential benefit justifies the potential risk [see Use in Specific Populations (8.7)].
7.3 Drugs that Induce Cytochrome P450 3A4 Enzymes and Drug Transport Systems
In a drug interaction study, co-administration of XARELTO (20 mg single dose with food) with a drug that is a combined P-gp and strong CYP3A4 inducer (rifampicin titrated up to 600 mg once daily) led to an approximate decrease of 50% and 22% in AUC and
C max, respectively. Similar decreases in pharmacodynamic effects were also observed. These decreases in exposure to rivaroxaban may decrease efficacy.
Avoid concomitant use of XARELTO with drugs that are combined P-gp and strong CYP3A4 inducers (e.g., carbamazepine, phenytoin, rifampin, St. John's wort). Consider increasing the XARELTO dose if these drugs must be coadministered [see Dosage and Administration (2.1)].
7.4 Anticoagulants
In a drug interaction study, single doses of enoxaparin (40 mg subcutaneous) and XARELTO (10 mg) given concomitantly resulted in an additive effect on anti-factor Xa activity. Enoxaparin did not affect the pharmacokinetics of rivaroxaban. In another study, single doses of warfarin (15 mg) and XARELTO (5 mg) resulted in an additive effect on factor Xa inhibition and PT. Warfarin did not affect the pharmacokinetics of rivaroxaban. The safety of long-term concomitant use of these drugs has not been studied.
Avoid concurrent use of XARELTO with other anticoagulants due to the increased bleeding risk other than during therapeutic transition periods where patients should be observed closely. Promptly evaluate any signs or symptoms of blood loss [see Warnings and Precautions (5.2)].
7.5 NSAIDs/Aspirin
In a single-dose drug interaction study there were no pharmacokinetic or pharmacodynamic interactions observed after concomitant administration of naproxen or aspirin (acetylsalicylic acid) with XARELTO. The safety of long-term concomitant use of these drugs has not been studied.
NSAIDs/aspirin are known to increase bleeding, and bleeding risk may be increased when these drugs are used concomitantly with XARELTO.
Promptly evaluate any signs or symptoms of blood loss if patients are treated concomitantly with NSAIDs and/or platelet aggregation inhibitors [see Warnings and Precautions (5.2)].
7.6 Clopidogrel
In two drug interaction studies where clopidogrel (300 mg loading dose followed by 75 mg daily maintenance dose) and XARELTO (15 mg single dose) were co-administered in healthy subjects, an increase in bleeding time to 45 minutes was observed in approximately 45% and 30% of subjects in these studies, respectively. The change in bleeding time was approximately twice the maximum increase seen with either drug alone. There was no change in the pharmacokinetics of either drug.
Avoid concurrent administration of clopidogrel with XARELTO unless the benefit outweighs the risk of increased bleeding [see Warnings and Precautions (5.2)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate or well-controlled studies of XARELTO in pregnant women, and dosing for pregnant women has not been established. Use XARELTO with caution in pregnant patients because of the potential for pregnancy related hemorrhage and/or emergent delivery with an anticoagulant that is not readily reversible. The anticoagulant effect of XARELTO cannot be reliably monitored with standard laboratory testing. Animal reproduction studies showed no increased risk of structural malformations, but increased post-implantation pregnancy loss occurred in rabbits. XARELTO should be used during pregnancy only if the potential benefit justifies the potential risk to mother and fetus.
Rivaroxaban crosses the placenta in animals. Animal reproduction studies have shown pronounced maternal hemorrhagic complications in rats and an increased incidence of post-implantation pregnancy loss in rabbits. Rivaroxaban increased fetal toxicity (increased resorptions, decreased number of live fetuses, and decreased fetal body weight) when pregnant rabbits were given oral doses of ≥10 mg/kg rivaroxaban during the period of organogenesis. This dose corresponds to about 11 times the human exposure of unbound drug, based on AUC comparisons at the maximum recommended human dose of 10 mg/day. Fetal body weights decreased when pregnant rats were given oral doses of 120 mg/kg. This dose corresponds to about 40 times the human exposure of unbound drug.
8.2 Labor and Delivery
Safety and effectiveness of rivaroxaban during labor and delivery have not been studied in clinical trials. However, in animal studies maternal bleeding and maternal and fetal death occurred at the rivaroxaban dose of 40 mg/kg (about 17 times maximum human exposure of the unbound drug at the human dose of 10 mg/day).
8.3 Nursing Mothers
It is not known if rivaroxaban is excreted in human milk. Rivaroxaban and/or its metabolites were excreted into the milk of rats. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from rivaroxaban, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of patients in the RECORD 1–3 clinical studies evaluating XARELTO, about 53% were 65 years and over, while about 15% were >75 years. In clinical trials the efficacy of XARELTO in the elderly (65 years or older) was similar to that seen in patients younger than 65 years.
Elderly subjects exhibited an increase in exposure that may be caused by age related changes in renal function. For patients 65 years of age and older, consideration should be given to assessment of renal function prior to starting therapy with XARELTO. Promptly evaluate any signs or symptoms of blood loss [see Clinical Pharmacology (12.3)].
8.6 Females of Reproductive Potential
Females of reproductive potential requiring anticoagulation should discuss pregnancy planning with their physician.
8.7 Renal Impairment
The safety and pharmacokinetics of single-dose XARELTO (10 mg) were evaluated in a study in healthy subjects [CrCl ≥80 mL/min (n=8)] and in subjects with varying degrees of renal impairment (see Table 4). Compared to healthy subjects with normal creatinine clearance, rivaroxaban exposure increased in subjects with renal impairment. Increases in pharmacodynamic effects were also observed.
Table 4: Percent Increase of Rivaroxaban PK and PD Parameters from Normal in Subjects with Renal Insufficiency from a Dedicated Renal Impairment Study
Renal Impairment Class
[CrCl (mL/min)]
Parameter Mild
[50 to 79]
N=8 Moderate
[30 to 49]
N=8
Severe
[15 to 29]
N=8
Exposure AUC44 52 64 (% increase relative to normal)C max28 12 26 FXa Inhibition AUC50 86 100
(% increase relative to normal) E max 9 10 12 PT Prolongation
AUC 33 116 144 (% increase relative to normal)
E max
4
17
20
PT = Prothrombin time; FXa = Coagulation factor Xa; AUC = Area under the concentration or effect curve; C max = maximum concentration; E max = maximum effect; and CrCl = creatinine clearance
Patients with any degree of renal impairment with concurrent use of P-gp and weak to moderate CYP3A4 inhibitors may have significant increases in exposure which may increase bleeding risk [see Drug Interactions (7.2)].
The combined analysis of the RECORD 1–3 clinical efficacy studies did not show an increase in bleeding risk for patients with moderate renal impairment and reported a possible increase in total VTE in this population. Observe closely and promptly evaluate any signs or symptoms of blood loss in patients with moderate renal impairment (CrCl 30 to <50 mL/min). Avoid the use of XARELTO in patients with severe renal impairment (CrCl <30 mL/min) [see Warnings and Precautions (5.2, 5.4)].
