2013年国际头痛新分类和诊断标准
头痛的国际分类(第三版)中文
The international Classification of Headache disorders, 3rd Editon2.1.2 Infrequent episodic tension-type headache not associated with pericranial tenderness2.2.1 Frequent episodic tension-type headache associated with pericranial tenderness2.2.2 Frequent episodic tension-type headache not associated with pericranial tenderness2.3.2 Chronic tension-type headache not associated with pericranial tenderness3.3.1 Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) 3.3.1.1 Episodic SUNCT3.3.1.2 Chronic SUNCT3.3.2 Short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA)3.3.2.1 Episodic SUNA3.3.2.2 Chronic SUNA3.4 Hemicrania continua3.5 Probable trigeminal autonomic cephalalgia3.5.1 Probable cluster headache3.5.2 Probable paroxysmal hemicrania3.5.3 Probable short-lasting unilateral neuralgiform headache attacks3.5.4 Probable hemicrania continua4.其它的原发性头痛Other primary headache disorders )4.1 Primary cough headache原发性咳嗽头痛4.1.1 Probable primary cough headache4.2 Primary exercise headache原发性运动性头痛4.2.1 Probable primary exercise headache4.3 Primary headache associated with sexual activity原发性性活动伴随的头痛4.3.1 Probable primary headache associated with sexual activity4.4 Primary thunderclap headache原发性霹雳头痛4.5 Cold-stimulus headache冷刺激性头痛4.5.1 Headache attributed to external application of a cold stimulus4.5.2 Headache attributed to ingestion or inhalation of a cold stimulus4.5.3 Probable cold-stimulus headache4.5.3.1 Headache probably attributed to external application of a cold stimulus4.5.3.2 Headache probably attributed to ingestion or inhalation of a cold stimulus则可两者均可作为诊断4.10 New daily persistent headache (NDPH) 新症每日持续性头痛4.10.1 Probable new daily persistent headach二、继发性头痛(the secondary headaches)5.缘于头、颈部外伤的头痛(Headache attributed to trauma or injury to the head and/or neck)5.1 Acute headache attributed to traumatic injury to the head5.1.1 Acute headache attributed to moderate or severe traumatic injury to the head5.1.2 Acute headache attributed to mild traumatic injury to the head5.2 Persistent headache attributed to traumatic injury to the head5.2.1 Persistent headache attributed to moderate or severe traumatic injury to the head5.2.2 Persistent headache attributed to mild traumatic injury to the head5.3 Acute headache attributed to whiplash5.4 Persistent headache attributed to whiplash5.5 Acute headache attributed to craniotomy5.6 Persistent headache attributed to craniotomy6.缘于头颈部血管疾病的头痛(Headache attributed to cranial or cervical vascular disorder )6.1 Headache attributed to ischaemic stroke or transient ischaemic attack6.1.1 Headache attributed to ischaemic stroke (cerebral infarction)6.1.2 Headache attributed to transient ischaemic attack (TIA)6.2 Headache attributed to non-traumatic intracranial haemorrhage6.2.1 Headache attributed to non-traumatic intracerebral haemorrhage非外伤性脑出血6.2.2 Headache attributed to non-traumatic subarachnoid haemorrhage (SAH)6.2.3 Headache attributed to non-traumatic acute subdural haemorrhage (ASDH)急性硬膜下血肿6.3 Headache attributed to unruptured vascular malformation未破裂的血管畸形6.3.1 Headache attributed to unruptured saccular aneurysm囊性动脉瘤6.3.2 Headache attributed to arteriovenous malformation (AVM) 动静脉畸形6.3.3 Headache attributed to dural arteriovenous fistula (DAVF) 硬膜动静脉瘘6.3.4 Headache attributed to cavernous angioma 海绵窦血管瘤6.3.5 Headache attributed to encephalotrigeminal or leptomeningeal angiomatosis (Sturge Weber syndrome)脑三叉神经或软脑膜血管瘤病6.4 Headache attributed to arteritis6.4.1 Headache attributed to