瑞戈非尼片说明书
瑞戈非尼(Stivarga)说明书

瑞戈非尼(Stivarga)
【规格】
40mg/片
【适应症】
用于不能通过手术切除以及使用其它已上市药物治疗无效的晚期胃肠道间质瘤(GIST)患者治疗。
【禁忌症】
对本品有严重超敏反应者禁用。
【用法用量】
160mg口服。
每天1次每28天疗程,与食物服用。
【不良反应】
最常见不良反应(≥30%)是乏力/疲乏、减低食欲和食物摄入量、手足皮肤反应(HFSR)、腹泻、口腔粘膜炎、体重减轻、感染、高血压和发音困难。
【注意事项】
1.出血:对严重或威胁生命出血永久终止用药。
2.皮肤学毒性:减低或终止Stivarga取决于皮肤学毒性的严重程度和持久性。
3.高血压:对严重或不能控制的高血压暂时或永久终止Stivarga。
4.心脏缺血和梗死:拒给Stivarga对新或急性心脏缺血/梗死和只有急性缺血事件解决后恢复。
5.可逆性后部白质脑病综合征(RPLS):终止Stivarga。
6.胃肠道穿孔或瘘管:终止Stivarga。
7.伤口愈合并发症:术前停止Stivarga,在伤口裂开患者中终止。
8.胚胎胎儿毒性:可能致胎儿危害,劝告妇女对胎儿潜在风险。
瑞戈非尼合理用药要点

瑞戈非尼合理用药要点
通用名:瑞戈非尼片
制剂与规格:片剂:40mg
适应证:
1.既往接受过甲苯磺酸索拉非尼治疗的肝细胞癌(HCC)患者。
2.既往接受过甲磺酸伊马替尼及苹果酸舒尼替尼治疗的局部晚期的、无法手术切除的或转移性胃肠道间质瘤患者。
3.既往接受过氟尿嘧啶、奥沙利铂和伊立替康为基础的化疗,以及既往接受过或不适合接受抗VEGF治疗、抗EGFR治疗(RAS野生型)的转移性结直肠癌(CRC)患者。
合理用药要点:
1.用药前无需进行基因检测。
2.药品说明书推荐剂量为160mg口服,每日一次用药3周停药1周。
基于个人的安全及耐受性考虑,可能需要中断或降低剂量,也可以考虑采用80~120mg起始剂量逐渐递增。
3.亚洲人群最常见不良反应为手足皮肤反应、肝功能异常(高胆红素血症、ALT升高、AST升高)和高血压,同时还要注意疼痛、乏力、腹泻、食欲下降及进食减少等不良反应;最严重的不良反应为重度肝损伤、出血及胃肠道穿孔及感染;有血栓、栓塞病史者应审慎使用。
4.对瑞戈非尼任一活性物质或辅料有超敏反应的患者禁用。
5.与CYP3A4活性的强抑制剂(如克拉霉素、葡萄柚汁、伊曲康唑、酮康唑、泊沙康唑、泰利霉素和伏立康唑),强UGT1A9抑制剂(如甲灭酸、二氟尼柳和尼氟酸),强CYP3A4诱导剂(利福平、苯妥英、卡马西平、苯巴比妥和贯叶连翘),需尽量避免同时使用。
瑞格非尼说明书

【特别警示】本药可引起严重甚至致命的肝毒性,用药前和用药期间应监测肝功能。
如出现肝毒性,根据其严重程度和持续时间采取适当措施(包括暂停给药、减量和停药)。
(FDA药品说明书-瑞格非尼片)【药物名称】中文通用名称:瑞格非尼英文通用名称:Regorafenib其他名称:Stivarga。
【药理分类】西药 > 肿瘤用药 > 抗肿瘤药 > 抗信号转导药【临床应用】CFDA说明书适应症尚未收集到相关资料。
其他临床应用参考1.用于治疗先前接受过含氟嘧啶、奥沙利铂、伊立替康的化疗和抗血管内皮生长因子(VEGF)、抗表皮生长因子受体(EGFR)(KRAS野生型)治疗的转移性结直肠癌(CRC)。
(FDA批准适应症)2.用于治疗先前接受过伊马替尼和舒尼替尼治疗的局部晚期、无法切除或转移性胃肠道间质细胞瘤(GIST)。
(FDA批准适应症)临床指南胃肠道间质瘤诊治指南解读肢体软组织肉瘤临床诊疗专家共识的解读中国胃肠间质瘤诊断治疗共识(2013年版)【用法与用量】国外用法用量参考成人·常规剂量·CRC、GIST1.口服给药一次160mg,一日1次,连用21日,28日为一疗程。
持续用药直至疾病进展或出现不可耐受的毒性。
·肾功能不全时剂量轻度肾功能损害[肌酐清除率(Ccr)为60-89ml/min]者无需调整剂量;中度肾功能损害(Ccr为30-59ml/min)者用药的研究资料有限;尚无重度肾功能损害或终末期肾病患者用药的研究资料。
·肝功能不全时剂量轻度(Child-Pugh分级为A级)或中度肝功能损害(Child-Pugh分级为B级)者无需调整剂量;尚无重度肝功能损害(Child-Pugh分级为C级)者用药的研究资料,故不推荐使用。
·毒性状态时剂量1.出现以下情况时,应暂停给药:(1)复发的或降低剂量后7日内无改善的2级手-足皮肤反应(HFSR);3级HFSR(暂停给药至少7日)。
瑞戈非尼英文说明书(2015年版)

FULL PRESCRIBING INFORMATION: CONTENTS* WARNING: HEPATOTOXICITY 1 INDICATIONS AND USAGE
1.1 Colorectal Cancer 1.2 Gastrointestinal Stromal Tumors
2 DOSAGE AND ADMINISTRATION 2.1 Recommended Dose 2.2 Dose Modifications
------------------------------ DRUG INTERACTIONS -----------------------------
Strong CYP3A4 inducers: Avoid strong CYP3A4 inducers. (7.1)
Strong CYP3A4 inhibitors: Avoid strong CYP3A4 inhibitors. (7.2)
Hypertension: Temporarily or permanently discontinue Stivarga for severe or uncontrolled hypertension. (5.4)
Cardiac ischemia and infarction: Withhold Stivarga for new or acute cardiac ischemia/infarction and resume only after resolution of acute ischemic events. (5.5)
瑞戈非尼片说明书

核准日期:2017年3月22日 修改日期:2017年12月5日瑞戈非尼片说明书请仔细阅读说明书并在医师指导下使用。
【药品名称】通用名称:瑞戈非尼片 商品名称:Stivarga® 拜万戈® 英文名称:Regorafenib Tablets 汉语拼音:Ruigefeini Pian【成份】主要成份:瑞戈非尼化学名称:4-[4-({[4-氯-3-(三氟甲基)苯基]氨基甲酰}氨基)-3-氟苯氧基]-N-甲基吡啶-2-甲酰胺一水合物化学结构式:分子式:C 21H 15ClF 4N 4O 3•H 2O 分子量:500.83 【性状】本品为浅粉色椭圆形薄膜衣片。
【适应症】1. 适用于治疗既往接受过以氟尿嘧啶、奥沙利铂和伊立替康为基础的化疗, 以及既往接受过或不适合接受抗VEGF 治疗、 抗EGFR 治疗(RAS 野生型)的转移性结直肠癌(mCRC )患者。
2. 既往接受过甲磺酸伊马替尼及苹果酸舒尼替尼治疗的局部晚期的、无法手术切除的或转移性的胃肠道间质瘤(GIST )患者。
3. 既往接受过索拉非尼治疗的肝细胞癌(HCC )患者。
【规格】警告:肝脏毒性•在临床研究中发生了严重的、有时是致命性的肝脏毒性; •在治疗前及治疗中进行肝功能监测;•在使用瑞戈非尼片治疗中,可根据肝功检测或肝细胞坏死所表现出来的肝脏毒性的严重程度和持续性,暂停后降低剂量或停药。
40mg【用法用量】瑞戈非尼应由在抗癌治疗给药方面有经验的医生开具。
推荐剂量推荐剂量为160mg(4片,每片含40mg 瑞戈非尼),每日一次,于每一疗程的前21天口服,28天为一疗程。
服用方法瑞戈非尼片应在每天同一时间,在低脂早餐(脂肪含量30%)后随水整片吞服。
患者不得在同一天服用两剂药物以弥补(前一天)漏服的剂量。
如果服用瑞戈非尼后出现呕吐,同一天内患者不得再次服药。
治疗时间应持续治疗直至患者不能临床受益或出现不可耐受的毒性反应。
剂量调整及特殊使用说明基于个人的安全性及耐受性考虑,可能需要中断给药或降低剂量。
STIVARGA (regorafenib) tablets, for oral use 瑞格菲尼说明书-英文版

HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use STIVARGA safely and effectively. See full prescribing information for STIVARGA.STIVARGA (regorafenib) tablets, for oral useInitial U.S. Approval: 2012WARNING: HEPATOTOXICITYSee full prescribing information for complete boxed warning.∙Severe and sometimes fatal hepatotoxicity has been observed inclinical trials. (5.1)∙Monitor hepatic function prior to and during treatment. (5.1)∙Interrupt and then reduce or discontinue Stivarga for hepatotoxicity as manifested by elevated liver function tests or hepatocellularnecrosis, depending upon severity and persistence. (2.2)-------------------------- RECENT MAJOR CHANGES --------------------------Indications and Usage (1.2) 02/2013 Warnings and Precautions (5.1, 5.2, 5.3, 5.4, 5.5) 02/2013 --------------------------- INDICATIONS AND USAGE --------------------------Stivarga is a kinase inhibitor indicated for the treatment of patients with:∙Metastatic colorectal cancer (CRC) who have been previously treated with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy, an anti-VEGF therapy, and, if KRAS wild type, an anti-EGFR therapy. (1.1)∙Locally advanced, unresectable or metastatic gastrointestinal stromal tumor (GIST) who have been previously treated with imatinib mesylate and sunitinib malate. (1.2)---------------------- DOSAGE AND ADMINISTRATION ----------------------∙Recommended Dose: 160 mg orally, once daily for the first 21 days of each 28-day cycle. (2.1)∙Take Stivarga with food (a low-fat breakfast). (2.1, 12.3)--------------------- DOSAGE FORMS AND STRENGTHS --------------------40 mg film-coated tablets (3)------------------------------ CONTRAINDICATIONS -----------------------------None.----------------------- WARNINGS AND PRECAUTIONS ----------------------∙Hemorrhage: Permanently discontinue Stivarga for severe or life-threatening hemorrhage. (5.2) ∙Dermatological toxicity: Interrupt and then reduce or discontinue Stivarga depending on severity and persistence of dermatologic toxicity. (5.3)∙Hypertension: Temporarily or permanently discontinue Stivarga for severe or uncontrolled hypertension. (5.4)∙Cardiac ischemia and infarction: Withhold Stivarga for new or acute cardiac ischemia/infarction and resume only after resolution of acute ischemic events. (5.5)∙Reversible Posterior Leukoencephalopathy Syndrome (RPLS): Discontinue Stivarga. (5.6)∙Gastrointestinal perforation or fistulae: Discontinue Stivarga. (5.7)∙Wound healing complications: Stop Stivarga before surgery. Discontinue in patients with wound dehiscence. (5.8)∙Embryofetal toxicity: Can cause fetal harm. Advise women of potential risk to a fetus. (5.9, 8.1)------------------------------ ADVERSE REACTIONS -----------------------------The most common adverse reactions (≥20%) are asthenia/fatigue, HFSR, diarrhea, decreased appetite/food intake, hypertension, mucositis, dysphonia, and infection, pain (not otherwise specified), decreased weight, gastrointestinal and abdominal pain, rash, fever, and nausea. (6)To report SUSPECTED ADVERSE REACTIONS, contact Bayer HealthCare Pharmaceuticals Inc. at 1-888-842-2937 or FDA at 1-800-FDA-1088 or /medwatch------------------------------ DRUG INTERACTIONS -----------------------------• Strong CYP3A4 inducers: Avoid strong CYP3A4 inducers. (7.1)• Strong CYP3A4 inhibitors: Avoid strong CYP3A4 inhibitors. (7.2)----------------------- USE IN SPECIFIC POPULATIONS ----------------------Nursing Mothers: Discontinue drug or nursing, taking into consideration the importance of the drug to the mother. (8.3)See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.Revised: 02/20137.2 Effect of Strong CYP3A4 Inhibitors on RegorafenibFULL PRESCRIBING INFORMATION: CONTENTS* 8 USE IN SPECIFIC POPULATIONS8.1 PregnancyWARNING: HEPATOTOXICITY 8.3 Nursing