8.8 Hepatic Impairment
The safety and pharmacokinetics of single-dose XARELTO (10 mg) were evaluated in a study in healthy subjects (n=16) and subjects with varying degrees of hepatic impairment (see Table 5). No patients with severe hepatic impairment (Child-Pugh C) were https://www.360docs.net/doc/ce5398495.html,pared to healthy subjects with normal liver function, significant increases in rivaroxaban exposure were observed in subjects with moderate hepatic impairment (Child-Pugh B). Increases in pharmacodynamic effects were also observed.
Table 5: Percent Increase of Rivaroxaban PK and PD Parameters from Normal in Subjects with Hepatic Insufficiency from a Dedicated Hepatic Impairment Study
Hepatic Impairment Class
(Child-Pugh Class)
Parameter Mild (Child-Pugh A)N=8 Moderate
(Child-Pugh B)
N=8
Exposure AUC 15 127
(% increase relative to normal) C max 0 27
FXa Inhibition
AUC 8 159 (% increase relative to normal) E max 0 24 PT Prolongation
AUC 6 114 (% increase relative to normal)
E max
2
41
PT = Prothrombin time; FXa = Coagulation factor Xa; AUC = Area under the concentration or effect curve; C max = maximum concentration; E max = maximum effect
Avoid the use of XARELTO in patients with moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment or with any hepatic disease associated with coagulopathy [see Warnings and Precautions (5.2, 5.5)].
10 OVERDOSAGE
Overdose of XARELTO may lead to hemorrhage. A specific antidote of rivaroxaban is not available. Discontinue XARELTO and initiate appropriate therapy if bleeding complications associated with overdosage occur. The use of activated charcoal to reduce
absorption in case of XARELTO overdose may be considered. Due to the high plasma protein binding, rivaroxaban is not expected to be dialyzable [see Clinical Pharmacology (12.3)].
11 DESCRIPTION
Rivaroxaban, a factor Xa inhibitor, is the active ingredient in XARELTO Tablets with the chemical name 5-Chloro-N-({(5S)-2-oxo-3-[4-(3-oxo-4-morpholinyl)phenyl]-1,3-oxazolidin-5-yl}methyl)-2-thiophenecarboxamide. The molecular formula of rivaroxaban is C 19H 18ClN 3O 5
S and the molecular weight is 435.89. The structural formula is:
Rivaroxaban is a pure (S )-enantiomer. It is an odorless, non-hygroscopic, white to yellowish powder. Rivaroxaban is only slightly soluble in organic solvents (e.g., acetone, polyethylene glycol 400) and is practically insoluble in water and aqueous media.Each XARELTO tablet contains 10 mg of rivaroxaban. The inactive ingredients of XARELTO are: Microcrystalline cellulose,croscarmellose sodium, hypromellose, lactose monohydrate, magnesium stearate, sodium lauryl sulfate, and Opadry ? Pink, a proprietary filmcoating mixture containing polyethylene glycol 3350, hypromellose, titanium dioxide, and ferric oxide red.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
XARELTO is an orally bioavailable factor Xa inhibitor that selectively blocks the active site of factor Xa and does not require a cofactor (such as Anti-thrombin III) for activity. Activation of factor X to factor Xa (FXa) via the intrinsic and extrinsic pathways plays a central role in the cascade of blood coagulation.
12.2 Pharmacodynamics
Dose-dependent inhibition of factor Xa activity was observed in humans and the Neoplastin? prothrombin time (PT), activated partial thromboplastin time (aPTT) and HepTest? are prolonged dose-dependently. Anti-factor Xa activity is also influenced by rivaroxaban. There are no data on the use of the International Normalized Ratio (INR). The predictive value of these coagulation parameters for bleeding risk or efficacy has not been established.
12.3 Pharmacokinetics
Absorption
The absolute bioavailability of rivaroxaban is high (estimated to be 80% to 100%) for the 10 mg dose. Rivaroxaban is rapidly absorbed with maximum concentrations (C max) appearing 2 to 4 hours after tablet intake.
Rivaroxaban pharmacokinetics are linear with no relevant accumulation beyond steady-state after multiple doses. Intake with food does not affect rivaroxaban AUC or C max at the 10 mg dose.
The pharmacokinetics of rivaroxaban were not affected by drugs altering gastric pH. Coadministration of XARELTO (30 mg single dose) with the H2-receptor antagonist ranitidine (150 mg twice daily) or the antacid aluminum hydroxide/magnesium hydroxide (10 mL) did not show an effect on the bioavailability and exposure of rivaroxaban.
Absorption of rivaroxaban is dependent on the site of drug release in the GI tract. A 29% and 56% decrease in AUC and C max compared to tablet was reported when rivaroxaban granulate is released in proximal small intestine. Exposure is further reduced when drug is released in the distal small intestine, or ascending colon. Avoid administration of rivaroxaban via a method that could deposit drug directly into the proximal small intestine (e.g., feeding tube) which can result in reduced absorption and related drug exposure [see Dosage and Administration (2)].
Distribution
Plasma protein binding of rivaroxaban in human plasma is approximately 92% to 95%, with albumin being the main binding component. The steady-state volume of distribution in healthy subjects is approximately 50 L.
Metabolism
Approximately 51% of an orally administered [14C]-rivaroxaban dose was recovered as metabolites in urine (30%) and feces (21%). Oxidative degradation catalyzed by CYP3A4/5 and CYP2J2 and hydrolysis are the major sites of biotransformation. Unchanged rivaroxaban was the predominant moiety in plasma with no major or active circulating metabolites.
Excretion
Following oral administration of a [14C]-rivaroxaban dose, 66% of the radioactive dose was recovered in urine (36% as unchanged drug) and 28% was recovered in feces (7% as unchanged drug). Unchanged drug is excreted into urine, mainly via active tubular secretion and to a lesser extent via glomerular filtration (approximate 5:1 ratio). Rivaroxaban is a substrate of the efflux transporter proteins P-gp and ABCG2 (also abbreviated Bcrp). Rivaroxaban's affinity for influx transporter proteins is unknown.
Rivaroxaban is a low-clearance drug, with a systemic clearance of approximately 10 L/hr in healthy volunteers following intravenous administration. The terminal elimination half-life of rivaroxaban is 5 to 9 hours in healthy subjects aged 20 to 45 years.
Special Populations
Gender
Gender did not influence the pharmacokinetics or pharmacodynamics of XARELTO.
Race
Healthy Japanese subjects were found to have 50% higher exposures compared to other ethnicities including Chinese.
Elderly
In clinical studies, elderly subjects exhibited higher rivaroxaban plasma concentrations than younger subjects with mean AUC values
being approximately 50% higher, mainly due to reduced (apparent) total body and renal clearance. Age related changes in renal
function may play a role in this age effect. The terminal elimination half-life is 11 to 13 hours in the elderly [see Use in Specific
Populations (8.5)].
