医学英语口语:英文病历
医学英语阅读:英文病历
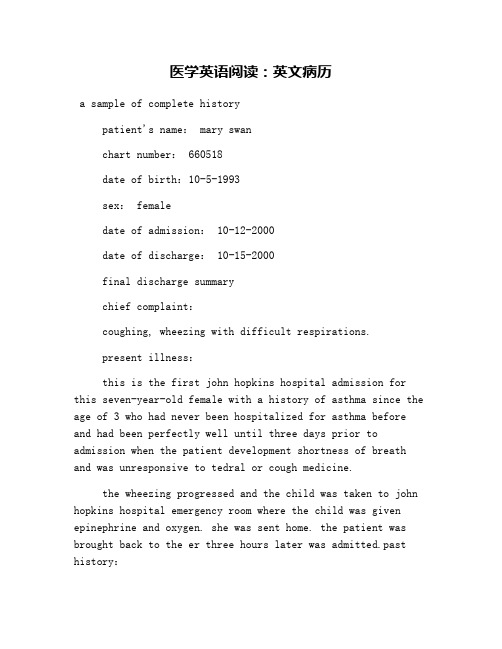
医学英语阅读:英文病历a sample of complete historypatient's name: mary swanchart number: 660518date of birth:10-5-1993sex: femaledate of admission: 10-12-2000date of discharge: 10-15-2000final discharge summarychief complaint:coughing, wheezing with difficult respirations.present illness:this is the first john hopkins hospital admission for this seven-year-old female with a history of asthma since the age of 3 who had never been hospitalized for asthma before and had been perfectly well until three days prior to admission when the patient development shortness of breath and was unresponsive to tedral or cough medicine.the wheezing progressed and the child was taken to john hopkins hospital emergency room where the child was given epinephrine and oxygen. she was sent home. the patient was brought back to the er three hours later was admitted.past history:the child was a product of an 8.5-month gestation. the mother had toxemia of pregnancy. immunizations: all. feeding:good. allergies: chocolate, dog hair, tomatoes.family history:the mother is 37, alive and well. the father is 45,alive and well. two sibs, one brother and one sister, alive and well. the family was not positive for asthma, diabetes, etc.review of systems:negative except for occasional conjunctivitis and asthma.physical examination on admission:the physical examination revealed a well-developed and well-nourished female, age 7, with a pulse of 96, respiratory rate of 42 and t emperature of 101.0℉. she was in a mist tent at the time of examination.funduscopic examination revealed normal fundi with flat discs. nose and throat were somewhat injected, particularlythe posterior pharynx. the carotids were palpable and equal. ears were clear. thyroid not palpable. the examination of the chest revealed bilateral inspiratory and expiratory wheezes. breath sounds were decreased in the left anterior lung field. the heart was normal. abdomen was soft and symmetrical, no palpable liver, kidney, or spleen. the bowel sounds were normal. pelvic: normal female child. rectal deferred. extremities negative.impression:bronchial asthma, and pharyngitis.laboratory data:the white count on admission was 13,600 with hgb of 13.0. differential revealed 64 segs and 35 lymphs with 3 eos. adequate platelets. sputum culture and sensitivity revealed alpha hemolytic streptococcus sensitive to penicillin. chestx-ray on admission showed hyperaeration and prominent bronchovascular markings. the child was started on procaine penicillin 600,000 unites im q.d in accordance with theculture and sensitivity of the sputum.hospital course:。
医学英语病历范文
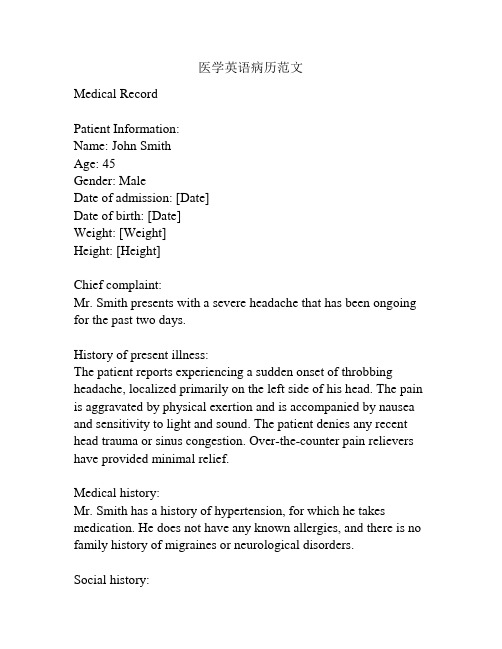
医学英语病历范文Medical RecordPatient Information:Name: John SmithAge: 45Gender: MaleDate of admission: [Date]Date of birth: [Date]Weight: [Weight]Height: [Height]Chief complaint:Mr. Smith presents with a severe headache that has been ongoing for the past two days.History of present illness:The patient reports experiencing a sudden onset of throbbing headache, localized primarily on the left side of his head. The pain is aggravated by physical exertion and is accompanied by nausea and sensitivity to light and sound. The patient denies any recent head trauma or sinus congestion. Over-the-counter pain relievers have provided minimal relief.Medical history:Mr. Smith has a history of hypertension, for which he takes medication. He does not have any known allergies, and there is no family history of migraines or neurological disorders.Social history:The patient is a smoker, consuming approximately 10 cigarettes per day. He drinks alcohol in moderation, primarily on social occasions. He denies any illicit drug use. His occupation involves long hours of computer work.Physical examination:On examination, the patient appears to be in mild distress due to the headache. His