giant cell arteritis (GCA) 颞动脉炎6.4.2 Headache attributed to primary angiitis of the central nervous system (PACNS)6.4.3 Headache attributed to secondary angiitis of the central nervous system (SACNS)6.7.1 Headache attributed to an intracranial endovascular procedure6.7.2 Angiography headache6.7.3 Headache attributed to reversible cerebral vasoconstriction syndrome (RCVS)6.7.3.1 Headache probably attributed to reversible cerebral vasoconstrictionsyndrome (RCVS)6.7.4 Headache attributed to intracranial arterial dissection颅内动脉夹层6.8 Headache attributed to genetic vasculopathy6.8.1 Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL)6.8.2 Mitochondrial Encephalopathy, Lactic Acidosis and Stroke-like episodes (MELAS)6.8.3 Headache attributed to another genetic vasculopathy6.9 Headache attributed to pituitary apoplexy垂体卒中7.缘于非血管性颅内疾病的头痛(Headache attributed to non-vascular intracranial disorder )7.1 Headache attributed to increased cerebrospinal fluid pressure颅内压增高7.1.1 Headache attributed to idiopathic intracranial hypertension (IIH)7.1.2 Headache attributed to intracranial hypertension secondary to metabolic, toxic or hormonal causes7.1.3 Headache attributed to intracranial hypertension secondary to hydrocephalus7.2 Headache attributed to low cerebrospinal fluid pressure颅内压低下7.2.1 Post-dural puncture headache腰穿后7.2.2 CSF fistula headache脑脊液漏7.2.3 Headache attributed to spontaneous intracranial hypotension自发性低颅压7.3 Headache attributed to non-infectious inflammatory disease非感染性炎性疾病7.3.1 Headache attributed to neurosarcoidosis7.3.2 Headache attributed to aseptic (non-infectious) meningitis7.3.3 Headache attributed to other non-infectious inflammatory disease7.3.4 Headache attributed to lymphocytic hypophysitis7.3.5 Syndrome of transient Headache and Neurological Deficits with cerebrospinal fluid Lymphocytosis (HaNDL)7.4 Headache attributed to intracranial neoplasia颅内新生物7.4.1 Headache attributed to intracranial neoplasm7.4.1.1 Headache attributed to colloid cyst of the third ventricle7.4.2 Headache attributed to carcinomatous meningitis癌性脑膜炎7.4.3 Headache attributed to hypothalamic or pituitary hyper- or hyposecretion7.5 Headache attributed to intrathecal injection鞘内注射7.6 Headache attributed to epileptic seizure7.6.1 Hemicrania epileptica癫痫半颅痛7.6.2 Post-ictal headache癫痫发作后头痛7.7 Headache attributed to Chiari malformation type I (CM1)7.8 Headache attributed to other non-vascular intracranial disorder8.缘于物质或物质戒断的头痛(Headache attributed to a substance or its withdrawal)8.1 Headache attributed to use of or exposure to a substance or its withdrawal缘于某种物质的应用或戒断8.1.1.2 Delayed NO donor-induced headache8.1.2 Phosphodiesterase (PDE) inhibitor-induced headache磷酸二酯酶抑制剂8.1.3 Carbon monoxide (CO)-induced headache一氧化碳诱发8.1.4 Alcohol-induced headache酒精诱发8.1.4.1 Immediate alcohol-induced headache8.1.4.2 Delayed alcohol-induced headache8.1.5 Headache induced by food and/or additive由于食物成分/添加剂诱发8.1.5.1 Monosodium glutamate (MSG)-induced headache谷氨酸单钠盐(味精)8.1.6 Cocaine-induced headache可卡因诱发8.1.7 Histamine-induced headache组织胺诱发8.1.7.1 Immediate histamine-induced headache8.1.7.2 Delayed histamine-induced headache8.1.8 Calcitonin gene-related peptide (CGRP)-induced headache降钙素基因相关多肽诱发8.1.8.1 Immediate CGRP-induced headache8.1.8.2 Delayed CGRP-induced headache8.1.9 Headache attributed to exogenous acute pressor agent8.1.10 Headache attributed to occasional use of non-headache medication8.1.11 Headache attributed to long-term use of non-headache medication8.1.12 Headache attributed to