Body Weight
Extremes in body weight (<50 kg or >120 kg) did not influence rivaroxaban exposure.
Drug Interactions
In vitro studies indicate that rivaroxaban neither inhibits the major cytochrome P450 enzymes CYP1A2, 2C8, 2C9, 2C19, 2D6, 2J2,
and 3A4 nor induces CYP1A2, 2B6, 2C19, or 3A4.
In vitro data also indicates a low rivaroxaban inhibitory potential for P-gp and ABCG2 transporters.
In addition, there were no significant pharmacokinetic interactions observed in studies comparing concomitant rivaroxaban 20 mg
and 7.5 mg single dose of midazolam (substrate of CYP3A4), 0.375 mg once-daily dose of digoxin (substrate of P-gp), or 20 mg once
daily dose of atorvastatin (substrate of CYP3A4 and P-gp) in healthy volunteers.
12.4 QT/QTc Prolongation
In a thorough QT study in healthy men and women aged 50 years and older, no QTc prolonging effects were observed for XARELTO
(15 mg and 45 mg, single-dose).
13 NON-CLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, and Impairment of Fertility
Rivaroxaban was not carcinogenic when administered by oral gavage to mice or rats for up to 2 years. The systemic exposures
(AUCs) of unbound rivaroxaban in male and female mice at the highest dose tested (60 mg/kg/day) were 3- and 5-times, respectively,
the human exposure of unbound drug at the human dose of 10 mg/day. Systemic exposures of unbound drug in male and female rats at
the highest dose tested (60 mg/kg/day) were 4- and 10-times, respectively, the human exposure.
Rivaroxaban was not mutagenic in bacteria (Ames-Test) or clastogenic in V79 Chinese hamster lung cells in vitro or in the mouse
micronucleus test in vivo.
No impairment of fertility was observed in male or female rats when given up to 200 mg/kg/day of rivaroxaban orally. This dose
resulted in exposure levels, based on the unbound AUC, at least 33 times the exposure in humans given 10 mg rivaroxaban daily.
14 CLINICAL STUDIES
XARELTO was studied in 9011 patients (4487 XARELTO-treated, 4524 enoxaparin-treated patients) in the RECORD 1, 2, and 3
studies.
The two randomized, double-blind, clinical studies (RECORD 1 and 2) in patients undergoing elective total hip replacement surgery
compared XARELTO 10 mg once daily starting at least 6 to 8 hours (about 90% of patients dosed 6 to 10 hours) after wound closure
versus enoxaparin 40 mg once daily started 12 hours preoperatively. In RECORD 1 and 2, a total of 6727 patients were randomized
and 6579 received study drug. The mean age [± standard deviation (SD)] was 63 ± 12.2 (range 18 to 93) years with 49% of patients ≥65 years and 55% of patients were female. More than 82% of patients were White, 7% were Asian, and less than 2% were Black. The studies excluded patients undergoing staged bilateral total hip replacement, patients with severe renal impairment defined as an
estimated creatinine clearance <30 mL/min, or patients with significant liver disease (hepatitis or cirrhosis). In RECORD 1, the mean
exposure duration (± SD) to active XARELTO and enoxaparin was 33.3 ± 7.0 and 33.6 ± 8.3 days, respectively. In RECORD 2, the
mean exposure duration to active XARELTO and enoxaparin was 33.5 ± 6.9 and 12.4 ± 2.9 days, respectively. After Day 13, oral
placebo was continued in the enoxaparin group for the remainder of the double-blind study duration. The efficacy data for RECORD 1
and 2 are provided in Table 6.
Table 6: Summary of Key Efficacy Analysis Results for Patients Undergoing Total Hip Replacement Surgery - Modified Intent-to-Treat Population
RECORD 1 RECORD 2
Treatment Dosage and Duration XARELTO
10 mg once
daily
Enoxaparin
40 mg once
daily
RRR*,
p-value
XARELTO
10 mg once
daily
Enoxaparin?
40 mg once
daily
RRR*,
p-value
Number of Patients N = 1513N = 1473N = 834N = 835
Total VTE 17 (1.1%) 57 (3.9%) 71% (95%
CI: 50, 83),
p<0.001 17 (2.0%) 70 (8.4%) 76% (95%
CI: 59, 86),
p<0.001
Components of Total VTE
Proximal DVT 1 (0.1%) 31 (2.1%) 5 (0.6%) 40 (4.8%) Distal DVT 12 (0.8%) 26 (1.8%) 11 (1.3%) 43 (5.2%) Non-fatal PE 3 (0.2%) 1 (0.1%) 1 (0.1%) 4 (0.5%) Death (any cause) 4 (0.3%) 4 (0.3%) 2 (0.2%) 4 (0.5%) Number of Patients N= 1600N = 1587N= 928N = 929
Major VTE? 3 (0.2%) 33 (2.1%) 91% (95%
CI: 71, 97),
p<0.001 6 (0.7%) 45 (4.8%) 87% (95%
CI: 69, 94),
p<0.001
Number of Patients N = 2103N = 2119N = 1178N = 1179
Symptomatic VTE 5 (0.2%) 11 (0.5%) 3 (0.3%) 15 (1.3%)
?Includes the placebo-controlled period of RECORD 2
?Proximal DVT, nonfatal PE or VTE-related death
One randomized, double-blind, clinical study (RECORD 3) in patients undergoing elective total knee replacement surgery compared XARELTO 10 mg once daily started at least 6 to 8 hours (about 90% of patients dosed 6 to 10 hours) after wound closure versus enoxaparin. In RECORD 3, the enoxaparin regimen was 40 mg once daily started 12 hours preoperatively. The mean age (± SD) of patients in the study was 68 ± 9.0 (range 28 to 91) years with 66% of patients ≥65 years. Sixty-eight percent (68%) of patients were female. Eighty-one percent (81%) of patients were White, less than 7% were Asian, and less than 2% were Black. The study excluded patients with severe renal impairment defined as an estimated creatinine clearance <30 mL/min or patients with significant liver disease (hepatitis or cirrhosis). The mean exposure duration (± SD) to active XARELTO and enoxaparin was 11.9 ± 2.3 and 12.5 ± 3.0 days, respectively. The efficacy data are provided in Table 7.