vital signs are within normal limits. Neurological examination reveals no focal deficits, and his cranial nerves appear to be intact. There is no evidence of meningeal irritation. His neck is supple, and there is no nuchal rigidity. The remainder of the physical examination is unremarkable. Laboratory tests:Blood tests, including a complete blood count and comprehensive metabolic panel, were performed. All results were within normal limits.Imaging studies:A brain MRI was ordered to rule out any structural abnormalities. The scan revealed no evidence of intracranial hemorrhage, mass, or other abnormalities.Assessment and plan:Mr. Smith is presenting with a severe headache consistent with a migraine without aura. He will be prescribed a triptan medication for acute management of his headache. He will also be counseled on lifestyle modifications, including smoking cessation and stress reduction techniques. A follow-up appointment will be scheduled in two weeks to evaluate the effectiveness of the treatment plan.Additionally, the patient is advised to seek immediate medical attention if his symptoms worsen or if he develops any new neurological symptoms.Signature: [Physician's Name]Date: [Date]。
soap英文病历

soap英文病历Patient Name: James SmithAge: 45Gender: MaleNationality: AmericanChief Complaint:The patient presents with a persistent rash on his arms and legs, accompanied by itching. He states that the rash appeared suddenly and has been present for the past two weeks. The patient is seeking medical attention to determine the cause and appropriate treatment for his condition.Medical History:The patient has a history of allergies, specifically to dust mites and pollen. He has not experienced any previous skin conditions or rashes. The patient is not currently taking any medications and has no known drug allergies.Present Illness:The patient reports that the rash initially started as small, red bumps on his arms and legs. Over time, the bumps have increased in size and have become itchy. He denies any associated symptoms, such as fever, fatigue, or joint pain. The patient has used over-the-counter hydrocortisone cream for itch relief, but it has provided only temporary relief.Physical Examination:On examination, the patient has multiple erythematous patches with raised edges on his arms and legs. The affected areas appear dry and slightly scaly. There are no signs of oozing or crusting. The rash is symmetrical and does not extend to the trunk or face. There is no lymphadenopathy or other abnormal findings on examination.Differential Diagnosis:1. Contact dermatitis: Contact with an irritant or allergen may cause a localized rash with itching and erythema.2. Atopic dermatitis: Chronic inflammatory skin condition characterized by itching, redness, and dryness of the skin.3. Psoriasis: Autoimmune disorder causing thick, scaly patches on the skin.4. Scabies: Infestation of the skin by microscopic mites causing intense itching and a characteristic rash.Investigations:1. Skin scraping and microscopic examination: To rule out scabies infestation.2. Allergy testing: To determine if the rash is related to an allergic reaction.Treatment Plan:1. Topical steroid cream: Prescribe a stronger topical steroid cream to reduce inflammation and relieve itching. Instruct the patient to apply a thin layer to the affected areas twice daily for two weeks.2. Moisturizers: Recommend using non-fragrance, hypoallergenic moisturizers to keep the skin hydrated and prevent dryness.3. Avoid triggers: Advise the patient to avoid known allergens or irritants that may exacerbate the rash.4. Follow-up: Schedule a follow-up appointment in two weeks to evaluate the effectiveness of the treatment and make any necessary adjustments.Patient Education:1. Review proper application of the topical steroid cream and discuss potential side effects, such as