Mothers1 INDICATIONS AND USAGE 8.4 Pediatric Use1.1 Colorectal Cancer 8.5 Geriatric Use1.2 Gastrointestinal Stromal Tumors 8.6 Hepatic Impairment2 DOSAGE AND ADMINISTRATION 8.7 Renal Impairment2.1 Recommended Dose 8.8 Females and Males of Reproductive Potential2.2 Dose Modifications 10 OVERDOSAGE3 DOSAGE FORMS AND STRENGTHS 11 DESCRIPTION4 CONTRAINDICATIONS 12 CLINICAL PHARMACOLOGY5 WARNINGS AND PRECAUTIONS 12.1 Mechanism of Action5.1 Hepatotoxicity 12.3 Pharmacokinetics5.2 Hemorrhage 13 NONCLINICAL TOXICOLOGY5.3 Dermatological Toxicity 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility5.4 Hypertension 13.2 Animal Toxicology and/or Pharmacology5.5 Cardiac Ischemia and Infarction 14 CLINICAL STUDIES5.6 Reversible Posterior Leukoencephalopathy Syndrome (RPLS) 14.1 Colorectal Cancer5.7 Gastrointestinal Perforation or Fistula 14.2 Gastrointestinal Stromal Tumors5.8 Wound Healing Complications 16 HOW SUPPLIED/STORAGE AND HANDLING5.9 Embryo-Fetal Toxicity 16.1 How Supplied6 ADVERSE REACTIONS 16.2 Storage and Handling6.1 Clinical Trials Experience 17 PATIENT COUNSELING INFORMATION7 DRUG INTERACTIONS7.1 Effect of Strong CYP3A4 Inducers on Regorafenib*Sections or subsections omitted from the full prescribing information are not listed.FULL PRESCRIBING INFORMATIONWARNING: HEPATOTOXICITY∙Severe and sometimes fatal hepatotoxicity has been observed in clinical trials [see Warnings and Precautions(5.1)].∙Monitor hepatic function prior to and during treatment [see Warnings and Precautions (5.1)].∙Interrupt and then reduce or discontinue Stivarga for hepatotoxicity as manifested by elevated liver function tests or hepatocellular necrosis, depending upon severity and persistence [see Dosage and Administration (2.2)].1 INDICATIONS AND USAGE1.1 Colorectal CancerStivarga® is indicated for the treatment of patients with metastatic colorectal cancer (CRC) who have been previously treated with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy, an anti-VEGF therapy, and, if KRAS wild type, an anti-EGFR therapy.1.2 Gastrointestinal Stromal TumorsStivarga is indicated for the treatment of patients with locally advanced, unresectable or metastatic gastrointestinal stromal tumor (GIST) who have been previously treated with imatinib mesylate and sunitinib malate.2 DOSAGE AND ADMINISTRATION2.1 Recommended DoseThe recommended dose is 160 mg regorafenib (four 40 mg tablets) taken orally once daily for the first 21 days of each 28day cycle. Continue treatment until disease progression or unacceptable toxicity.Take Stivarga at the same time each day. Swallow tablet whole with a low-fat breakfast that contains less than 30% fat [see Clinical Pharmacology (12.3)]. Examples of a low-fat breakfast include 2 slices of white toast with 1 tablespoon of low-fat margarine and 1 tablespoon of jelly, and 8 ounces of skim milk (319 calories and 8.2 g fat); or 1 cup of cereal, 8 ounces of skim milk, 1 slice of toast with jam, apple juice, and 1 cup of coffee or tea (520 calories and 2 g fat). Do not take two doses of Stivarga on the same day to make up for a missed dose from the previous day.2.2 Dose ModificationsInterrupt Stivarga for the following:∙NCI CTCAE Grade 2 hand-foot skin reaction (HFSR) [palmar-plantar erythrodysesthesia (PPE)] that is recurrent or does not improve within 7 days despite dose reduction; interrupt therapy for a minimum of 7 days for Grade 3 HFSR ∙Symptomatic Grade 2 hypertension∙Any NCI CTCAE Grade 3 or 4 adverse reactionReduce the dose of Stivarga to 120 mg:∙For the first occurrence of Grade 2 HFSR of any duration∙After recovery of any Grade 3 or 4 adverse reaction∙For Grade 3 aspartate aminotransferase (AST)/alanine aminotransferase (ALT) elevation; only resume if the potential benefit outweighs the risk of hepatotoxicityReduce the dose of Stivarga to 80 mg:∙For re-occurrence of Grade 2 HFSR at the 120 mg dose∙After recovery of any Grade 3 or 4 adverse reaction at the 120 mg dose (except hepatotoxicity)Discontinue Stivarga permanently for the following:∙Failure to tolerate 80 mg dose∙Any occurrence of AST or ALT more than 20 times the upper limit of normal (ULN)∙Any occurrence of AST or ALT more than 3 times ULN with concurrent bilirubin more than 2 times ULN∙Re-occurrence of AST or ALT more than 5 times ULN despite dose reduction to 120 mg∙For any Grade 4 adverse reaction; only resume if the potential benefit outweighs the risks3 DOSAGE FORMS AND STRENGTHSStivarga is a 40 mg, light pink, oval shaped, film-coated tablet, debossed with ‘BAYER’ on one side and ‘40’ on the other side.4 CONTRAINDICATIONSNone5 WARNINGS AND PRECAUTIONS5.1 HepatotoxicitySevere drug induced liver injury with fatal outcome occurred in 0.3% of 1200 Stivarga-treated patients across all clinical trials. Liver biopsy results, when available, showed hepatocyte necrosis with lymphocyte infiltration. In Study 1, fatal hepatic failure occurred in 1.6% of patients in the regorafenib arm and in 0.4% of patients in the placebo arm; all the patients with hepatic failure had metastatic disease in the liver. In Study 2, fatal hepatic failure occurred in 0.8% of patients in the regorafenib arm [see Adverse Reactions (6.1)].Obtain liver function tests (ALT, AST and bilirubin) before initiation of Stivarga and monitor at least every two weeks during the first 2 months of treatment. Thereafter, monitor monthly or more frequently as clinically indicated. Monitor liver function tests weekly in patients experiencing elevated liver function tests until improvement to less than 3 times the ULN or baseline.Temporarily hold and then reduce or permanently discontinue Stivarga depending on the severity and persistence of hepatotoxicity as manifested by elevated liver function tests or hepatocellular necrosis [see Dosage and Administration (2.2)].5.2 HemorrhageStivarga caused an increased incidence of hemorrhage. The overall incidence (Grades 1-5) was 21% and 11% in Stivargatreated patients compared to 8% and 3% in placebo-treated patients in Studies 1 and 2. Fatal hemorrhage occurred in 4 of 632 (0.6%) of Stivarga-treated patients in Studies 1 and 2 and involved the respiratory, gastrointestinal, or genitourinary tracts.Permanently discontinue Stivarga in patients with severe or life-threatening hemorrhage. Monitor INR levels more frequently in patients receiving warfarin [see Clinical Pharmacology (12.3)].5.3 Dermatological ToxicityStivarga caused increased incidences of adverse reactions involving the skin and subcutaneous tissues (72% versus 24% in Study 1 and 78% versus 24% in Study 2), including hand-foot skin reaction (HFSR) also known as palmar-plantar erythrodysesthesia (PPE), and severe rash requiring dose modification.The overall incidence of HFSR was higher in Stivarga-treated patients, (45% versus 7% in Study 1 and 67% versus 12% in Study 2), than in the placebo-treated patients. Most cases of HFSR in Stivarga-treated patients appeared during the first cycle of treatment (69% and 71% of patients who developed HFSR in Study 1 and Study 2, respectively). The incidence of Grade 3 HFSR (17% versus 0% in Study 1 and 22% versus 0% in Study 2), Grade 3 rash (6% versus <1% in Study 1 and 7% versus 0% in Study 2), serious adverse reactions of erythema multiforme (0.2% vs. 0% in Study 1) and Stevens Johnson Syndrome (0.2% vs. 0% in Study 1) was higher in Stivarga-treated patients [see Adverse Reactions (6.1)].Toxic epidermal necrolysis occurred in 0.17% of 1200 Stivarga-treated patients across all clinical trials.Withhold Stivarga, reduce the dose, or permanently discontinue Stivarga depending on the severity and persistence of dermatologic toxicity [see Dosage and Administration (2.2)]. Institute supportive measures for symptomatic relief.5.4 HypertensionStivarga caused an increased incidence of hypertension (30% versus 8% in Study 1 and 59% versus 27% in Study 2) [see Adverse Reactions (6.1)]. Hypertensive crisis occurred in 0.25% of 1200 Stivarga-treated patients across all clinical trials. The onset of hypertension occurred during the first cycle of treatment in most patients who developed hypertension (72% in Study 1 and Study 2).Do not initiate Stivarga unless blood pressure is adequately controlled. Monitor blood pressure weekly for the first 6 weeks of treatment and then every cycle, or more frequently, as clinically indicated. Temporarily or permanently withhold Stivarga for severe or uncontrolled hypertension [see Dosage and Administration (2.2)].5.5 Cardiac Ischemia and InfarctionStivarga increased the incidence of myocardial ischemia and infarction in Study 1 (1.2% versus 0.4%) [see Adverse Reactions (6.1)]. Withhold Stivarga in patients who develop new or acute onset cardiac ischemia or infarction. Resume Stivarga only after resolution of acute cardiac ischemic events, if the potential benefits outweigh the risks of further cardiac ischemia.5.6 Reversible Posterior Leukoencephalopathy Syndrome (RPLS)Reversible Posterior Leukoencephalopathy Syndrome (RPLS), a syndrome of subcortical vasogenic edema diagnosed by characteristic finding on MRI, occurred in one of 1200 Stivarga-treated patients across all clinical trials. Perform an evaluation for RPLS in any patient presenting with seizures, headache, visual disturbances, confusion or altered mental function. Discontinue Stivarga in patients who develop RPLS.5.7 Gastrointestinal Perforation or FistulaGastrointestinal perforation or fistula occurred in 0.6% of 1200 patients treated with Stivarga across all clinical trials; this included four fatal events. In Study 2, 2.1 % (4/188) of Stivarga-treated patients who were treated during the blinded or open-label portion of the study developed gastrointestinal fistula or perforation; of these, two cases of gastrointestinal perforation were fatal. Permanently discontinue Stivarga in patients who develop gastrointestinal perforation or fistula.5.8 Wound Healing ComplicationsNo formal studies of the effect of regorafenib on wound healing have been conducted. Since vascular endothelial growth factor receptor (VEGFR) inhibitors such as regorafenib can impair wound healing, treatment with regorafenib should be stopped at least 2 weeks prior to scheduled surgery. The decision to resume regorafenib after surgery should be based on clinical judgment of adequate wound healing. Regorafenib should be discontinued in patients with wound dehiscence. 5.9 Embryo-Fetal ToxicityStivarga can cause fetal harm when administered to a pregnant woman. Regorafenib was embryolethal and teratogenic in rats and rabbits at exposures lower than human exposures at the recommended dose, with increased incidences of cardiovascular, genitourinary, and skeletal malformations. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1)].6 ADVERSE REACTIONSThe following serious adverse reactions are discussed elsewhere in the labeling:∙Hepatotoxicity [See Warnings and Precautions (5.1)]∙Hemorrhage [See Warnings and Precautions (5.2)]∙Dermatological Toxicity [See Warnings and Precautions (5.3)]∙Hypertension [See Warnings and Precautions (5.4)]∙Cardiac Ischemia and Infarction [See Warnings and Precautions (5.5)]∙Reversible Posterior Leukoencephalopathy Syndrome (RPLS) [See Warnings and Precautions (5.6)]∙Gastrointestinal Perforation or Fistula [See Warnings and Precautions (5.7)]Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rate observed in practice.The most frequently observed adverse drug reactions (≥20%) in patients receiving Stivarga are asthenia/fatigue, HFSR, diarrhea, decreased appetite/food intake, hypertension, mucositis, dysphonia, infection, pain (not otherwise specified), decreased weight, gastrointestinal and abdominal pain, rash, fever, and nausea.The most serious adverse drug reactions in patients receiving Stivarga are hepatotoxicity, hemorrhage, and gastrointestinal perforation.6.1 Clinical Trials ExperienceColorectal CancerThe safety data described below, except where noted, are derived from a randomized (2:1), double-blind, placebo-controlled trial (Study 1) in which 500 patients (median age 61 years; 61% men) with previously treated metastatic colorectal cancer received Stivarga as a single agent at the dose of 160 mg daily for the first 3 weeks of each 4 week treatment cycle and 253 patients (median age 61 years; 60% men) received placebo. The median duration of therapy was 7.3 (range 0.3, 47.0) weeks for patients receiving Stivarga. Due to adverse reactions, 61% of the patients receiving Stivarga required a dose interruption and 38% of the patients had their dose reduced. Drug-related adverse reactions that resulted in treatment discontinuation were reported in 8.2% of Stivarga-treated patients compared to 1.2% of patients whoreceived placebo. Hand-foot skin reaction (HFSR) and rash were the most common reasons for permanent discontinuation of Stivarga.Table 1 compares the incidence of adverse reactions (≥10%) in patients receiving Stivarga and reported more commonly than in patients receiving placebo (Study 1).Table 1 Adverse drug reactions (≥10%) reported in patients treated with Stivarga in Study 1 and reported more commonly than in patients receiving placeboAdverse ReactionsStivarga(N=500)Placebo(N=253) Grade GradeAll%≥ 3%All%≥ 3%General disorders and administration site conditionsAsthenia/fatigue PainFever 642928153246211592Metabolism and nutrition disordersDecreased appetite and food intake 47 5 28 4Skin and subcutaneous tissue disorders HFSR/PPERash a 452617674<1Gastrointestinal disorders DiarrheaMucositis 4333841752InvestigationsWeight loss 32 <1 10 0 Infections and infestationsInfection 31 9 17 6 Vascular disordersHypertension Hemorrhage b 30218288<1<1Respiratory, thoracic and mediastinaldisordersDysphonia 30 0 6 0Nervous system disordersHeadache 10<170 a The term rash represents reports of events of drug eruption, rash, erythematous rash, generalized rash, macular rash,maculo-papular rash, papular rash, and pruritic rash.b Fatal outcomes observed.Laboratory AbnormalitiesLaboratory abnormalities observed in Study 1 are shown in Table 2. Table 2 Laboratory test abnormalities reported in Study 1Laboratory ParameterStivarga(N=500 a)Placebo(N=253 a)Grade b Grade bAll%3%4%All%3%4%Blood and lymphatic systemdisordersAnemia 79 5 1 66 3 0 Thrombocytopenia 412<117<10 Neutropenia 3 1 0 0 0 0 Lymphopenia 54 9 0 34 3 0 Metabolism and nutritiondisordersHypocalcemia 591<11810 Hypokalemia 2648<10 Hyponatremia 30 7 1 22 4 0 Hypophosphatemia 57 31 1 11 4 0 Hepatobiliary disordersHyperbilirubinemia 45 10 3 17 5 3 IncreasedAST 65 5 1 46 4 1 IncreasedALT 45 5 1 30 3 <1Renal and urinary disordersProteinuria 60 <1 0 34 <1 0 InvestigationsIncreased INR c 244N/A172N/A IncreasedLipase 46 9 2 19 3 2 Increased Amylase 26 