Table 7: Summary of Key Efficacy Analysis Results for Patients Undergoing Total Knee Replacement Surgery- Modified Intent-to-Treat Population
RECORD 3
Treatment Dosage and Duration
XARELTO
10 mg once daily
Enoxaparin
40 mg once daily
RRR*,
p-value
Number of Patients N = 813N = 871
Total VTE 79 (9.7%) 164 (18.8%) 48% (95% CI: 34, 60), p<0.001 Components of events contributing to Total VTE
Proximal DVT 9 (1.1%) 19 (2.2%)
Distal DVT 74 (9.1%) 154 (17.7%)
Non-fatal PE 0 4 (0.5%)
Death (any cause) 0 2 (0.2%)
Number of Patients N = 895N = 917
Major VTE?9 (1.0%) 23 (2.5%) 60% (95% CI: 14, 81), p=0.024 Number of Patients N = 1206N = 1226
Symptomatic VTE8 (0.7%) 24 (2.0%)
?Proximal DVT, nonfatal PE or VTE-related death
16 HOW SUPPLIED/STORAGE AND HANDLING
XARELTO (rivaroxaban) 10 mg Tablets are round, light red, biconvex film-coated tablets marked with a triangle pointing down above a "10" on one side, and an "Xa" on the other side. The tablets are supplied in the packages listed:
NDC 50458-580-30 Bottle containing 30 tablets
NDC 50458-580-10 Blister package containing 100 tablets (10 blister cards containing 10 tablets each)
Store at 25° C (77° F) or room temperature; excursions permitted to 15°–30° C (59°–86° F) [see USP Controlled Room Temperature]. Keep out of the reach of children.
17 PATIENT COUNSELING INFORMATION
17.1 Instructions for Patient Use
?Advise patients to take XARELTO only as directed.
?Remind patients not to discontinue XARELTO prematurely without first talking to their healthcare professional.
?If a dose is missed, advise the patient to take XARELTO as soon as possible and continue on the following day with their once daily dose regimen.
17.2 Bleeding Risks
If patients have had neuraxial anesthesia or spinal puncture, and particularly, if they are taking concomitant NSAIDs or platelet inhibitors, advise patients to watch for signs and symptoms of spinal or epidural hematoma, such as tingling, numbness (especially
in the lower limbs) and muscular weakness. If any of these symptoms occur, advise the patient to contact his or her physician immediately.
Advise patients to report any unusual bleeding or bruising to their physician. Inform patients that it might take them longer than usual to stop bleeding, and that they may bruise and/or bleed more easily when they are treated with XARELTO [see Warnings and Precautions (5.2)].
17.3 Concomitant Medication and Herbals
Advise patients to inform their physicians and dentists if they are taking, or plan to take, any prescription or over-the-counter drugs or herbals, so their healthcare professionals can evaluate potential interactions [see Drug Interactions (7)].
17.4 Pregnancy and Pregnancy-Related Hemorrhage
Advise patients to inform their physician immediately if they become pregnant or intend to become pregnant during treatment with XARELTO [see Use in Specific Populations (8.1)].
Advise pregnant women receiving XARELTO to immediately report to their physician any bleeding or symptoms of blood loss [see Warnings and Precautions (5.3)].
17.5 Nursing
Advise patients to discuss with their physician if they are nursing or intend to nurse during anticoagulant treatment [see Use in Specific Populations (8.3)].
17.6 Females of Reproductive Potential
Advise patients who can become pregnant to discuss pregnancy planning with their physician [see Use in Specific Populations (8.6)]. Active Ingredient Made in Germany
Finished Product Manufactured by:
Janssen Ortho, LLC
Gurabo, PR 00778
Manufactured for:
Janssen Pharmaceuticals, Inc.
Titusville, NJ 08560
Licensed from:
Bayer HealthCare AG
51368 Leverkusen, Germany
? Janssen Pharmaceuticals, Inc. 2011
PRINCIPAL DISPLAY PANEL - 10 mg Tablet Bottle Label
NDC 50458-580-30
30 Tablets
Xarelto?
(rivaroxaban)
Tablets 10 mg Rx only janssen
度他雄胺软胶囊fda说明书
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use AVODART safely and effectively. See full prescribing information for AVODART. AVODART (dutasteride) Soft Gelatin Capsules Initial U.S. Approval: 2001 ---------------------------RECENT MAJOR CHANGES--------------------Warnings and Precautions, Evaluation for Other Urological 03/2012 Diseases (5.3) ----------------------------INDICATIONS AND USAGE---------------------AVODART is a 5 alpha-reductase inhibitor indicated for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to: (1.1) x improve symptoms, x reduce the risk of acute urinary retention, and x reduce the risk of the need for BPH-related surgery. AVODART in combination with the alpha adrenergic antagonist, tamsulosin, is indicated for the treatment of symptomatic BPH in men with an enlarged prostate. (1.2) Limitations of Use: AVODART is not approved for the prevention of prostate cancer. (1.3) -----------------------DOSAGE AND ADMINISTRATION ----------------Monotherapy: 0.5 mg once daily. (2.1) Combination with tamsulosin: 0.5 mg once daily and tamsulosin 0.4 mg once daily. (2.2) Dosing considerations: Swallow whole. May take with or without food. (2) ---------------------DOSAGE FORMS AND STRENGTHS -------------- 0.5-mg soft gelatin capsules (3) -------------------------------CONTRAINDICATIONS------------------------ x Pregnancy and women of childbearing potential. (4, 5.4, 8.1) x Pediatric patients. (4) FULL PRESCRIBING INFORMATION: CONTENTS* 1INDICATIONS AND USAGE 1.1Monotherapy 1.2Combination With Alpha Adrenergic Antagonist 1.3Limitations of Use 2DOSAGE AND ADMINISTRATION 2.1Monotherapy 2.2Combination With Alpha Adrenergic Antagonist 3DOSAGE FORMS AND STRENGTHS 4 C O NTRAINDICATI O NS 5WARNINGS AND PRECAUTIONS 5.1Effects on Prostate-Specific Antigen (PSA) and the Use of PSA in Prostate Cancer Detection 5.2Increased Risk of High-Grade Prostate Cancer 5.3Evaluation for Other Urological Diseases 5.4Exposure of Women—Risk to Male Fetus 5.5B lood Donation 5.6Effect on Semen Characteristics 6ADVERSE REACTIONS 6.1Clinical Trials Experience 6.2Postmarketing Experience 7DRUG INTERACTIONS 7.1Cytochrome P450 3A Inhibitors 7.2Alpha Adrenergic Antagonists 7.3Calcium Channel Antagonists 7.4Cholestyramine 7.5Digoxin 7.6Warfarin x Patients with previously demonstrated, clinically significant hypersensitivity (e.g., serious skin reactions, angioedema) to AVODART or other 5 alpha-reductase inhibitors. (4) -----------------------WARNINGS AND PRECAUTIONS ---------------- x AVODART reduces serum prostate-specific antigen (PSA) concentration by approximately 50%. However, any confirmed increase in PSA while on AVODART may signal the presence of prostate cancer and should be evaluated, even if those values are still within the normal range for untreated men. (5.1) x AVODART may increase the risk of high-grade prostate cancer. (5.2, 6.1) x Prior to initiating treatment with AVODART, consideration should be given to other urological conditions that may cause similar symptoms. (5.3) x Women who are pregnant or could become pregnant should not handle AVODART Capsules due to potential risk to a male fetus. (5.4, 8.1) x Patients should not donate blood until 6 months after their last dose of AVODART. (5.5) ------------------------------ADVERSE REACTIONS ----------------------- The most common adverse reactions, reported in t1% of subjects treated with AVODART and more commonly than in subjects treated with placebo, are impotence, decreased libido, ejaculation disorders, and breast disorders. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or https://www.360docs.net/doc/ce5398495.html,/medwatch. -------------------------------DRUG INTERACTIONS------------------------ Use with caution in patients taking potent, chronic CYP3A4 enzyme inhibitors (e.g., ritonavir). (7) See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 10/2012 8USE IN SPECIFIC POPULATIONS 8.1Pregnancy 8.3Nursing Mothers 8.4Pediatric Use 8.5Geriatric Use 8.6Renal Impairment 8.7Hepatic Impairment 10OVERDOSAGE 11DESCRIPTION 12CLINICAL PHARMACOLOGY 12.1Mechanism of Action 12.2Pharmacodynamics 12.3Pharmacokinetics 13NONCLINICAL TOXICOLOGY 13.1Carcinogenesis, Mutagenesis, Impairment of Fertility 13.2Animal Toxicology and/or Pharmacology 14CLINICAL STUDIES 14.1Monotherapy 14.2Combination With Alpha-Blocker Therapy (CombAT) 16HOW SUPPLIED/STORAGE AND HANDLING 17PATIENT COUNSELING INFORMATION 17.1PSA Monitoring 17.2Increased Risk of High-Grade Prostate Cancer 17.3Exposure of Women—Risk to Male Fetus 17.4Blood Donation *Sections or subsections omitted from the full prescribing information are not listed.