exogenous hormone8.1.13 Headache attributed to use of or exposure to other substance8.2.4 Opioid-overuse headache鸦片类8.2.5 Combination-analgesic-overuse headache复合制剂过度应用8.2.6 Medication-overuse headache attributed to multiple drug classes not individually over used联合用药所致8.2.7 Medication-overuse headache attributed to unverified overuse of multiple drug classes8.2.8 Medication-overuse headache attributed to other medication8.3 Headache attributed to substance withdrawal物质戒断8.3.1 Caffeine-withdrawal headache咖啡因8.3.2 Opioid-withdrawal headache鸦片类8.3.3 Oestrogen-withdrawal headache雌激素8.3.4 Headache attributed to withdrawal from chronic use of other substance9.缘于感染的头痛(Headache attributed to infection)9.1 Headache attributed to intracranial infection颅内感染9.1.1 Headache attributed to bacterial meningitis or meningoencephalitis细菌性脑膜炎/脑膜脑炎9.1.1.1 Acute headache attributed to bacterial meningitis or meningoencephalitis9.1.1.2 Chronic headache attributed to bacterial meningitis or meningoencephalitis9.1.1.3 Persistent headache attributed to past bacterial meningitis or meningoencephalitis9.1.2 Headache attributed to viral meningitis or encephalitis病毒性脑膜炎或脑炎9.1.2.1 Headache attributed to viral meningitis9.1.2.2 Headache attributed to viral encephalitis9.1.3 Headache attributed to intracranial fungal or other parasitic infection真菌或寄生虫感染9.1.3.1 Acute headache attributed to intracranial fungal or other parasitic infection9.1.3.2 Chronic headache attributed to intracranial fungal or other parasitic infection9.1.4 Headache attributed to brain abscess脑脓肿9.1.5 Headache attributed to subdural empyema硬膜下积脓9.2 Headache attributed to systemic infection系统感染9.2.1 Headache attributed to systemic bacterial infection系统细菌感染9.2.1.1 Acute headache attributed to systemic bacterial infection9.2.1.2 Chronic headache attributed to systemic bacterial infection9.2.2 Headache attributed to systemic viral infection系统病毒感染9.2.2.1 Acute headache attributed to systemic viral infection9.2.2.2 Chronic headache attributed to systemic viral infection9.2.3 Headache attributed to other systemic infection其他系统感染9.2.3.1 Acute headache attributed to other systemic infection9.2.3.2 Chronic headache attributed to other systemic infection10.缘于内环境紊乱的头痛(Headache attributed to disorder of homoeostasis)10.1 Headache attributed to hypoxia and/or hypercapnia缺氧和/或高碳酸血症10.1.1 High-altitude headache高海拔头痛10.1.2 Headache attributed to aeroplane travel飞行头痛10.1.3 Diving headache潜水头痛10.1.4 Sleep apnoea headache睡眠呼吸暂停性头痛10.2 Dialysis headache10.3 Headache attributed to arterial hypertension高血压性头痛10.3.1 Headache attributed to phaeochromocytoma嗜络细胞瘤10.3.2 Headache attributed to hypertensive crisis without hypertensive encephalopathy无高血压脑病的高血压危象10.3.3 Headache attributed to hypertensive encephalopathy高血压脑病10.3.4 Headache attributed to pre-eclampsia or eclampsia先兆子痫10.3.5 Headache attributed to autonomic dysreflexia自主反射障碍10.4 Headache attributed to hypothyroidism甲状腺低下10.5 Headache attributed to fasting禁食10.6 Cardiac cephalalgia心源性头痛10.7 Headache attributed to other disorder of homoeostasis其他内环境稳定失调疾患11.