2 <1 17 2 <1a % based on number of patients with post-baseline samples which may be less than 500 (regorafenib) or 253 (placebo).b Common Terminology Criteria for Adverse Events (CTCAE), v3.0.c International normalized ratio: No Grade 4 denoted in CTCAE, v3.0.Gastrointestinal Stromal TumorsThe safety data described below are derived from a randomized (2:1), double-blind, placebo-controlled trial (Study 2) inwhich 132 patients (median age 60 years; 64% men) with previously treated GIST received Stivarga as a single agent at adose of 160 mg daily for the first 3 weeks of each 4 week treatment cycle and 66 patients (median age 61 years; 64%men) received placebo. The median duration of therapy was 22.9 (range 0.1, 50.9) weeks for patients receiving Stivarga.Dose interruptions for adverse events were required in 58% of patients receiving Stivarga and 50% of patients had theirdose reduced. Drug-related adverse reactions that resulted in treatment discontinuation were reported in 2.3% of Stivargatreated patients compared to 1.5% of patients who received placebo.Table 3 compares the incidence of adverse reactions (≥10%) in GIST patients receiving Stivarga and reported morecommonly than in patients receiving placebo (Study 2).Table 3 Adverse reactions (≥10%) reported in patients treated with Stivarga in Study 2 and reported more commonly than in patients receiving placeboAdverse ReactionsStivarga(N=132)Placebo(N=66)Grade Grade All%≥ 3%All%≥ 3%Skin and subcutaneous tissue disordersHFSR/PPE Rash a Alopecia 673024227215322General disorders and administration site conditionsAsthenia/Fatigue Fever 52214391122Vascular disordersHypertension Hemorrhage 59112842735Gastrointestinal disordersDiarrhea Mucositis Nausea Vomiting 47402017822<19812822Respiratory, thoracic and mediastinaldisordersDysphonia 39 0 9 0Infections and infestationsInfection 32550 Metabolism and nutrition disordersDecreased appetite and food intake Hypothyroidism b 3118<12163Nervous system disordersHeadache 1690 InvestigationsWeight loss 14 0 8 0Musculoskeletal and connective tissuedisordersMusculoskeletal stiffness 14 0 3 0a The term rash represents reports of events of rash, erythematous rash, macular rash, maculo-papular rash, papular rashand pruritic rash.b Hypothyroidism incidence based on subset of patients with normal TSH and no thyroid supplementation at baseline.Laboratory AbnormalitiesLaboratory abnormalities observed in Study 2 are shown in Table 4. Table 4 Laboratory test abnormalities reported in Study 2Laboratory ParameterStivarga(N=132 a)Placebo(N=66 a)Grade b Grade bAll%3%4%All%3%4%Blood and lymphaticsystem disordersThrombocytopenia 13 1 0 2 0 2 Neutropenia 16 2 0 12 3 0 Lymphopenia 30 8 0 24 3 0 Metabolism and nutritiondisordersHypocalcemia 17 2 0 5 0 0 Hypokalemia 21 3 0 3 0 0 Hypophosphatemia 55 20 2 3 2 0 Hepatobiliary disordersHyperbilirubinemia 33 3 1 12 2 0Increased AST 58 3 1 47 3 0Increased ALT 39 4 1 39 2 0Renal and urinarydisordersProteinuria 333-c 30 3 -c InvestigationsIncreased Lipase 14 0 1 5 0 0ab CTCAE, v4.0.c No Grade 4 denoted in CTCAE, v4.0.7 DRUG INTERACTIONS7.1 Effect of Strong CYP3A4 Inducers on RegorafenibCo-administration of a strong CYP3A4 inducer (rifampin) with a single 160 mg dose of Stivarga decreased the mean exposure of regorafenib, increased the mean exposure of the active metabolite M-5, and resulted in no change in the mean exposure of the active metabolite M-2. Avoid concomitant use of strong CYP3A4 inducers (e.g. rifampin, phenytoin, carbamazepine, phenobarbital, and St. John’s Wort) [see Clinical Pharmacology (12.3)].7.2 Effect of Strong CYP3A4 Inhibitors on RegorafenibCo-administration of a strong CYP3A4 inhibitor (ketoconazole) with a single 160 mg dose of Stivarga increased the mean exposure of regorafenib and decreased the mean exposure of the active metabolites M-2 and M-5. Avoid concomitant use of strong inhibitors of CYP3A4 activity (e.g. clarithromycin, grapefruit juice, itraconazole, ketoconazole, posaconazole, telithromycin, and voriconazole) [see Clinical Pharmacology (12.3)].8 USE IN SPECIFIC POPULATIONS8.1 PregnancyPregnancy Category D [see Warnings and Precautions (5.9)]Risk SummaryBased on its mechanism of action, Stivarga can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies with Stivarga in pregnant women. Regorafenib was embryolethal and teratogenic in rats and rabbits at exposures lower than human exposures at the recommended dose, with increased incidences of cardiovascular, genitourinary, and skeletal malformations. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.Animal DataIn embryo-fetal development studies, a total loss of pregnancy (100% resorption of litter) was observed in rats at doses as low as 1 mg/kg (approximately 6% of the recommended human dose, based on body surface area) and in rabbits at doses as low as 1.6 mg/kg (approximately 25% of the human exposure at the clinically recommended dose measured by AUC).In a single dose distribution study in pregnant rats, there was increased penetration of regorafenib across the blood-brain barrier in fetuses compared to dams. In a repeat dose study with daily administration of regorafenib to pregnant rats during organogenesis, findings included delayed ossification in fetuses at doses > 0.8 mg/kg (approximately 5% of the recommended human dose based on body surface area) with dose-dependent increases in skeletal malformations including cleft palate and enlarged fontanelle at doses ≥ 1 mg/kg (approximately 10% of the clinical exposure based on AUC). At doses ≥ 1.6 mg/kg (approximately 11% of the recommended human dose based on body surface area), there were dose-dependent increases in the incidence of cardiovascular malformations, external abnormalities, diaphragmatic hernia, and dilation of the renal pelvis.In pregnant rabbits administered regorafenib daily during organogenesis, there were findings of ventricular septal defects evident at the lowest tested dose of 0.4 mg/kg (approximately 7% of the AUC in patients at the recommended dose). At doses of ≥ 0.8 mg/kg (approximately 15% of the human exposure at the recommended human dose based on AUC), administration of regorafenib resulted in dose-dependent increases in the incidence of additional cardiovascular malformations and skeletal anomalies as well as significant adverse effects on the urinary system including missing kidney/ureter; small, deformed and malpositioned kidney; and hydronephrosis. The proportion of viable fetuses that were male decreased with increasing dose in two rabbit embryo-fetal toxicity studies.8.3 Nursing MothersIt is unknown whether regorafenib or its metabolites are excreted in human milk. In rats, regorafenib and its metabolites are excreted in milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Stivarga, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.8.4 Pediatric UseThe safety and efficacy of Stivarga in pediatric patients less than 18 years of age have not been established.In 28-day repeat dose studies in rats there were dose-dependent findings of dentin alteration and angiectasis. These findings were observed at regorafenib doses as low as 4 mg/kg (approximately 25% of the AUC in humans at the recommended dose). In 13-week repeat dose studies in dogs there were similar findings of dentin alteration at doses as。
瑞戈非尼产品幻灯

石文质
本文仅供参考
瑞戈非尼是什么药?