FDA 行业指南 中英对照 待完成
Guidance for Industry Container Closure Systems for Packaging Human Drugs and Biologics Chemistry, Manufacturing and Controls Documentation 行业指南 人用药品及生物制品的包装容器和封装系统:化学,生产和控制文件 指南发布者:美国FDA下属的CDER及CBER 发布日期:May 1999 TABLE OF CONTENTS目录 I. INTRODUCTION介绍 II. BACKGROUND 背景 A. Definitions 定义 B. CGMP, CPSC and USP Requirements on Containers and Closures. CGMP, CPSC和 USP对容器和密封的要求 C. Additional Considerations 其他需要考虑的事项 III. QUALIFICATION AND QUALITY CONTROL OF PACKAGING COMPONENTS包装组件的合格要求以及质量控制 A. Introduction 介绍 B. General Considerations 通常要求 C. Information That Should Be Submitted in Support of an Original Application for Any Drug Product 为支持任何药品的原始申请所必须提供的信息 D. Inhalation Drug Products 吸入性药品 E. Drug Products for Injection and Ophthalmic Drug Products 注射剂和眼科用药 F. Liquid-Based Oral and Topical Drug Products and Topical Delivery Systems 液体口服 和外用药品和外用给药系统 G. Solid Oral Dosage Forms and Powders for Reconstitution 口服固体剂型和待重新溶解 的粉末 H. Other Dosage Forms 其他剂型 IV. POSTAPPROVAL PACKAGING CHANGES 批准后的包装变更 V. TYPE III DRUG MASTER FILES 药品主文件第III类 A. General Comments 总体评述 B. Information in a Type III DMF 第III类DMF中包括的信息 VI. BULK CONTAINERS 大包装容器 A. Containers for Bulk Drug Substances 用于原料药的容器 B. Containers for Bulk Drug Products 用于散装药品的容器 ATTACHMENT A 附件A REGULATORY REQUIREMENTS 药政要求
美国FDA批准药品Afinitor(everolimus,依维莫司)使用说明书
Afinitor(everolimus,依维莫司) FDA批准药品使用说明书 2016年3月份修订版 提供者:haoeyou(好医友)
FDA批准的抗癌药Anifitor,通用名为依维莫司。依维莫司是一种口服的雷帕霉素(mTOR)抑制剂,是西罗莫司(sirolimus,又称雷帕霉素,即rapamycin)的衍生物,故依维莫司又称40-O-(2-羟乙基)-雷帕霉素,或40-O-(2-羟乙基)-西罗莫司。近日,美国监管方面传来喜讯,Afinitor的新适应症,用于起源于胃肠道(gastrointestinal,GI)或肺部(lung)的不可切除性、局部晚期或转移性、进展性、分化良好的非功能性神经内分泌肿瘤(neuroendocrine tumor,NET)成人患者的治疗。 【用法用量】 (1)晚期肾细胞癌 每天一次,每次口服10mg,与食物同服或不同服皆可。中度肝功能损害患者,减量服用本品,每天一次,每次口服5mg。如需同时服用中度CYP3A4抑制剂或P糖蛋白抑制剂(如红霉素、氟康唑、维拉帕米),减量服用本品,每天一次,每次口服2.5mg,如果患者能耐受,剂量可增至每次口服5mg。如需同时服用CYP3A4强诱导剂(如利福平、苯妥英),增量服用本品,每次增加5mg,最大使用剂量可达每天一次,每次20mg。 (2)室管膜下巨细胞星形细胞瘤(SEGA) 初始剂量随着患者体表面积(BSA)的不同而不同(BSA 0.5 m2 ~1.2 m2,初始剂量2.5 mg/天;BSA 1.3 m2 ~ 2.1 m2,5mg/天;BSA≥2.2 m2,7.5 mg/天),随后滴定剂量使血药谷浓度达到5-10 ng/mL。 如需同时服用中度CYP3A4抑制剂或P糖蛋白抑制剂,大约减量50%服用本品。随后的剂量需根据血药浓度监测结果(TDM,therapeutic drug monitoring)来调整。 如需同时服用CYP3A4强诱导剂,加倍增量服用本品。随后的剂量需根据血药浓度监测结果(TDM)来调整。处理药物不良反应时,可能需要减量服用本品,或中断本品治疗。 【禁忌症】 禁用于对本品、其它雷帕霉素衍生物或任何辅料过敏的患者。 【注意事项】 (1)非-感染性肺炎:监测临床症状或影象学改变; 曾发生致命性病例。减低本品剂量或停用本品直至症状缓解,可考虑使用皮质甾体激素。 (2)感染:本品可增加感染风险, 可能致命。监测体征和症状,及时治疗。 (3)口腔溃疡:口腔溃烂, 口内炎和口粘膜炎很常见。处理包括口腔冲洗(无酒精或过氧化物)和局部治疗。
FDA指南中文版
目录表 I. 导言 (1) II. 背景 (2) III. 分析方法的类型 (3) A. 法定分析方法 (3) B. 可选择分析方法 (3) 3 C. 稳定性指示分析 (3) IV. 对照品 (4) A. 对照品的类型 (4) B. 分析报告单 (4) C. 对照品的界定 (4) V. IND中的分析方法验证 (6) VI. NDA, ANDA, BLA 和PLA中分析方法验证的内容和格式 (6) A. 原则 (6) B. 取样 (7) C. 仪器和仪器参数 (7) D. 试剂 (7) E. 系统适应性实验 (7) F. 对照品的制备 (7) G. 样品的制备 (8) H. 分析方法 (8) L. 计算 (8) J. 结果报告 (8) VII. NDA,ANDA,BLA和PLA中的分析方法验证 (9) A. 非法定分析方法 (9) 1.验证项目 (9) 2. 其它分析方法验证信息 (10) a. 耐用性 (11)
b. 强降解实验 (11) c. 仪器输出/原始资料 (11) 3.各类检测的建议验证项目 (13) B. 法定分析方法 (15) VIII. 统计分析 (15) A. 总则 (15) B. 比较研究 (16) C. 统计 (16) IX. 再验证 (16) X. 分析方法验证技术包:内容和过程 (17) A. 分析方法验证技术包 (17) B. 样品的选择和运输 (18) C. 各方责任 (19) XI. 方法 (20) A. 高效液相色谱(HPLC) (20) B. 气相色谱(GC) (22) C. 分光光度法,光谱学,光谱法和相关的物理方法 (23) D. 毛细管电泳 (23) E. 旋光度 (24) F. 粒径相关的分析方法 (25) G. 溶出度 (26) H. 其它仪器分析方法 (27) 附件 A:NDA,ANDA,BLA和PLA申请的内容 (28) 附件 B:分析方法验证的问题和延误 (29) 参考文献 (30) 术语表 (32) I. INTRODUCTION This guidance provides recommendations to applicants on submitting analytical
美国FDA指南 中文版
《美国FDA认证与申办指南》权威资讯系列 《合成原料药DMF起草大纲》
使用说明: 1、本大纲是为了帮助我公司客户把握DMF的整体内容而准备的, 由于DMF内容繁多,从整体上了解内容框架和组成部分,对于理解FDA对DMF的要求和意图非常有必要; 2、根据FDA的要求,凡是本大纲提到的内容,原料药制造商均应 该提供。因此,客户务必依照规定提供尽可能详细的内容。 3、本大纲的内容和相关要求能够确保客户目前的运作达到FDA的cGMP标准,因此,准备DMF的过程,也使客户按照FDA的要求进 行整改和提高的过程,这些都为FDA未来的现场检查打下良好基础;4、凡是本大纲中提到的非技术性具体内容要求,请参照本公司专有的与此大纲配套的相关DFM指导性文件,包括《FDA药物主文件指南》、《关于在药品递交中递交的有关原料药生产的支持文件的指南》、《药物申办中质量管理方面通用技术文件格式与内容要求》; 5、凡是本大纲中提到的技术性具体内容要求,如杂质、稳定性、验证等具体技术要求,请参照本公司专有的FDA相关技术标准文件, 包括《原料药认证指南》、《制剂认证指南》、《化学药物稳定性指南》、《化学药物杂质指南》、《化学药物化验与合格参数指南》、《化学药物验证指南》等;