缘于头、颈、眼、耳、鼻、鼻窦、牙、口或其他头面部结构病变的头面痛(Headache or facial pain attributed to disorder of the cranium, neck,eyes, ears, nose, sinuses, teeth, mouth or other facial or cervical structure )11.1 Headache attributed to disorder of cranial bone颅骨11.2 Headache attributed to disorder of the neck 颈部11.2.1 Cervicogenic headache11.2.2 Headache attributed to retropharyngeal tendonitis11.2.3 Headache attributed to craniocervical dystonia11.3 Headache attributed to disorder of the eyes眼睛11.3.1 Headache attributed to acute glaucoma急性青光眼11.3.2 Headache attributed to refractive error屈光不正11.3.3 Headache attributed to heterophoria or heterotropia (latent or persistent squint)斜视11.3.4 Headache attributed to ocular inflammatory disorder11.3.5 Headache attributed to trochleitis11.4 Headache attributed to disorder of the ears耳朵11.5 Headache attributed to disorder of the nose or paranasal sinuses鼻子或鼻窦11.5.1 Headache attributed to acute rhinosinusitis急性鼻窦炎11.5.2 Headache attributed to chronic or recurring rhinosinusitis11.6 Headache attributed to disorder of the teeth or jaw11.7 Headache attributed to temporomandibular disorder (TMD)11.8 Head or facial pain attributed to inflammation of the stylohyoid ligament11.9 Headache or facial pain attributed to other disorder of cranium, neck, eyes, ears, nose,sinuses, teeth, mouth or other facial or cervical structure12.缘于精神疾病的头痛(Headache attributed to psychiatric disorder)12.1 Headache attributed to somatization disorder躯体化障碍12.2 Headache attributed to psychotic disorder精神疾病三、脑神经痛、中枢和原发性颜面痛及其他头痛(painful cranial neuropathies, other facial pains and other headaches)13.脑神经痛和中枢性颜面痛(Painful cranial neuropathies and other facial pains)13.1 Trigeminal neuralgia三叉神经痛13.1.1 Classical trigeminal neuralgia13.1.1.1 Classical trigeminal neuralgia, purely paroxysmal13.1.1.2 Classical trigeminal neuralgia with concomitant persistent facial pain13.1.2 Painful trigeminal neuropathy13.1.2.1 Painful trigeminal neuropathy attributed to acute Herpes zoster13.1.2.2 Post-herpetic trigeminal neuropathy13.1.2.3 Painful post-traumatic trigeminal neuropathy13.1.2.4 Painful trigeminal neuropathy attributed to multiple sclerosis (MS) plaque13.1.2.5 Painful trigeminal neuropathy attributed to space-occupying lesion13.1.2.6 Painful trigeminal neuropathy attributed to other disorder13.2 Glossopharyngeal neuralgia舌咽神经痛13.3 Nervus intermedius (facial nerve) neuralgia中间神经痛(面神经痛)13.3.1 Classical nervus intermedius neuralgia13.6 Headache attributed to ischaemic ocular motor nerve palsy缺血性眼神经麻痹13.7 Tolosa-Hunt syndrome13.8 Paratrigeminal oculosympathetic (Raeder’s) syndrome13.9 Recurrent painful ophthalmoplegic neuropathy复发性痛性眼肌麻痹13.10 Burning mouth syndrome (BMS)13.11 Persistent idiopathic facial pain (PIFP)13.12 Central neuropathic pain中枢神经痛13.12.1 Central neuropathic pain attributed to multiple sclerosis (MS)13.12.2 Central post-stroke pain (CPSP)14. 其他头痛(Other headache disorders)。
头痛的国际分类(第三版)中文
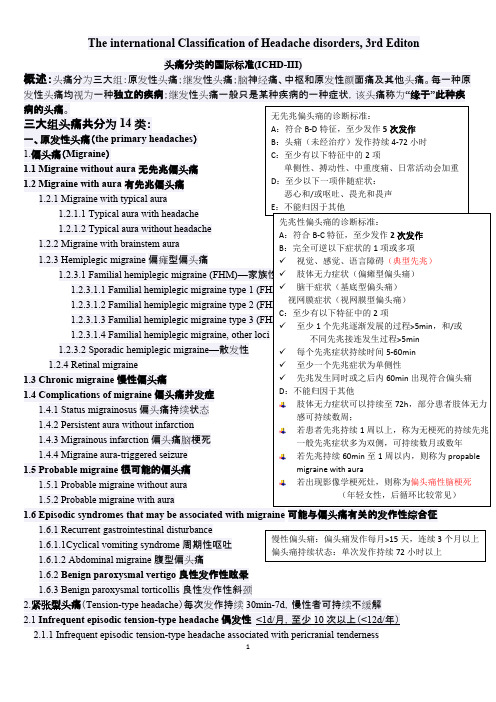
The international Classification of Headache disorders, 3rd Editon头痛分类的国际标准(ICHD-III)概述:头痛分为三大组:原发性头痛;继发性头痛;脑神经痛、中枢和原发性颜面痛及其他头痛。
每一种原发性头痛均视为一种独立的疾病;继发性头痛一般只是某种疾病的一种症状,该头痛称为“缘于”此种疾病的头痛。
三大组头痛共分为14类: 一、原发性头痛(the primary headaches ) 1.偏头痛(Migraine ) 1.1 Migraine without aura 无先兆偏头痛 1.2 Migraine with aura 有先兆偏头痛 1.2.1 Migraine with typical aura 1.2.1.1 Typical aura with headache 1.2.1.2 Typical aura without headache 1.2.2 Migraine with brainstem aura 1.2.3 Hemiplegic migraine 偏瘫型偏头痛1.2.3.1 Familial hemiplegic migraine (FHM)—家族性 1.2.3.1.1 Familial hemiplegic migraine type 1 (FHM1) 1.2.3.1.2 Familial hemiplegic migraine type 2 (FHM2) 1.2.3.1.3 Familial hemiplegic migraine type 3 (FHM3) 1.2.3.1.4 Familial hemiplegic migraine, other loci 1.2.3.2 Sporadic hemiplegic migraine —散发性 1.2.4 Retinal migraine 1.3 Chronic migraine 慢性偏头痛1.4 Complications of migraine 偏头痛并发症1.4.1 Status migrainosus 偏头痛持续状态 1.4.2 Persistent aura without infarction 1.4.3 Migrainous infarction 偏头痛脑梗死 1.4.4 Migraine aura-triggered seizure 1.5 Probable migraine 很可能的偏头痛 1.5.1 Probable migraine without aura1.5.2 Probable migraine with aura 1.6 Episodic syndromes that may be associated with migraine 可能与偏头痛有关的发作性综合征1.6.1 Recurrent gastrointestinal disturbance1.6.1.1Cyclical vomiting syndrome 周期性呕吐 1.6.1.2 Abdominal migraine 腹型偏头痛1.6.2 Benign paroxysmal vertigo 良性发作性眩晕1.6.3 Benign paroxysmal torticollis 良性发作性斜颈2.