【药品名称】
通用名称:瑞戈非尼片 商品名称:拜万戈 Stivarga 英文名称:regorafenib 汉语拼音:Rui ge fei ni pian
化学结构式:
【成份】
主要成份:瑞戈非尼 化学名称:4-[4-({[4-氯-3-(三氟 甲基)苯基]氨基甲酰}氨基)-3-氟 苯氧基]-N-甲基吡啶-2-甲酰胺一 水合物
可逆性后部脑病综合征(PRES):据报告PRES与瑞戈非尼治疗相关。PRES的体征和症状包括癫痫发作、 头痛、精神状态改变、视力障碍或皮质盲,伴随或不伴随有高血压。PRES的诊断需要脑成像证实。对于患 PRES的患者,建议停用瑞戈非尼,并控制高血压,对其他症状采取支持性医学管理。
胃肠道穿孔及瘘管:瑞戈非尼治疗的患者报告出现胃肠道穿孔(包括致命结局)和瘘管。这些事件也是腹腔 内恶性肿瘤患者常见的与疾病有关的并发症。建议对出现胃肠道穿孔或瘘的患者停用瑞戈非尼。
心肌缺血及梗死:有缺血性心脏病史的患者应监测心肌缺血的临床体征和症状。对于出现心肌缺血和(或) 梗死的患者,建议中断瑞戈非尼直至恢复。对个例患者潜在获益和风险进行仔细考虑后,可做出重新开始瑞戈 非尼治疗的决定。如果未恢复,应永久停用瑞戈非尼。
瑞戈非尼是细胞膜结合的和胞内的多种激酶的小分子抑制剂,这些激酶 参与正常的细胞功能以及肿瘤发生、肿瘤血管生成、肿瘤转移和肿瘤免 疫等病理过程。
哪些患者适合用瑞戈非尼治疗?
【适应症】
1. 适用于治疗既往接受过以氟尿嘧啶、奥沙利铂和伊立替康为基础的化 疗, 以及既往接受过或不适合接受抗VEGF治疗、抗EGFR治疗(RAS野 生型)的转移性结直肠癌(mCRC)患者。 2. 既往接受过甲磺酸伊马替尼及苹果酸舒尼替尼治疗的局部晚期的、无 法手术切除的或转移性的胃肠道间质瘤(GIST)患者。 3. 既往接受过索拉非尼治疗的肝细胞癌(HCC)患者。
瑞戈非尼说明书
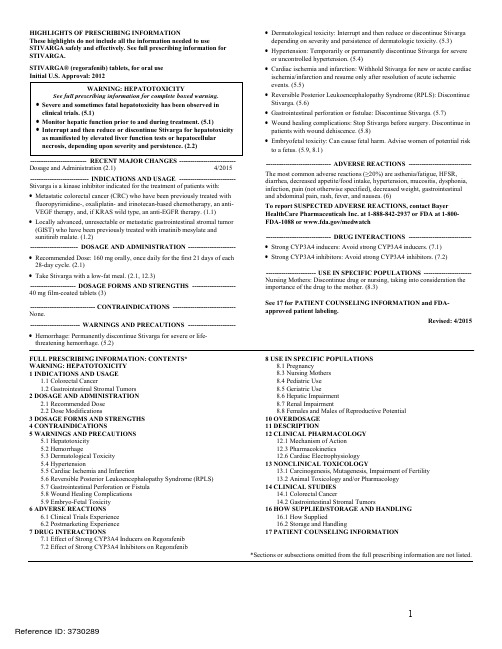
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use STIVARGA safely and effectively. See full prescribing information for STIVARGA.STIVARGA® (regorafenib) tablets, for oral useInitial U.S. Approval: 2012WARNING: HEPATOTOXICITYSee full prescribing information for complete boxed warning.∙Severe and sometimes fatal hepatotoxicity has been observed inclinical trials. (5.1)∙Monitor hepatic function prior to and during treatment. (5.1)∙Interrupt and then reduce or discontinue Stivarga for hepatotoxicity as manifested by elevated liver function tests or hepatocellularnecrosis, depending upon severity and persistence. (2.2)-------------------------- RECENT MAJOR CHANGES --------------------------Dosage and Administration (2.1) 4/2015 --------------------------- INDICATIONS AND USAGE --------------------------Stivarga is a kinase inhibitor indicated for the treatment of patients with:∙Metastatic colorectal cancer (CRC) who have been previously treated with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy, an anti-VEGF therapy, and, if KRAS wild type, an anti-EGFR therapy. (1.1)∙Locally advanced, unresectable or metastatic gastrointestinal stromal tumor (GIST) who have been previously treated with imatinib mesylate and sunitinib malate. (1.2)----------------------DOSAGE AND ADMINISTRATION ---------------------- ∙Recommended Dose: 160 mg orally, once daily for the first 21 days of each 28-day cycle. (2.1)∙Take Stivarga with a low-fat meal. (2.1, 12.3)--------------------- DOSAGE FORMS AND STRENGTHS --------------------40 mg film-coated tablets (3)------------------------------ CONTRAINDICATIONS -----------------------------None.----------------------- WARNINGS AND PRECAUTIONS ----------------------∙Hemorrhage: Permanently discontinue Stivarga for severe or life-threatening hemorrhage. (5.2) ∙Dermatological toxicity: Interrupt and then reduce or discontinue Stivarga depending on severity and persistence of dermatologic toxicity. (5.3)∙Hypertension: Temporarily or permanently discontinue Stivarga for severe or uncontrolled hypertension. (5.4)∙Cardiac ischemia and infarction: Withhold Stivarga for new or acute cardiac ischemia/infarction and resume only after resolution of acute ischemic events. (5.5)∙Reversible Posterior Leukoencephalopathy Syndrome (RPLS): Discontinue Stivarga. (5.6)∙Gastrointestinal perforation or fistulae: Discontinue Stivarga. (5.7)∙Wound healing complications: Stop Stivarga before surgery. Discontinue in patients with wound dehiscence. (5.8)∙Embryofetal toxicity: Can cause fetal harm. Advise women of potential risk to a fetus. (5.9, 8.1)------------------------------ ADVERSE REACTIONS -----------------------------The most common adverse reactions (≥20%) are asthenia/fatigue, HFSR, diarrhea, decreased appetite/food intake, hypertension, mucositis, dysphonia, infection, pain (not otherwise specified), decreased weight, gastrointestinal and abdominal pain, rash, fever, and nausea. (6)To report SUSPECTED ADVERSE REACTIONS, contact Bayer HealthCare Pharmaceuticals Inc. at 1-888-842-2937 or FDA at 1-800FDA-1088 or /medwatch------------------------------ DRUG INTERACTIONS -----------------------------∙Strong CYP3A4 inducers: Avoid strong CYP3A4 inducers. (7.1)∙Strong CYP3A4 inhibitors: Avoid strong CYP3A4 inhibitors. (7.2)----------------------- USE IN SPECIFIC POPULATIONS ----------------------Nursing Mothers: Discontinue drug or nursing, taking into consideration the importance of the drug to the mother. (8.3)See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.Revised: 4/2015FULL PRESCRIBING INFORMATION: CONTENTS* WARNING: HEPATOTOXICITY1 INDICATIONS AND USAGE1.1 Colorectal Cancer1.2 Gastrointestinal Stromal Tumors2 DOSAGE AND ADMINISTRATION2.1 Recommended Dose2.2 Dose Modifications3 DOSAGE FORMS AND STRENGTHS4 CONTRAINDICATIONS5 WARNINGS AND PRECAUTIONS5.1 Hepatotoxicity5.2 Hemorrhage5.3 Dermatological Toxicity5.4 Hypertension5.5 Cardiac Ischemia and Infarction5.6 Reversible Posterior Leukoencephalopathy Syndrome (RPLS)5.7 Gastrointestinal Perforation or Fistula5.8 Wound Healing Complications5.9 Embryo-Fetal Toxicity6 ADVERSE REACTIONS6.1 Clinical Trials Experience6.2 Postmarketing Experience7 DRUG INTERACTIONS7.1 Effect of Strong CYP3A4 Inducers on Regorafenib7.2 Effect of Strong CYP3A4 Inhibitors on Regorafenib8 USE IN SPECIFIC POPULATIONS8.1 Pregnancy8.3 Nursing Mothers8.4 Pediatric Use8.5 Geriatric Use8.6 Hepatic Impairment8.7 Renal Impairment8.8 Females and Males of Reproductive Potential10 OVERDOSAGE11 DESCRIPTION12 CLINICAL PHARMACOLOGY12.1 Mechanism of Action12.3 Pharmacokinetics12.6 Cardiac Electrophysiology13 NONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility13.2 Animal Toxicology and/or Pharmacology14 CLINICAL STUDIES14.1 Colorectal Cancer14.2 Gastrointestinal Stromal Tumors16 HOW SUPPLIED/STORAGE AND HANDLING16.1 How Supplied16.2 Storage and Handling17 PATIENT COUNSELING INFORMATION*Sections or subsections omitted from the full prescribing information are not listed.FULL PRESCRIBING INFORMATIONWARNING: HEPATOTOXICITY∙Severe and sometimes fatal hepatotoxicity has been observed in clinical trials [see Warnings and Precautions(5.1)].∙ Monitor hepatic function prior to and during treatment [see Warnings and Precautions (5.1)].∙ Interrupt and then reduce or discontinue Stivarga for hepatotoxicity as manifested by elevated liver function tests or hepatocellular necrosis, depending upon severity and persistence [see Dosage and Administration (2.2)].1 INDICATIONS AND USAGE1.1 Colorectal CancerStivarga® is indicated for the treatment of patients with metastatic colorectal cancer (CRC) who have been previously treated with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy, an anti-VEGF therapy, and, if KRAS wild type, an anti-EGFR therapy.1.2 Gastrointestinal Stromal TumorsStivarga is indicated for the treatment of patients with locally advanced, unresectable or metastatic gastrointestinal stromal tumor (GIST) who have been previously treated with imatinib mesylate and sunitinib malate.2 DOSAGE AND ADMINISTRATION2.1 Recommended DoseThe recommended dose is 160 mg regorafenib (four 40 mg tablets) taken orally once daily for the first 21 days of each 28day cycle. Continue treatment until disease progression or unacceptable toxicity.Take Stivarga at the same time each day. Swallow tablet whole with water after a low-fat meal that contains less than 600 calories and less than 30% fat [see Clinical Pharmacology (12.3)]. Do not take two doses of Stivarga on the same day to make up for a missed dose from the previous