skin thinning and discoloration.2. Emphasize the importance of avoiding scratching to prevent infection and further skin damage.3. Discuss the potential triggers for allergic reactions and provide recommendations for allergen avoidance, such as using fragrance-free products and washing clothes with mild detergents.Prognosis:With appropriate treatment and adherence to the prescribed regimen, the prognosis for this patient is good. The symptoms should improve within two weeks with resolution of the rash and relief from itching. However, it is important to monitor the patient for any signs of exacerbation or recurrence.。
英语病历范文
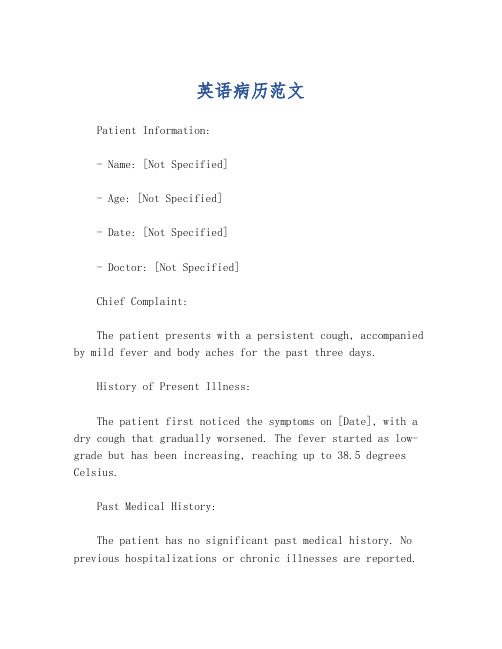
英语病历范文Patient Information:- Name: [Not Specified]- Age: [Not Specified]- Date: [Not Specified]- Doctor: [Not Specified]Chief Complaint:The patient presents with a persistent cough, accompanied by mild fever and body aches for the past three days.History of Present Illness:The patient first noticed the symptoms on [Date], with a dry cough that gradually worsened. The fever started as low-grade but has been increasing, reaching up to 38.5 degrees Celsius.Past Medical History:The patient has no significant past medical history. No previous hospitalizations or chronic illnesses are reported.Medications:The patient has not taken any medications for the current illness, nor are they on any regular medication.Allergies:No known allergies to medications or environmental factors.Physical Examination:Vital signs: Temperature 38.3°C, Puls e 92 bpm, Respiratory rate 20 breaths per minute, Blood pressure 120/80 mmHg. The patient appears fatigued but in no acute distress. Lungs are clear to auscultation with no wheezing or crackles. The throat is slightly red without exudates.Assessment:Based on the symptoms and physical examination, the patient is likely suffering from a viral upper respiratory infection.Plan:1. Hydration and rest are recommended.2. Over-the-counter fever reducers and cough suppressants may be used as needed for symptomatic relief.3. If symptoms persist or worsen, the patient should return for further evaluation and potential testing for influenza or COVID-19.Follow-up:The patient is advised to follow up in one week if symptoms have not improved or if new symptoms develop.Instructions:- Increase fluid intake to prevent dehydration.- Avoid contact with others to prevent the spread of the infection.- Monitor for signs of worsening condition, such as difficulty breathing, persistent high fever, or chest pain.Note: This is a hypothetical patient case and should not be used as a substitute for professional medical advice, diagnosis, or treatment.。
医学英语-英文病例-范文

医学英语-英文病例-范文Case HistoryName: Meretrix Gender: FemaleAge: 40 Occupation: NurseBirth Place: Washington DC Marital Status: MarriedAddress: #112, Main Avenue, Washington DCReliability: Reliable Supplier: Patient herselfDate of Admission: 10am, Aug. 6th, 2006Date of Record: Aug. 6th, 2006C.C.:Palpitation and breathlessness after exertion for 7 years; edema of lower extremities for 4 daysH.P.I.:The patient got palpitation and breathlessness after overexertion and going upstairs alleviating after having a rest 7 years ago. Then she saw her doctor, and the roentgenography showed an enlargement of the heart; but it was so negligible that she was not treated. She came to Washington 5 years ago because of frequent bad colds due to bad weather conditions with strong cough which didn’t ameliorate with the disappearance of the palpitation and breathlessness but with orthopnea at night. She was once hospitalized with an injection of penicillin and glucose and had a rest of 2 weeks, thus propelling the symptoms. She complains of a flatulence without edema of lower extremities in the recent 2 years. One month ago, she was admitted to our hospital with sore throat, cough, hemoptysis, palpitation, breathlessness, and