紧张型头痛(Tension-type headache )每次发作持续30min-7d ,慢性者可持续不缓解2.1 Infrequent episodic tension-type headache 偶发性 <1d/月,至少10次以上(<12d/年)2.1.1 Infrequent episodic tension-type headache associated with pericranial tenderness无先兆偏头痛的诊断标准:A :符合B-D 特征,至少发作5次发作B :头痛(未经治疗)发作持续4-72小时C :至少有以下特征中的2项单侧性、搏动性、中重度痛、日常活动会加重D :至少以下一项伴随症状:恶心和/或呕吐、畏光和畏声E :不能归因于其他 先兆性偏头痛的诊断标准:A :符合B-C 特征,至少发作2次发作B :完全可逆以下症状的1项或多项✓ 视觉、感觉、语言障碍(典型先兆)✓ 肢体无力症状(偏瘫型偏头痛)✓ 脑干症状(基底型偏头痛)视网膜症状(视网膜型偏头痛)C :至少有以下特征中的2项 ✓ 至少1个先兆逐渐发展的过程>5min ,和/或 不同先兆接连发生过程>5min ✓ 每个先兆症状持续时间5-60min✓ 至少一个先兆症状为单侧性✓ 先兆发生同时或之后内60min 出现符合偏头痛 D :不能归因于其他 肢体无力症状可以持续至72h ,部分患者肢体无力感可持续数周; 若患者先兆持续1周以上,称为无梗死的持续先兆一般先兆症状多为双侧,可持续数月或数年 若先兆持续60min 至1周以内,则称为propablemigraine with aura若出现影像学梗死灶,则称为偏头痛性脑梗死 (年轻女性,后循环比较常见) 慢性偏头痛:偏头痛发作每月>15天,连续3个月以上 偏头痛持续状态:单次发作持续72小时以上4.5 Cold-stimulus headache 冷刺激性头痛 4.5.1 Headache attributed to external application of a cold stimulus4.5.2 Headache attributed to ingestion or inhalation of a cold stimulus 4.5.3 Probable cold-stimulus headache4.5.3.1 Headache probably attributed to external application of a cold stimulus4.5.3.2 Headache probably attributed to ingestion or inhalation of a cold stimulus 4.6 External-pressure headache 4.6.1 External-compression headache 4.6.2 External-traction headache 4.6.3 Probable external-pressure headache4.6.3.1 Probable external-compression headache 4.6.3.2 Probable external-traction headache 4.7 Primary stabbing headache4.7.1 Probable primary stabbing headache4.8 Nummular headache4.8.1 Probable nummular headache4.9 Hypnic headache4.9.1 Probable hypnic headache4.10 New daily persistent headache (NDPH) 新症每日持续性头痛4.10.1 Probable new daily persistent headach 二、继发性头痛(the secondary headaches )5.缘于头、颈部外伤的头痛(Headache attributed to trauma or injury to the head and/or neck )5.1 Acute headache attributed to traumatic injury to the head5.1.1 Acute headache attributed to moderate or severe traumatic injury to the head5.1.2 Acute headache attributed to mild traumatic injury to the head5.2 Persistent headache attributed to traumatic injury to the head5.2.1 Persistent headache attributed to moderate or severe traumatic injury to the head5.2.2 Persistent headache attributed to mild traumatic injury to the head5.3 Acute headache attributed to whiplash5.4 Persistent headache attributed to whiplash5.5 Acute headache attributed to craniotomy5.6 Persistent headache attributed to craniotomy6.缘于头颈部血管疾病的头痛(Headache attributed to cranial or cervical vascular disorder )6.1 Headache attributed to ischaemic stroke or transient ischaemic attack6.1.1 Headache attributed to ischaemic stroke (cerebral infarction)6.1.2 Headache attributed to transient ischaemic attack (TIA)6.2 Headache attributed to non-traumatic intracranial haemorrhage6.2.1 Headache attributed to non-traumatic intracerebral haemorrhage 非外伤性脑出血6.2.2 Headache attributed to non-traumatic subarachnoid haemorrhage (SAH)6.2.3 Headache attributed to non-traumatic acute subdural haemorrhage (ASDH)急性硬膜下血肿NDPH 诊断标准: A :持续性头痛,符合B-C 的标准B :Distinct and clearly remembered onset, with pain becomingcontinuous and unremitting within 24 hours C :Present for>3 monthsD :除外其他疾患 