day.2.2 Dose ModificationsInterrupt Stivarga for the following:∙ NCI CTCAE Grade 2 hand-foot skin reaction (HFSR) [palmar-plantar erythrodysesthesia (PPE)] that is recurrent or does not improve within 7 days despite dose reduction; interrupt therapy for a minimum of 7 days for Grade 3 HFSR ∙ Symptomatic Grade 2 hypertension∙ Any NCI CTCAE Grade 3 or 4 adverse reactionReduce the dose of Stivarga to 120 mg:∙ For the first occurrence of Grade 2 HFSR of any duration∙ After recovery of any Grade 3 or 4 adverse reaction∙ For Grade 3 aspartate aminotransferase (AST)/alanine aminotransferase (ALT) elevation; only resume if the potential benefit outweighs the risk of hepatotoxicityReduce the dose of Stivarga to 80 mg:∙For re-occurrence of Grade 2 HFSR at the 120 mg dose∙After recovery of any Grade 3 or 4 adverse reaction at the 120 mg dose (except hepatotoxicity)Discontinue Stivarga permanently for the following:∙Failure to tolerate 80 mg dose∙Any occurrence of AST or ALT more than 20 times the upper limit of normal (ULN)∙Any occurrence of AST or ALT more than 3 times ULN with concurrent bilirubin more than 2 times ULN∙Re-occurrence of AST or ALT more than 5 times ULN despite dose reduction to 120 mg∙For any Grade 4 adverse reaction; only resume if the potential benefit outweighs the risks3 DOSAGE FORMS AND STRENGTHSStivarga is a 40 mg, light pink, oval shaped, film-coated tablet, debossed with ‘BAYER’ on one side and ‘40’ on the other side.4 CONTRAINDICATIONSNone5 WARNINGS AND PRECAUTIONS5.1 HepatotoxicitySevere drug induced liver injury with fatal outcome occurred in 0.3% of 1200 Stivarga-treated patients across all clinical trials. Liver biopsy results, when available, showed hepatocyte necrosis with lymphocyte infiltration. In Study 1, fatal hepatic failure occurred in 1.6% of patients in the regorafenib arm and in 0.4% of patients in the placebo arm; all the patients with hepatic failure had metastatic disease in the liver. In Study 2, fatal hepatic failure occurred in 0.8% of patients in the regorafenib arm [see Adverse Reactions (6.1)].Obtain liver function tests (ALT, AST and bilirubin) before initiation of Stivarga and monitor at least every two weeks during the first 2 months of treatment. Thereafter, monitor monthly or more frequently as clinically indicated. Monitor liver function tests weekly in patients experiencing elevated liver function tests until improvement to less than 3 times the ULN or baseline.Temporarily hold and then reduce or permanently discontinue Stivarga depending on the severity and persistence of hepatotoxicity as manifested by elevated liver function tests or hepatocellular necrosis [see Dosage and Administration (2.2)].5.2 HemorrhageStivarga caused an increased incidence of hemorrhage. The overall incidence (Grades 1-5) was 21% and 11% in Stivargatreated patients compared to 8% and 3% in placebo-treated patients in Studies 1 and 2. Fatal hemorrhage occurred in 4 of 632 (0.6%) of Stivarga-treated patients in Studies 1 and 2 and involved the respiratory, gastrointestinal, or genitourinary tracts.Permanently discontinue Stivarga in patients with severe or life-threatening hemorrhage. Monitor INR levels more frequently in patients receiving warfarin [see Clinical Pharmacology (12.3)].5.3 Dermatological ToxicityStivarga caused increased incidences of adverse reactions involving the skin and subcutaneous tissues (72% versus 24% in Study 1 and 78% versus 24% in Study 2), including hand-foot skin reaction (HFSR) also known as palmar-plantar erythrodysesthesia (PPE), and severe rash requiring dose modification.The overall incidence of HFSR was higher in Stivarga-treated patients, (45% versus 7% in Study 1 and 67% versus 12% in Study 2), than in the placebo-treated patients. Most cases of HFSR in Stivarga-treated patients appeared during the first cycle of treatment (69% and 71% of patients who developed HFSR in Study 1 and Study 2, respectively). The incidence of Grade 3 HFSR (17% versus 0% in Study 1 and 22% versus 0% in Study 2), Grade 3 rash (6% versus <1% in Study 1 and 7% versus 0% in Study 2), serious adverse reactions of erythema multiforme (0.2% vs. 0% in Study 1) and Stevens Johnson Syndrome (0.2% vs. 0% in Study 1) was higher in Stivarga-treated patients [see Adverse Reactions (6.1)].Toxic epidermal necrolysis occurred in 0.17% of 1200 Stivarga-treated patients across all clinical trials.Withhold Stivarga, reduce the dose, or permanently discontinue Stivarga depending on the severity and persistence of dermatologic toxicity [see Dosage and Administration (2.2)]. Institute supportive measures for symptomatic relief.5.4 HypertensionStivarga caused an increased incidence of hypertension (30% versus 8% in Study 1 and 59% versus 27% in Study 2) [see Adverse Reactions (6.1)]. Hypertensive crisis occurred in 0.25% of 1200 Stivarga-treated patients across all clinical trials. The onset of hypertension occurred during the first cycle of treatment in most patients who developed hypertension (72% in Study 1 and Study 2).Do not initiate Stivarga unless blood pressure is adequately controlled. Monitor blood pressure weekly for the first 6 weeks of treatment and then every cycle, or more frequently, as clinically indicated. Temporarily or permanently withhold Stivarga for severe or uncontrolled hypertension [see Dosage and Administration (2.2)].5.5 Cardiac Ischemia and InfarctionStivarga increased the incidence of myocardial ischemia and infarction in Study 1 (1.2% versus 0.4%) [see Adverse Reactions (6.1)]. Withhold Stivarga in patients who develop new or acute onset cardiac ischemia or infarction. Resume Stivarga only after resolution of acute cardiac ischemic events, if the potential benefits outweigh the risks of further cardiac ischemia.5.6 Reversible Posterior Leukoencephalopathy Syndrome (RPLS)Reversible Posterior Leukoencephalopathy Syndrome (RPLS), a syndrome of subcortical vasogenic edema diagnosed by characteristic finding on MRI, occurred in one of 1200 Stivarga-treated patients across all clinical trials. Perform an evaluation for RPLS in any patient presenting with seizures, headache, visual disturbances, confusion or altered mental function. Discontinue Stivarga in patients who develop RPLS.5.7 Gastrointestinal Perforation or FistulaGastrointestinal perforation or fistula occurred in 0.6% of 1200 patients treated with Stivarga across all clinical trials; this included four fatal events. In Study 2, 2.1% (4/188) of Stivarga-treated patients who were treated during the blinded or open-label portion of the study developed gastrointestinal fistula or perforation; of these, two cases of gastrointestinal perforation were fatal. Permanently discontinue Stivarga in patients who develop gastrointestinal perforation or fistula.5.8 Wound Healing ComplicationsNo formal studies of the effect of regorafenib on wound healing have been conducted. Since vascular endothelial growth factor receptor (VEGFR) inhibitors such as regorafenib can impair wound healing, treatment with regorafenib should be stopped at least 2 weeks prior to scheduled surgery. The decision to resume regorafenib after surgery should be based on clinical judgment of adequate wound healing. Regorafenib should be discontinued in patients with wound dehiscence. 