《合成原料药DMF起草大纲》 一、公司和生产场地的基本描述 1、第一类的DMF文件建议由位于美国之外的人提供,以帮助FDA对他们的生产设施进行现场检查。DMF文件应描述生产场地、设备能力、生产流程图等。A Type I DMF is recommended for a person outside of the United States to assist FDA in conducting on site inspections of their manufacturing facilities. The DMF should describe the manufacturing site, equipment capabilities, and operational layout. 2、第一类的DMF文件对美国国内设施通常不需要,除非该设施没有登记并定期接受检查。A Type I DMF is normally not needed to describe domestic facilities, except in special cases, such as when a person is not registered and not routinely inspected. 3、场地的描述应包括面积、实际地址以及表明该场地与最近的城市的距离的地图。提供该场地的鸟瞰图和平面图。The description of the site should include acreage, actual site address, and a map showing its location with respect to the nearest city. An aerial photograph and a diagram of the site may be helpful. 4、主要生产和加工区域的平面图对于理解整个生产布局会有帮助。应当描述主要设备的生产能力、用途和位置。通常不用描述设备的制造商和型号,除非特别新或独特的设备。A diagram of major production and processing areas is helpful for understanding the operational layout. Major equipment should be described in terms of capabilities, application, and location. Make and model would not normally be needed unless the equipment is new or unique. 5、公司主要的组成部门结构图,包括总公司和生产场地的关键生产、质量控制、质量保证岗位,A diagram of major corporate organizational elements, with key manufacturing, quality control, and quality assurance positions highlighted, at both the manufacturing site and corporate headquarters, is also helpful. 二、原料药的物理和化学特征 1、特性Properties 相关法规要求对原料药的物理和化学特征做出详细描述。该要求可以通过提供下
美国FDA指南-中文版
《美国FDA认证与申办指南》 权威资讯系列 《合成原料药DMF起草大纲》
使用说明: 1、本大纲是为了帮助我公司客户把握DMF的整体内容而准备 的,由于DMF内容繁多,从整体上了解内容框架和组成部分,对于理解FDA对DMF的要求和意图非常有必要; 2、根据FDA的要求,凡是本大纲提到的内容,原料药制造商均 应该提供。因此,客户务必依照规定提供尽可能详细的内容。3、本大纲的内容和相关要求能够确保客户目前的运作达到FDA 的cGMP标准,因此,准备DMF的过程,也使客户按照FDA的要求进行整改和提高的过程,这些都为FDA未来的现场检查打下良好基础; 4、凡是本大纲中提到的非技术性具体内容要求,请参照本公司专有的与此大纲配套的相关DFM指导性文件,包括《FDA药物主文件指南》、《关于在药品递交中递交的有关原料药生产的支持文件的指南》、《药物申办中质量管理方面通用技术文件格式与内容要求》; 5、凡是本大纲中提到的技术性具体内容要求,如杂质、稳定性、验证等具体技术要求,请参照本公司专有的FDA相关技术标准文件,包括《原料药认证指南》、《制剂认证指南》、《化学药物稳定性指南》、《化学药物杂质指南》、《化学药物化验与合格参数指南》、《化学药物验证指南》等;
《合成原料药DMF起草大纲》 一、公司和生产场地的基本描述 1、第一类的DMF文件建议由位于美国之外的人提供,以帮助FDA对他们的生产设施进行现场检查。DMF文件应描述生产场地、设备能力、生产流程图等。A Type I DMF is recommended for a person outside of the United States to assist FDA in conducting on site inspections of their manufacturing facilities. The DMF should describe the manufacturing site, equipment capabilities, and operational layout. 2、第一类的DMF文件对美国国内设施通常不需要,除非该设施没有登记并定期接受检查。A Type I DMF is normally not needed to describe domestic facilities, except in special cases, such as when a person is not registered and not routinely inspected. 3、场地的描述应包括面积、实际地址以及表明该场地与最近的城市的距离的地图。提供该场地的鸟瞰图和平面图。The description of the site should include acreage, actual site address, and a map showing its location with respect to the nearest city. An aerial photograph and a diagram of the site may be helpful. 4、主要生产和加工区域的平面图对于理解整个生产布局会有帮助。应当描述主要设备的生产能力、用途和位置。通常不用描述设备的制造商和型号,除非特别新或独特的设备。A diagram of major production and processing areas is helpful for understanding the operational layout. Major equipment should be described in terms of capabilities, application, and location. Make and model would not normally be needed unless the equipment is new or unique. 5、公司主要的组成部门结构图,包括总公司和生产场地的关键生产、质量控制、质量保证岗位,A diagram of major corporate organizational elements, with key manufacturing, quality control, and quality assurance positions highlighted, at both the manufacturing site and corporate headquarters, is also helpful.