慢性头痛,起病急,可清晰回忆发病时间为哪一天 疼痛缺乏特点,可以为偏头痛,可以为紧张性,亦可两者混合 若患者符合慢性偏头痛或慢性紧张型头痛的标准,则不诊断NDPH 若患者为药物过度使用性头痛,且符合NDPH 的标准, 则可两者均可作为诊断6.3 Headache attributed to unruptured vascular malformation 未破裂的血管畸形6.3.1 Headache attributed to unruptured saccular aneurysm囊性动脉瘤6.3.2 Headache attributed to arteriovenous malformation (AVM) 动静脉畸形6.3.3 Headache attributed to dural arteriovenous fistula (DAVF) 硬膜动静脉瘘6.3.4 Headache attributed to cavernous angioma 海绵窦血管瘤6.3.5 Headache attributed to encephalotrigeminal or leptomeningeal angiomatosis (Sturge Weber syndrome) 脑三叉神经或软脑膜血管瘤病6.4 Headache attributed to arteritis6.4.1 Headache attributed to giant cell arteritis (GCA) 颞动脉炎6.4.2 Headache attributed to primary angiitis of the central nervous system (PACNS)6.4.3 Headache attributed to secondary angiitis of the central nervous system (SACNS)颞动脉炎诊断标准:美国风湿学会1990年1. 50岁以上发病:50岁以上发现症状2.新发的头痛:出现新发的局限性头痛3.颞动脉异常:颞动脉压痛或者与颈动脉的动脉硬化无关的搏动减弱4.血沉值升高:50mm/h以上5.动脉活检异常:单核细胞为主的细胞浸润或者伴多核巨细胞的肉芽肿出现为特征的血管炎证据5项中如满足3项以上,敏感度93.5%。
前庭性偏头痛

叉血管反射;)
2、三叉血管系统激活:(无菌性炎性渗出反应;双侧
前庭张力不平衡;)
3、血浆外渗;
4、神经介质释放;
5、血管痉挛;
6、遗传因素;
7、离子通道基因缺陷等。
VM发作的常见诱因:
月经 睡眠不足 过度紧张及压力劳累 特别食物(红酒、奶酪、味精) 感觉刺激(耀眼夺目的光,强烈刺激,噪声) 前庭刺激可诱发偏头痛,例如温度实验
√ 2、很可能的VM
√ • A. 至少5次中重度前庭症状发作,持续时间5分钟至72小时 • B. 仅符合前庭性偏头痛诊断标准中的一项B或C(偏头痛病史 或发作时的偏头痛表现) • C. 不符合其他前庭疾病诊断或其他ICHD诊断
前庭性偏头痛
偏
前
头 痛 病
VM
庭 性
史
晕
曾经有痛
追问
小贴士:
•神经科医生不懂前庭外周疾病 不容易看明白头晕病人; •耳科医生不懂头痛和脑血管其病他 也不容易看明白头晕病人;
预防性治疗
小贴士: 小剂量开始,逐渐增加药量; 持续使用至少1年。
钙通道维Te阻拉x滞帕t 剂米:、氟桂利嗪
其他: 乙酰唑胺
药物
三环抗抑郁药: 去甲替林、奥氮平
抗癫痫药
Text
β受体阻滞剂: 普萘洛尔、比索洛尔、美托洛尔
规律 运动
前庭康复训练
规律 饮食睡眠
避免已 知诱因
非药物治疗
前庭性偏头痛
vestibular migraine
你遇到过这几种表现的眩晕病人吗?
反复发作的眩晕伴头疼
被诊断为梅尼埃病十余年无听力减退
反复发作的眩晕病史,但是每次休息后可 自愈,或是用药后马上好转,发作间隔期 无明显身体不适或行走不稳
头痛的分类及诊断流程

头痛的分类及诊断流程
第17页
担心型头痛诊疗标准-3
2.3 慢性担心型头痛
A. 最少3个月,每个月发作不少于15天(每年发作>180天,并符合诊疗标准 B~D);
B. 头痛连续数小时或连续发作: C. 头痛最少有以下特点中2个:
①双侧头痛; ②性质为压迫性或紧箍样(非搏动性); ③轻到中度头痛; ④日常活动如行走或上楼梯不加重头痛;
头痛的分类及诊断流程
第12页
பைடு நூலகம்
有偏头痛经典先兆性偏头痛诊疗标准-2
C. 最少符合以下2条:
①双侧视觉症状和/或单侧感觉症状; ②最少一个先兆症状逐步进展时间≥5分钟和/或不一样先兆症状接连
出现≥5分钟; ③每个症状≥5分钟并≤60分钟
D. 在先兆期或先兆症状随即60分钟之内出现了符合无先 兆性偏头痛B~D标准头痛
Neurology ;63:427-35
头痛的分类及诊断流程
第5页
第二版《国际头痛疾患分类》
(一)原发性头痛 1. 偏头痛 2. 担心型头痛 3. 丛集性头痛和其它三叉自主神经性痛 4. 其它原发性头痛
头痛的分类及诊断流程
第6页
第二版《国际头痛疾患分类》
(二)继发性头痛
5. 归因于头和/或颈创伤头痛 6. 归因于颅或颈部血管疾病头痛 7. 归因于非血管性颅内疾病头痛 8. 归因于某种物质或其戒断头痛 9. 归因于感染头痛 10. 归因于代谢性疾病头痛 11. 归因于颅、颈、眼、耳、鼻、鼻窦、牙齿、口腔、和其它头面部结
头痛的分类及诊断流程
第14页
担心型头痛(TTH)分类-2
2.3 慢性担心型头痛
2.3.1伴颅周压痛慢性担心型头痛 2.3.2不伴颅周压痛慢性担心型头痛
头痛地国际分类第三版中文

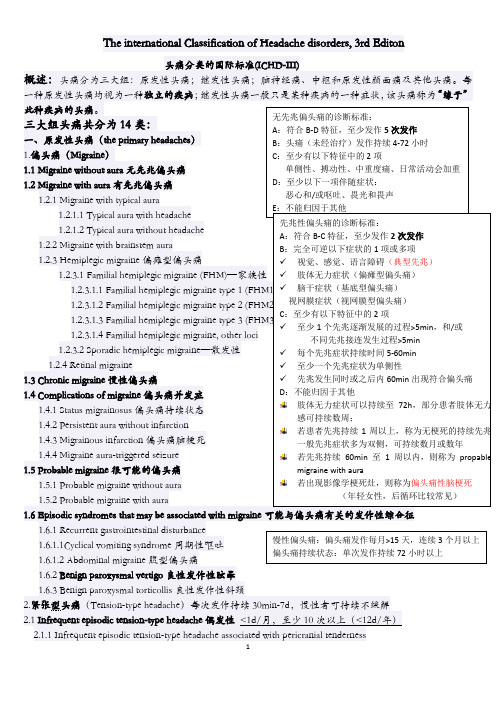
The international Classification of Headache disorders, 3rd Editon 头痛分类的国际标准(ICHD-III)概述:头痛分为三大组:原发性头痛;继发性头痛;脑神经痛、中枢和原发性颜面痛及其他头痛。
每一种原发性头痛均视为一种独立的疾病;继发性头痛一般只是某种疾病的一种症状,该头痛称为“缘于”此种疾病的头痛。
三大组头痛共分为14类: 一、原发性头痛(the primary headaches ) 1.偏头痛(Migraine ) 1.1 Migraine without aura 无先兆偏头痛 1.2 Migraine with aura 有先兆偏头痛 1.2.1 Migraine with typical aura1.2.1.1 Typical aura with headache 1.2.1.2 Typical aura without headache 1.2.2 Migraine with brainstem aura 1.2.3 Hemiplegic migraine 偏瘫型偏头痛1.2.3.1 Familial hemiplegic migraine (FHM)—家族性 1.2.3.1.1 Familial hemiplegic migraine type 1 (FHM1)1.2.3.1.2 Familial hemiplegic migraine type 2 (FHM2)1.2.3.1.3 Familial hemiplegic migraine type 3 (FHM3) 1.2.3.1.4 Familial hemiplegic migraine, other loci 1.2.3.2 Sporadic hemiplegic migraine —散发性 1.2.4 Retinal migraine 1.3 Chronic migraine 慢性偏头痛1.4 Complications of migraine 偏头痛并发症1.4.1 Status migrainosus 偏头痛持续状态 1.4.2 Persistent aura without infarction 1.4.3 Migrainous infarction 偏头痛脑梗死 1.4.4 Migraine aura-triggered seizure 1.5 Probable migraine 很可能的偏头痛 1.5.1 Probable migraine without aura1.5.2 Probable migraine with aura 1.6 Episodic syndromes that may be associated with migraine 可能与偏头痛有关的发作性综合征1.6.1 Recurrent gastrointestinal disturbance1.6.1.1Cyclical vomiting syndrome 周期性呕吐 1.6.1.2 Abdominal migraine 腹型偏头痛1.6.2 Benign paroxysmal vertigo 良性发作性眩晕1.6.3 Benign paroxysmal torticollis 良性发作性斜颈2.