5.9 Embryo-Fetal ToxicityStivarga can cause fetal harm when administered to a pregnant woman. Regorafenib was embryolethal and teratogenic in rats and rabbits at exposures lower than human exposures at the recommended dose, with increased incidences of cardiovascular, genitourinary, and skeletal malformations. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1)].6 ADVERSE REACTIONSThe following serious adverse reactions are discussed elsewhere in the labeling:∙Hepatotoxicity [See Warnings and Precautions (5.1)]∙Hemorrhage [See Warnings and Precautions (5.2)]∙Dermatological Toxicity [See Warnings and Precautions (5.3)]∙Hypertension [See Warnings and Precautions (5.4)]∙Cardiac Ischemia and Infarction [See Warnings and Precautions (5.5)]∙Reversible Posterior Leukoencephalopathy Syndrome (RPLS) [See Warnings and Precautions (5.6)]∙Gastrointestinal Perforation or Fistula [See Warnings and Precautions (5.7)]Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rate observed in practice.The most frequently observed adverse drug reactions (≥20%) in patients receiving Stivarga are asthenia/fatigue, HFSR, diarrhea, decreased appetite/food intake, hypertension, mucositis, dysphonia, infection, pain (not otherwise specified), decreased weight, gastrointestinal and abdominal pain, rash, fever, and nausea.The most serious adverse drug reactions in patients receiving Stivarga are hepatotoxicity, hemorrhage, and gastrointestinal perforation.6.1 Clinical Trials ExperienceColorectal CancerThe safety data described below, except where noted, are derived from a randomized (2:1), double-blind, placebo-controlled trial (Study 1) in which 500 patients (median age 61 years; 61% men) with previously-treated metastatic colorectal cancer received Stivarga as a single agent at the dose of 160 mg daily for the first 3 weeks of each 4 week treatment cycle and 253 patients (median age 61 years; 60% men) received placebo. The median duration of therapy was 7.3 (range 0.3, 47.0) weeks for patients receiving Stivarga. Due to adverse reactions, 61% of the patients receiving Stivarga required a dose interruption and 38% of the patients had their dose reduced. Drug-related adverse reactions that resulted in treatment discontinuation were reported in 8.2% of Stivarga-treated patients compared to 1.2% of patients whoreceived placebo. Hand-foot skin reaction (HFSR) and rash were the most common reasons for permanent discontinuation of Stivarga.Table 1 compares the incidence of adverse reactions (≥10%) in patients receiving Stivarga and reported more commonly than in patients receiving placebo (Study 1).Table 1 Adverse drug reactions (≥10%) reported in patients treated with Stivarga in Study 1 and reported more commonly than in patients receiving placeboAdverse ReactionsStivarga(N=500)Placebo(N=253) Grade GradeAll%≥ 3%All%≥ 3%General disorders and administration site conditionsAsthenia/fatigue PainFever 642928153246211592Metabolism and nutrition disordersDecreased appetite and food intake 47 5 28 4Skin and subcutaneous tissue disorders HFSR/PPERash a 452617674<1Gastrointestinal disorders DiarrheaMucositis 4333841752InvestigationsWeight loss 32 <1 10 0 Infections and infestationsInfection 31 9 17 6 Vascular disordersHypertension Hemorrhage b 30218288<1<1Respiratory, thoracic and mediastinaldisordersDysphonia 30 0 6 0Nervous system disordersHeadache 10<170 amaculo-papular rash, papular rash, and pruritic rash.b Fatal outcomes observed.Laboratory AbnormalitiesLaboratory abnormalities observed in Study 1 are shown in Table 2. Table 2 Laboratory test abnormalities reported in Study 1 Laboratory Parameter Stivarga (N=500 a) Placebo(N=253 a )Grade b Grade b All %3 %4 %All %3 %4 %Blood and lymphatic systemdisordersAnemia 79 5 1 66 3 0Thrombocytopenia 41 2 <1 17 <1 0 Neutropenia 3 1 0 0 0 0 Lymphopenia 54 9 0 34 3 0 Metabolism and nutrition disorders Hypocalcemia 59 1 <1 18 1 0 Hypokalemia 26 4 0 8 <1 0 Hyponatremia30 7 1 22 4 0 Hypophosphatemia 57 31 1 11 4 0 Hepatobiliary disordersHyperbilirubinemia 45 10 3 17 5 3 Increased AST 65 5 1 46 4 1 Increased ALT 45 5 1 30 3 <1 Renal and urinary disordersProteinuria 60 <1 0 34 <1 0 InvestigationsIncreased INR c24 4 N/A 17 2 N/AIncreased Lipase 46 9 2 19 3 2Increased Amylase 26 2 <1 17 2 <1 a% based on number of patients with post-baseline samples which may be less than 500 (regorafenib) or 253 (placebo). bCommon Terminology Criteria for Adverse Events (CTCAE), v3.0. cInternational normalized ratio: No Grade 4 denoted in CTCAE, v3.0. Gastrointestinal Stromal TumorsThe safety data described below are derived from a randomized (2:1), double-blind, placebo-controlled trial (Study 2) in which 132 patients (median age 60 years; 64% men) with previously-treated GIST received Stivarga as a single agent at a dose of 160 mg daily for the first 3 weeks of each 4 week treatment cycle and 66 patients (median age 61 years; 64% men) received placebo. The median duration of therapy was 22.9 (range 0.1, 50.9) weeks for patients receiving Stivarga. Dose interruptions for adverse events were required in 58% of patients receiving Stivarga and 50% of patients had their dose reduced. Drug-related adverse reactions that resulted in treatment discontinuation were reported in 2.3% of Stivargatreated patients compared to 1.5% of patients who received placebo.Table 3 compares the incidence of adverse reactions (≥10%) in GIST patients receiving Stivarga and reported more commonly than in patients receiving placebo (Study 2).Table 3 Adverse reactions (≥10%) reported in patients treated with Stivarga in Study 2 and reported more commonly than in patients receiving placeboAdverse ReactionsStivarga(N=132)Placebo(N=66)Grade Grade All%≥ 3%All%≥ 3%Skin and subcutaneous tissue disordersHFSR/PPE Rash a Alopecia 673024227212322General disorders and administration site conditionsAsthenia/Fatigue Fever 52214391122Vascular disordersHypertension Hemorrhage 59112842735Gastrointestinal disordersDiarrhea Mucositis Nausea Vomiting 47402017822<19812822Respiratory, thoracic and mediastinaldisordersDysphonia 3990 Infections and infestationsInfection 32550 Metabolism and nutrition disordersDecreased appetite and food intake Hypothyroidism b 3118<12163Nervous system disordersHeadache 1690 InvestigationsWeight loss 14 0 8 0Musculoskeletal and connective tissuedisordersMusculoskeletal stiffness 14 0 3 0a The term rash represents reports of events of rash, erythematous rash, macular rash, maculo-papular rash, papular rashand pruritic rash.b Hypothyroidism incidence based on subset of patients with normal TSH and no thyroid supplementation at baseline.Laboratory AbnormalitiesLaboratory abnormalities observed in Study 2 are shown in Table 4. Table 4 Laboratory test abnormalities reported in Study 2Laboratory ParameterStivarga(N=132 a)Placebo(N=66 a)Grade b Grade bAll%3%4%All%3%4%Blood and lymphaticsystem disordersThrombocytopenia 13 1 0 2 0 2 Neutropenia 16 2 0 12 3 0 Lymphopenia 30 8 0 24 3 0 Metabolism and nutritiondisordersHypocalcemia 17 2 0 5 0 0 Hypokalemia 21 3 0 3 0 0 Hypophosphatemia 55 20 2 3 2 0 Hepatobiliary disordersHyperbilirubinemia 33 3 1 12 2 0Increased AST 58 3 1 47 3 0Increased ALT 39 4 1 39 2 0Renal and urinarydisordersProteinuria 333-c 30 3 -c InvestigationsIncreasedLipase 14 0 1 5 0 0ab CTCAE, v4.0.c No Grade 4 denoted in CTCAE, v4.0.6.2 Postmarketing ExperienceThe following adverse reaction has been identified during postapproval use of Stivarga. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure:hypersensitivity reaction7 DRUG INTERACTIONS7.1 Effect of Strong CYP3A4 Inducers on RegorafenibCo-administration of a strong CYP3A4 inducer (rifampin) with a single 160 mg dose of Stivarga decreased the mean exposure of regorafenib, increased the mean exposure of the active metabolite M-5, and resulted in no change in the mean exposure of the active metabolite M-2. Avoid concomitant use of Stivarga with strong CYP3A4 inducers (e.g. rifampin, phenytoin, carbamazepine, phenobarbital, and St. John’s Wort) [see Clinical Pharmacology (12.3)].7.2 Effect of Strong CYP3A4 Inhibitors on RegorafenibCo-administration of a strong CYP3A4 inhibitor (ketoconazole) with a single 160 mg dose of Stivarga increased the mean exposure of regorafenib and decreased the mean exposure of the active metabolites M-2 and M-5. Avoid concomitant use of Stivarga with strong inhibitors of CYP3A4 activity (e.g. clarithromycin, grapefruit juice, itraconazole, ketoconazole, nefazodone, posaconazole, telithromycin, and voriconazole) [see Clinical Pharmacology (12.3)].8 USE IN SPECIFIC POPULATIONS8.1 PregnancyPregnancy Category D [see Warnings and Precautions (5.9)]Risk SummaryBased on its mechanism of action, Stivarga can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies with Stivarga in pregnant women. Regorafenib was embryolethal and teratogenic in rats and rabbits at exposures lower than human exposures at the recommended dose, with increased incidences of cardiovascular, genitourinary, and skeletal malformations. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.Animal DataIn embryo-fetal development studies, a total loss of pregnancy (100% resorption of litter) was observed in rats at doses as low as 1 mg/kg (approximately 6% of the recommended human dose, based on body surface area) and in rabbits at doses as low as 1.6 mg/kg (approximately 25% of the human exposure at the clinically recommended dose measured by AUC).In a single dose distribution study in pregnant rats, there was increased penetration of regorafenib across the blood-brain barrier in fetuses compared to dams. In a repeat dose study with daily administration of regorafenib to pregnant rats during organogenesis, findings included delayed ossification in fetuses at doses > 0.8 mg/kg (approximately 5% of the recommended human dose based on body surface area) with dose-dependent increases in skeletal malformations including cleft palate and enlarged fontanelle at doses ≥ 1 mg/kg (approximately 10% of the clinical exposure based on AUC). At doses ≥ 1.6 mg/kg (approximately 11% of the recommended human dose based on body surface area), there were dose-dependent increases in the incidence of cardiovascular malformations, external abnormalities, diaphragmatic hernia, and dilation of the renal pelvis.In pregnant rabbits administered regorafenib daily during organogenesis, there were findings of ventricular septal defects evident at the lowest tested dose of 0.4 mg/kg (approximately 7% of the AUC in patients at the recommended dose). At doses of ≥ 0.8 mg/kg (approximately 15% of the human exposure at the recommended human dose based on AUC), administration of regorafenib resulted in dose-dependent increases in the incidence of additional cardiovascular malformations and skeletal anomalies as well as significant adverse effects on the urinary system including missing kidney/ureter; small, deformed and malpositioned kidney; and hydronephrosis. The proportion of viable fetuses that were male decreased with increasing dose in two rabbit embryo-fetal toxicity studies.8.3 Nursing MothersIt is unknown whether regorafenib or its metabolites are excreted in human milk. In rats, regorafenib and its metabolites are excreted in milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Stivarga, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.8.4 Pediatric UseThe safety and efficacy of Stivarga in pediatric patients less than 18 years of age have not been established.In 28-day repeat dose studies in rats there were dose-dependent findings of dentin alteration and angiectasis. These findings were observed at regorafenib doses as low as 4 mg/kg (approximately 25% of the AUC in humans at the recommended dose). In 13-week repeat dose studies in dogs there were similar findings of dentin alteration at doses as low as 20 mg/kg (approximately 43% of the AUC in humans at the recommended dose). Administration of regorafenib in these animals also led to persistent growth and thickening of the femoral epiphyseal growth plate.8.5 Geriatric UseOf the 632 Stivarga-treated patients enrolled in Studies 1 and 2, 37% were 65 years of age and over, while 8% were 75 and over. No overall differences in safety or efficacy were observed between these patients and younger patients.8.6 Hepatic ImpairmentStivarga is eliminated mainly via the hepatic route. No clinically important differences in the mean exposure of regorafenib or the active metabolites M-2 and M-5 were observed in patients with hepatocellular carcinoma and mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment compared to patients with normal hepatic function [see Clinical Pharmacology (12.3)]. No dose adjustment is recommended in patients with mild or moderate hepatic impairment. Closely monitor patients with hepatic impairment for adverse reactions [see Warnings and Precautions (5.1)].Stivarga is not recommended for use in patients with severe hepatic impairment (Child-Pugh Class C), as it has not been studied in this population.8.7 Renal ImpairmentNo clinically relevant differences in the mean exposure of regorafenib and the active metabolites M-2 and M-5 were observed in patients with mild renal impairment (CLcr 60-89 mL/min) compared to patients with normal renal function following regorafenib 160 mg daily for 21 days [see Clinical Pharmacology (12.3)]. No dose adjustment is recommended for patients with mild renal impairment. Limited pharmacokinetic data are available from patients with moderate renal impairment (CLcr 30-59 mL/min). Stivarga has not been studied in patients with severe renal impairment or end-stage renal disease.8.8 Females and Males of Reproductive PotentialContraceptionUse effective contraception during treatment and up to 2 months after completion of therapy.InfertilityThere are no data on the effect of Stivarga on human fertility. Results from animal studies indicate that regorafenib can impair male and female fertility [see Nonclinical Toxicology (13.1)].10 OVERDOSAGEThe highest dose of Stivarga studied clinically is 220 mg per day. In the event of suspected overdose, interrupt Stivarga, institute supportive care, and observe until clinical stabilization.。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
【用法用量】
(1)推荐剂量:160 mg口服.每天1次每28天疗程的头21天.
(2)与食物服用Stivarga(一种低脂肪早餐).
【不良反应】最常见不良反应(≥30%)是乏力/疲乏.减低食欲和食物摄入量.手足皮肤反应(HFSR) [掌足红肿(PPE)].腹泻.口腔粘膜炎.体重减轻.感染.高血压.和发音困难.
(5)可逆性后部白质脑病综合征(RPLS):终止Stivarga.
(6)胃肠道穿孔或瘘管:终止Stivarga.
(7)伤口愈合并发症:瑞格非尼片哪里卖术前停止Stivarga.在伤口裂开患者中终止.
(8)胚胎胎儿毒性:可能致胎儿危害.劝告妇女对胎儿潜在风险.
【规格】40mg.28片/盒.
【贮藏】遮光.密封保存.
Stivarga价格瑞戈非尼片价格瑞戈非尼片说明书名称】Stivarga
【通用名称】瑞戈非尼片
【英文名称】regorafenib
【汉语拼音】Ruigefeinipian
【产品价格】40mg×28片×3瓶:30000元/盒
【适应症】Stivarga是一种激酶抑制剂适用于既往曾用基于氟嘧啶.奥沙利铂-和伊立替康化疗.一种抗-VEGF治疗.和.如KRAS野生型.一种抗-EGFR治疗过的转移结肠直肠癌(CRC)患者的治疗.
【注意事项】
(1)出血:对严重或威胁生命出血永久终止Stivarga.
(2)皮肤学毒性:瑞格非尼片价格中断和然后减低或终止Stivarga取决于皮肤学毒性的严重程度和持久性.
(3)高血压:对严重或不能控制的高血压暂时或永久终止Stivarga.
(4)心脏缺血和梗死:拒给Stivarga对新或急性心脏缺血/梗死和只有急性缺血事件解决后恢复.