FDA批准药品Nelarabine最新使用说明书
奈拉滨(Nelarabine)是用于治疗至少两种治疗方案无效或治疗后复发的T细胞急性淋巴细胞性白血病(T-ALL)和T细胞淋巴母细胞性淋巴瘤(T-LBL)。 中文名称:奈拉滨 中文别名:奈拉滨及其中间体(研发);奈拉滨及其中间体;奈拉宾;9beta-D-阿拉伯呋喃糖-6-甲氧基-9H-嘌呤-2-胺;9-beta-D-阿拉伯呋喃糖-6-甲氧基-9H-嘌呤-2-胺 英文名称:Nelzarabine 英文别名:NELARABINE; Nelzarabine [USAN]; 9-beta-D-Arabinofuranosyl-6-methoxy-9H-purin-2-amine; 9-(D-arabinofuranosyl)-6-methoxy-9H-purin-2-amine CAS:121032-29-9 分子式:C11H15N5O5 分子量:297.2673 原研企业:GSK 适应症:用于治疗至少对两种以上化疗方案无应答或复发的急性T一细胞淋巴母细胞性白血病(T—ALL)T一细胞淋巴母细胞性淋巴瘤(T—LBL)患者。 用法用量: 成年人:采用静脉滴注给药,推荐剂量为1500mg·m-2·d-1,5天隔日给药,2l天为一周期。 儿童:采用静脉滴注给药,推荐剂量为650mg·m-2·d-1,连续5天,21 天为一周期。 作用机制 奈拉滨在腺苷脱氨酶作用下,去甲基转化成ara—G,在脱氧鸟苷激酶和脱氧苷激酶作用下单磷酸化,接着转化为活性5-三磷酸盐ara-GTP。Ara-GTP在白血病胚细胞中蓄积到一定程度后嵌合入DNA中,从而抑制DNA的合成,最终导致细胞死亡。此外,BeesleyAH等人研究发现,T细胞对奈拉滨的敏感度是B细胞的8倍。E1ineJ等人研究表明,ara—GTP在T细胞内比在B细胞内的累积速度更快,累积量更多,ara—GTP对T细胞有更强的选择性细胞毒作用。 药代 BergSL等人对T-ALL和T-LBL患者奈拉滨药代动力学研究表明,药物及其活性代谢物ara—G 能迅速分布到血浆中。奈拉滨及其活性代谢物ara—G半衰期分为l5分钟和3小时。成人和儿童体内,奈拉滨表观分布容积分别为(197±216)L/m。和(213±358)L/m。,ara—G表观分布容积分别为(50+24)L/m。以及(33--+9.3)L/m。注射1500mg/m2奈拉滨两小时后成年患者体内的奈拉滨和ara—G的平均血浆浓度值分别为(5.0-+3.0)ug/mL和(31.4-+5.6)ug/mL。静脉滴注奈拉滨104~2900mm。后,成人和儿童表观平均清除值分别为(197-+189)L·h-1·m-2和(259±409)L·h-1·m-2,儿童较成年人高30%。成人和儿童体内ara—G平均清除值大致与奈拉宾相等,分别为(197±189)L·h-1·m-2和(259±409)L·h-1·m-2 奈拉滨的主要代谢途径是,在腺苷脱氨酶的作用下,脱甲基生成ara-G,进一步水解形成鸟嘌呤,最后脱甲基生成尿酸。部分奈拉滨直接水鸟嘌吟’然后胛基生成尿酸。 奈拉滨和ara—G在肾脏部分消除,分别以原药形式从尿中排泄(6.6-+4.7)%和(27±l5)%。规定给药剂量下(650mg·m-2·d-1),28位成年患者注射给药24小时后测得奈拉滨和araG的肾清除率平均值为(24±23)L/h和(6.2±5.0)L/h。 临床试验 FDA发布一份奈拉滨临床研究报告,将参与试验的患者分为儿童组和成年组。采用静脉滴注给药,儿童组剂量为650 mg·m-2·d-1连续5天。成人组为在第一,三和五天1500 mg·m-2·d-1。
左乙拉西坦注射液FDA说明书
Zemplar? (paricalcitol injection) Fliptop Vial DESCRIPTION Zemplar? (paricalcitol injection) is a synthetically manufactured vitamin D analog. It is available as a sterile, clear, colorless, aqueous solution for intravenous injection. Each mL contains paricalcitol, 5 mcg; propylene glycol, 30% (v/v); and alcohol, 20% (v/v). Paricalcitol is a white powder chemically designated as 19-nor-1a,3?,25-trihydroxy-9,10-secoergosta-5(Z),7(E),22(E)-triene and has the following structural formula: Molecular weight is 416.65. CLINICAL PHARMACOLOGY Mechanism of Action Paricalcitol is a synthetic vitamin D analog. Vitamin D and paricalcitol have been shown to reduce parathyroid hormone (PTH) levels. Pharmacokinetics Distribution The pharmacokinetics of paricalcitol have been studied in patients with chronic renal failure (CRF) requiring hemodialysis.Zemplar? is administered as an intravenous bolus injection. Within two hours after administering doses ranging from 0.04 to 0.24 mcg/kg, concentrations of paricalcitol decreased rapidly; thereafter, concentrations of paricalcitol declined log-linearly with a mean half-life of about 15 hours. No accumulation of paricalcitol was observed with multiple dosing. Elimination In healthy subjects, plasma radioactivity after a single 0.16 mcg/kg intravenous bolus dose of3H-paricalcitol (n=4) was attributed to parent drug. Paricalcitol was eliminated primarily by hepatobiliary excretion, as 74% of the radioactive dose was recovered in feces and only 16%was found in urine. Metabolism Several unknown metabolites were detected in both the urine and feces, with no detectable paricalcitol in the urine. These metabolites have not been characterized and have not been identified. Together, these metabolites contributed 51% of the urinary radioactivity and 59%
FDA英文药品说明书规定项目中英对照