紧张型头痛(Tension-type headache )每次发作持续30min-7d ,慢性者可持续不缓解2.1 Infrequent episodic tension-type headache 偶发性 <1d/月,至少10次以上(<12d/年)2.1.1 Infrequent episodic tension-type headache associated with pericranial tenderness无先兆偏头痛的诊断标准:A :符合B-D 特征,至少发作5次发作B :头痛(未经治疗)发作持续4-72小时C :至少有以下特征中的2项单侧性、搏动性、中重度痛、日常活动会加重D :至少以下一项伴随症状:恶心和/或呕吐、畏光和畏声E :不能归因于其他 先兆性偏头痛的诊断标准:A :符合B-C 特征,至少发作2次发作B :完全可逆以下症状的1项或多项✓ 视觉、感觉、语言障碍(典型先兆)✓ 肢体无力症状(偏瘫型偏头痛)✓ 脑干症状(基底型偏头痛) 视网膜症状(视网膜型偏头痛) C :至少有以下特征中的2项 ✓ 至少1个先兆逐渐发展的过程>5min ,和/或 不同先兆接连发生过程>5min ✓ 每个先兆症状持续时间5-60min✓ 至少一个先兆症状为单侧性✓ 先兆发生同时或之后内60min 出现符合偏头痛 D :不能归因于其他 肢体无力症状可以持续至72h ,部分患者肢体无力感可持续数周; 若患者先兆持续1周以上,称为无梗死的持续先兆一般先兆症状多为双侧,可持续数月或数年若先兆持续60min 至1周以内,则称为propablemigraine with aura若出现影像学梗死灶,则称为偏头痛性脑梗死 (年轻女性,后循环比较常见) 慢性偏头痛:偏头痛发作每月>15天,连续3个月以上偏头痛持续状态:单次发作持续72小时以上4.3.1 Probable primary headache associated with sexual activity 4.4 Primary thunderclap headache 原发性霹雳头痛 4.5 Cold-stimulus headache 冷刺激性头痛 4.5.1 Headache attributed to external application of a cold stimulus4.5.2 Headache attributed to ingestion or inhalation of a cold stimulus4.5.3 Probable cold-stimulus headache 4.5.3.1 Headache probably attributed to external application of a cold stimulus4.5.3.2 Headache probably attributed to ingestion or inhalation of a cold stimulus4.6 External-pressure headache 4.6.1 External-compression headache 4.6.2 External-traction headache 4.6.3 Probable external-pressure headache4.6.3.1 Probable external-compression headache4.6.3.2 Probable external-traction headache 4.7 Primary stabbing headache 4.7.1 Probable primary stabbing headache 4.8 Nummular headache 4.8.1 Probable nummular headache4.9 Hypnic headache4.9.1 Probable hypnic headache4.10 New daily persistent headache (NDPH) 新症每日持续性头痛4.10.1 Probable new daily persistent headach 二、继发性头痛(the secondary headaches )5.缘于头、颈部外伤的头痛(Headache attributed to trauma or injury to the head and/or neck )5.1 Acute headache attributed to traumatic injury to the head5.1.1 Acute headache attributed to moderate or severe traumatic injury to the head5.1.2 Acute headache attributed to mild traumatic injury to the head5.2 Persistent headache attributed to traumatic injury to the head5.2.1 Persistent headache attributed to moderate or severe traumatic injury to the head5.2.2 Persistent headache attributed to mild traumatic injury to the head5.3 Acute headache attributed to whiplash5.4 Persistent headache attributed to whiplash5.5 Acute headache attributed to craniotomy5.6 Persistent headache attributed to craniotomy6.缘于头颈部血管疾病的头痛(Headache attributed to cranial or cervical vascular disorder )6.1 Headache attributed to ischaemic stroke or transient ischaemic attack6.1.1 Headache attributed to ischaemic stroke (cerebral infarction)6.1.2 Headache attributed to transient ischaemic attack (TIA)6.2 Headache attributed to non-traumatic intracranial haemorrhage6.2.1 Headache attributed to non-traumatic intracerebral haemorrhage 非外伤性脑出血6.2.2 Headache attributed to non-traumatic subarachnoid haemorrhage (SAH)NDPH 诊断标准:A :持续性头痛,符合B-C 的标准B :Distinct and clearly remembered onset, with pain becomingcontinuous and unremitting within 24 hours C :Present for>3 months D :除外其他疾患慢性头痛,起病急,可清晰回忆发病时间为哪一天 疼痛缺乏特点,可以为偏头痛,可以为紧张性,亦可两者混合若患者符合慢性偏头痛或慢性紧张型头痛的标准,则不诊断NDPH 