FDA英文药品说明书规定项目中英对照 -------------------------------------------------------------------------------- 药品说明书旧称description,instruction,direction.今称insert,package insert 美国FDA规定其应包括十项。 一.drug names(药物名称) 1.通常每种药物有三个名字 (1)proprietary name(商品名称) (2)popular name(俗名) (3)chemical name(化学名) 2.说明书标题多用商品名 其右上角标有R者,表示registered trademark(注册商标) 二.description(性状)(常用description,introduction,composition) 包括药品的chemical structure(化学结构)、chemical composition(化学成分)、physical and chemical properties(物理和化学性质) 三.clinical pharmacology(临床药理学) 常用的还有: clinical data(临床数据)、clinical experience(临床经验)、clinical use(临床应用)、clinical observation(临床观察)、clinical effect(临床疗效)、clinical discussion(临床讨论)、mode of mechanism of action(临床机理及途径)、pharmacological actions(药理作用)、therapeutical actions(治疗作用)、bacteriology(细菌学)、microbiology(微生物学)、physiology(生理学)、toxicology(毒理学) 四.indications and usage(适应证和用法) 常用标题:indications,major indications,clinical indications,principal indications,condications,uses,treatment 五.contraindications(禁忌证) 1.常用标题 contraindications,restriction on use(限制使用) 2.常用词(组) pregnant women孕妇 women of childbeating age育龄妇女 be hypersensitive to 对......过敏者
美国FDA网站使用方法
美国食品和药品管理局FDA药学信息资源 美国食品和药品管理局FDA (Food and Drug Administration)是 一个美国政府监督美国国内食品、药品、化妆品、放射物、医疗器械等是否安全、有效、可信的主管部门。FDA网站[1]即是由FDA在Internet上建立的,向公众开放的信息发布站点。本文介绍该站的结构并主要考察其中的药学信息资源。 1. FDA主页结构 经分析,该主页可分4个区:功能区、职责区、专业区、提示区。实际是4个主索引,便于访客浏览。各区相互间有大部分是交叉的。现分别介绍如下。 1.1 功能区这是一般网站主页(包括个人和商业网站主页)最常用的 结构,有7个栏目。 1.1.1 更新情况(what’s new) 提供新增内容和近期修改,主要向FDA 网站的经常访问者服务。 1.1.2 网址目录Index(FDA Web Site Index) 系FDA下级目录的主题,按字母顺序排列。如“关于FDA”(about FDA)、缩写(Acronyms and Abbreviations)、副作用(Adverse Reactions)、顾问团(Advisory Committees)、爱滋病(AIDS)、老化(Aging)、年鉴(Almanac)等等。粗略浏览可以对网站总貌有个大致了解。点击标题(如Aging)即可进入相关内容。 1.1.3 搜索Search(FAD Search) 有助于快速找到网站内所需信息。以阿昔洛韦为例,键入Acyclovir,搜索范围“Search All of FDA”,可以从该网站庞大的47370篇文献中找到127篇相匹配。搜索结果分别列出了这些文献的概述(Summary)和入口,入口为蓝色的URL地址(http://......),点击后可进入正文。如果只关心Acyclovir在FDA新药审评中的情况,可以确定搜索范围在药品审评和研究中心(Center for Drug Evaluation and Research,CDER),则匹配文献减至71篇。 1.1.4 高频问题FAQS(Frequently Asked Questions) 以问答式列出一 些常见问题。分为4大类:动物药、化妆品、食品、FDA一般问题。以“FDA一般问题”为例有,FDA作用?组成?处理不良反应方式?等等。
如何使用FDA
网上FDA及其药学信息资源 FDA(Food and Drug Administration,美国食品和药品管理局)是一个美国政府监督美国国内食品、药品、化妆品、放射物、医疗器械等是否安全、有效、可信的主管部门。FDA网站[1]即是由FDA在Internet 上建立的,向公众开放的信息发布站点。本文介绍该站的结构并主要考察其中的药学信息资源。 1. FDA主页结构 经分析,该主页可分4个区:功能区、职责区、专业区、提示区。实际是4个主索引,便于访客浏览。各区相互间有大部分是交叉的。现分别介绍如下。 1.1 功能区这是一般网站主页(包括个人和商业网站主页)最常用的结构,有7个栏目。 1.1.1 更新情况(what‘s new)提供新增内容和近期修改,主要向FDA网站的经常访问者服务。 1.1.2 网址目录Index(FDA Web Site Index)系FDA下级目录的主题,按字母顺序排列。如“关于FDA”(about FDA)、缩写(Acronyms and Abbreviations)、副作用(Adverse Reactions)、顾问团(Advisory Committees)、爱滋病(AIDS)、老化(Aging)、年鉴(Almanac)等等。粗略浏览可以对网站总貌有个大致了解。点击标题(如Aging)即可进入相关内容。 1.1.3 搜索Search(FAD Search)有助于快速找到网站内所需信息。以阿昔洛韦为例,键入Acyclovir,搜索范围“Search All of FDA”,可以从该网站庞大的47370篇文献中找到127篇相匹配。搜索结果分别列出了这些文献的概述(Summary)和入口,入口为蓝色的URL地址(http://……),点击后可进入正文。如果只关心Acyclovir在FDA新药审评中的情况,可以确定搜索范围在药品审评和研究中心(Center for Drug Evaluation and Research,CDER),则匹配文献减至71篇。 1.1.4 高频问题FAQS(Frequently Asked Questions)以问答式列出一些常见问题。分为4大类:动物药、化妆品、食品、FDA一般问题。以“FDA一般问题”为例有,FDA作用?组成?处理不良反应方式?等等。 1.1.5 记事本(Dockets)相当于FDA的档案室,包括重要事件、会议记录、日程流水帐。笔者认为较主要的有2个部分,其一是会议记录公开(点击 FDA Advisory Committees);其二是联邦注册档案(FDA Federal Register Documents)。所谓会议记录公开,系FDA各顾问团的公开会议记录。为了体现新药审评中的公开、公正,各顾问团的部分会议讲话被记录在案,上网公布。不过这些会议记录动辄三百多页,是名符其实的文山会海。如果你只关心会上专家们是怎样谈到Acyclovir的,则需用搜索(见1.1.3)来缩小范围。键入Acyclovir后,将搜索范围限于“Dockets”,则可以从12233篇Dockets文献中查到29篇相匹配,仔细浏览概述(Summy),找到会议记录,点击入口,即可知道Mr.XX是如何评价Acyclovir了。查Acyclovir的联邦注册档案可同上操作。在网上可以看到Acyclovir的审批资料原文(图片形式),甚至FDA官员们在Acyclovir审批资料上潦草的鉴名。 1.1.6 外语版和国际信息International(Foreign Language and Interational Information)涉及一些FDA法规的外语版和FDA的国际间协议和活动。其中,FDA法规中文版的信息不多,主要讲食品和化妆品进口。有志于将药品打入美国市场的医药公司,可以重点研究“国际信息栏”中“人用药品”(Human Pharmaceutical Products:International Activities),其法律条文是最新的。