若患者为药物过度使用性头痛,且符合NDPH 的标准, 则可两者均可作为诊断6.2.3 Headache attributed to non-traumatic acute subdural haemorrhage (ASDH)急性硬膜下血肿6.3 Headache attributed to unruptured vascular malformation未破裂的血管畸形6.3.1 Headache attributed to unruptured saccular aneurysm囊性动脉瘤6.3.2 Headache attributed to arteriovenous malformation (AVM) 动静脉畸形6.3.3 Headache attributed to dural arteriovenous fistula (DAVF) 硬膜动静脉瘘6.3.4 Headache attributed to cavernous angioma 海绵窦血管瘤6.3.5 Headache attributed to encephalotrigeminal or leptomeningeal angiomatosis (Sturge Weber syndrome)脑三叉神经或软脑膜血管瘤病6.4 Headache attributed to arteritis6.4.1 Headache attributed to giant cell arteritis (GCA) 颞动脉炎6.4.2 Headache attributed to primary angiitis of the central nervous system (PACNS)6.4.3 Headache attributed to secondary angiitis of the central nervous system (SACNS)颞动脉炎诊断标准:美国风湿学会1990年1. 50岁以上发病:50岁以上发现症状2.新发的头痛:出现新发的局限性头痛3.颞动脉异常:颞动脉压痛或者与颈动脉的动脉硬化无关的搏动减弱4.血沉值升高:50mm/h以上5.动脉活检异常:单核细胞为主的细胞浸润或者伴多核巨细胞的肉芽肿出现为特征的血管炎证据5项中如满足3项以上,敏感度93.5%。
国际头痛疾患分类第3版_试用版_原发性头痛部分解读_冯智英
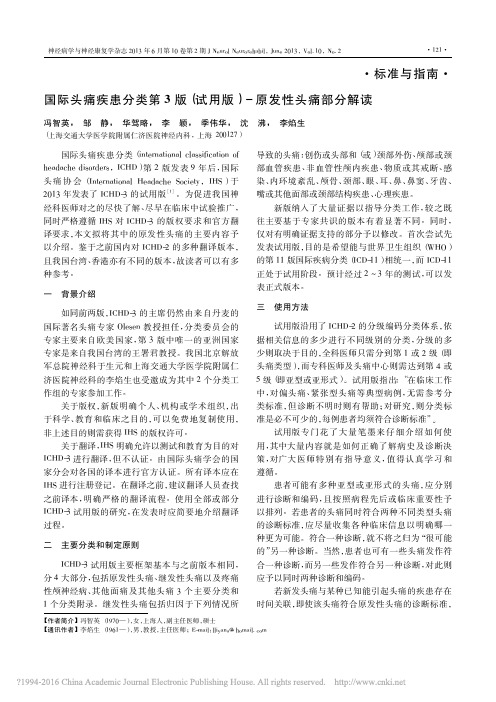
试用版沿用了 ICHD-2 的分级编码分类体系,依 据相关信息 的 多 少 进 行 不 同 级 别 的 分 类,分 级 的 多 少则取决于目的,全科医师只需分到第 1 或 2 级( 即 头痛类型) ,而专科医师及头痛中心则需达到第 4 或 5 级( 即亚型或亚形式) 。试用版指出: “在临床工作 中,对 偏 头 痛、紧 张 型 头 痛 等 典 型 病 例,无 需 参 考 分 类标准,但诊断不明时则有帮助; 对研究,则分类标 准是必不可少的,每例患者均须符合诊断标准”。
神经病学与神经康复学杂志 2013 年 6 月第 10 卷第 2 期 J Neurol Neurorehabil,June 2013,Vol. 10,No. 2
·123·
偏头痛双侧 更 为 常 见,偏 侧 头 痛 多 始 于 青 年 或 成 年 早期。偏头 痛 的 头 痛 常 位 于 额 和 颞 部,儿 童 枕 部 头 痛极罕见,诊 断 时 需 谨 慎。 有 些 其 他 表 现 典 型 的 患 者 的 疼 痛 位 于 颜 面 部,在 文 献 中 称 为‘颜 面 性 偏 头 痛’,没有证 据 提 示 这 些 患 者 为 独 立 的 偏 头 痛 亚 型。 在年幼儿 童,可 从 其 行 为 推 断 有 畏 光 和 畏 声。 偏 头 痛发作可伴随有头部自主神经症状和皮肤异常疼痛 ( allodynia) 症状。
无先兆偏头痛常与月经有关。ICHD-3 试用版给 出了 A1. 1. 1 单纯月经性偏头痛和 A1. 1. 2 月经相关 性偏头痛的 诊 断 标 准,但 由 于 不 能 确 定 它 们 是 否 应 视作单独的疾病实体而列在附录中。
非常频繁 的 偏 头 痛 发 作 现 归 为 1. 3 慢 性 偏 头 痛。当与药物过度使用有关时,则应同时诊断为 1. 3 慢性偏头痛和 8. 2 药物过度使用性头痛。当频繁使 用症状性药物治疗时,1. 1 无先兆偏头痛是最易于导 致频繁使用对症药物的情况。
国际头痛诊断标准

国际头痛诊断标准国际头痛诊断标准是指世界范围内普遍适用的诊断头痛疾病的标准。
这个标准是由国际头痛协会制定并持续更新的,旨在帮助医生更好地诊断、治疗和管理头痛疾病。
根据国际头痛诊断标准,头痛可以分为两大类:原发性头痛和继发性头痛。
原发性头痛是指没有已知病因的头痛,如偏头痛、紧张性头痛、群集性头痛等。
继发性头痛是指由其他原因引起的头痛,如颅脑损伤、感染、血管疾病等。
根据头痛的临床特点和频率等不同的表现,国际头痛诊断标准进一步将原发性头痛细分为不同的类型。
其中,偏头痛是最常见的类型之一,其诊断标准是:符合以下两个条件中的第一条和第二条,以及所有的三至六条:1. 发作时头痛为中至重度的搏动性、跳动性疼痛,常伴有恶心、呕吐、光过敏、声过敏等症状。
2. 头痛持续时间为4至72小时。
3. 头痛每个月发作至少2次。
4. 头痛符合以下条件之一:a. 位于头的一侧;b. 只在头的一侧或基本只在头的一侧;c. 在头的一侧或基本只在头的一侧,并且头痛的强度或质地在另一侧轻微或部分缺失。
5. 头痛符合以下条件之一:a. 伴有神经系统症状,如视觉障碍、感觉异常、肢体无力等;b. 引起注意力降低或狭窄;c. 发作前出现典型的神经系统症状,如视觉幻觉、口齿不清等。
6. 头痛不符合紧张性头痛、硬膜外血肿、颅内占位性病变、颅内炎症、颅内血管畸形等其他头痛疾病的诊断标准。
此外,国际头痛诊断标准还规定了其他原发性头痛的诊断标准,如紧张性头痛、群集性头痛、原发性咳嗽性头痛等。
继发性头痛的诊断要根据病因进行诊断,如头外伤引起的头痛、脑垂体瘤引起的头痛等。
在诊断头痛疾病时,医生需要仔细询问病史、观察头痛的临床表现、进行必要的检查和鉴别诊断,采用遵循国际头痛诊断标准的方法进行诊断,并针对性地进行治疗和管理。
头痛分类的国际标准

头痛分类的国际标准按照头痛分类的国际标准( ICHD-III)的分类标准,临床上头痛一共有14种类型,每种类型又包含若干种头痛。
偏头痛▎概述临床最常见的原发性头痛,人群中患病率高达5%-10%,也就是说在中国有至少有6500万的患者。
头痛发作位置大多如图所示,疼痛为中重度搏动样头痛,可持续4-72小时,非常影响患者生活。
▎诱因偏头痛的诱因非常复杂,据美国流行病调查统计,大约70%-80%的患者有家族史,同时外界因素(声、光刺激等)和生活规律(食物、睡眠、压力等)也可能引发偏头痛。
▎治疗因此对偏头痛的治疗方案也较多,如果考虑针对病因的治疗,可以让患者记录下每次发作的时间、地点和状况,以便分析其诱因。
针对中轻度头痛,一般治疗可单用非特异性止痛药,如非甾体类消炎药(对乙酰氨基酚、萘普生、布洛芬等)。
对中重度头痛,可选用偏头痛特异性治疗药物如麦角类制剂和曲谱坦类药物。
由于这两类药物有强烈的血管收缩作用,并且长期大量使用可引起严重不良后果,因此,对于以往服用非甾体类消炎药(NSAIDs)效果较好的中重度头痛患者,可以继续给予NSAIDs类药物。
由于偏头痛诱因复杂,部分患者可建议进行心理疏导,对于慢性长期性偏头痛,美国有研究者认为认知行为治疗也是可行的替代方案。
丛集性头痛▎概述此病之所以得这么个名字,是因为它的疼痛成群结队而来,表现为一连串的密集的非搏动性剧痛。
丛集性期长达2周至3个月,每次发作持续15-180分钟。
位置如图,在一侧眼眶或额颞部。
发作时患者坐立不安,部分患者甚至会用拳击打头部以减轻疼痛。
此病发病率比偏头痛较少,近6.8/10万。
▎诱因丛集性头痛一般无家族史,可由饮酒、吸烟、缺氧、热度或高海拔等因素诱发。
其病因尚不明确,一般认为是颅内、外血管扩张导致。
Horton认为与组胺释放有关。
▎治疗对于安定类药物效果不佳的丛集性头痛可给予吸氧(100%氧气8-10L/min,10-15分钟)。
曲普坦类药物可以迅速缓解头痛。