orthopnea due to a bad cold resulting from exhaustion. Antitussive and penicillin have been employed but it was in vain. Edema of lowerextremities came into being in the recent 3 days or so; urine is little with a dark color; feces are not amorphous with once a day; dyspepsia and nausea are overt. Digitalis has not been used and good in mental status with infrequent insomnia.P.H.:The patient has been and is weak with frequent sore throat since her childhood. Shegot malaria 11 years ago with a medication of quinine and thus symptoms disappeared a week after with a recurrence and a similar treatment resulting in good outcome; no migrant rash was found. No histories of allergy to drug or food, of trauma or surgery, of blood transfusion. And we are not informed of a history of inoculation.Pers. H.:The patient was a Shanghaier and came to Washington DC 5 years ago. No visiting history to other places. She was an undergraduate. The patient is a housewife with a gasto of reading. She is quiet and not addicted to smoke or wine. SheF.H.:She married at the age of 24 and her husband is 39 now. Parents, a girl aged 10, and a boy aged 6 are all living and well.Mens. H.:614——4028P.E.:T. 38.0℃. P. 70. R. 30. B.P. 100/70mmHg.The patient stayed in bed in semi-reclining position. She looked actually ill, but remained conscious, and was well oriented to time, place, and person.Skin and Lymph Node: N.A.D. (No abnormality detected.)Head: There was flaring of the nares, but otherwise normal.Neck: Negative.Chest: Excursion decreased on the right side of the chest. Trachea in the midline. Heart: Disseminated rales in the fundi of the two lungs, especially the right lung. Lungs: Slightly increased fremitus, dull percussion note, diminished breath sound, and fine moist inspiratory rales were present on the right bases. The rest of the chest showed nothing special.Abdomen: Soft. Liver felt 1.5 cm below L.C.M. (lower costal margin) on the mid-clavicular line. Spleen not felt. Murphy’s sign weakly positive, withno palpable gall-bladder. No tenderness or mass elsewhere.Spine, Extremities, Rectum and External Genitalia: Nothing remarkable. Neurological Reflexes: Physiological reflexes normal. No pathological reflexes elicited. O.P.D. Lab. Findings (Out-Patient Department Laboratory Findings):Blood:W.B.C. 14,000/cmmD.B.C. P.M.N.82%, Lymph. 16%, M.1%R.B.C. 3,900,000/cmmHgb. 11 gmFeces:Dark yellow, slightly cloudy, acidic.Density 1.019Protein (+)Glucose (-)W.B.C. 5/HPMajor Diagnostic Evidence:1.History of streptococcal infection and a weak body.2.Symptoms and signs of heart failure and pulmonary edema.3.W.B.C. of 14,000 with 82% polys.Impression:1. Rheumatic valvular disease.Mitral stenosis complicated with mitral regurgitationAtrial fibrillationGrade III heart failure2. Acute onset of a chronic tonsillitis.Date: Aug. 6th, 2006Attending Physician____________。
常用医学英语口语对话
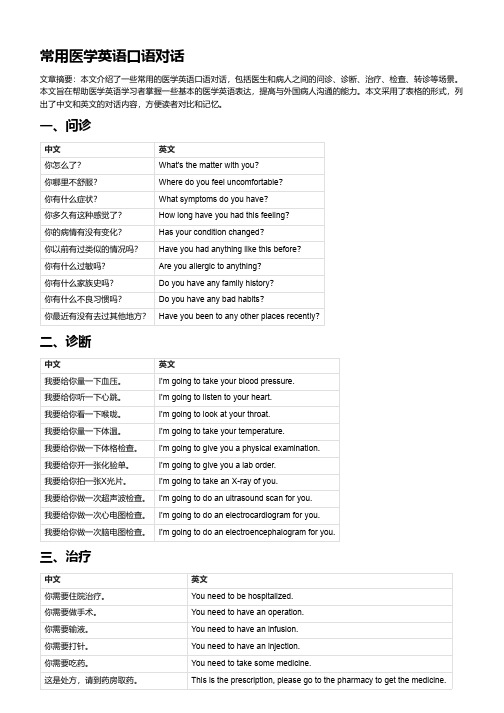
常用医学英语口语对话文章摘要:本文介绍了一些常用的医学英语口语对话,包括医生和病人之间的问诊、诊断、治疗、检查、转诊等场景。
本文旨在帮助医学英语学习者掌握一些基本的医学英语表达,提高与外国病人沟通的能力。
本文采用了表格的形式,列出了中文和英文的对话内容,方便读者对比和记忆。
一、问诊中文英文你怎么了?What's the matter with you?你哪里不舒服?Where do you feel uncomfortable?你有什么症状?What symptoms do you have?你多久有这种感觉了?How long have you had this feeling?你的病情有没有变化?Has your condition changed?你以前有过类似的情况吗?Have you had anything like this before?你有什么过敏吗?Are you allergic to anything?你有什么家族史吗?Do you have any family history?你有什么不良习惯吗?Do you have any bad habits?你最近有没有去过其他地方?Have you been to any other places recently?二、诊断中文英文我要给你量一下血压。
I'm going to take your blood pressure.我要给你听一下心跳。
I'm going to listen to your heart.我要给你看一下喉咙。
I'm going to look at your throat.我要给你量一下体温。
I'm going to take your temperature.我要给你做一下体格检查。
I'm going to give you a physical examination.我要给你开一张化验单。
医学英语病历写作范文

医学英语病历写作范文Chief Complaint: Left leg pain with recent fall.History of Present Illness: The patient is a 65-year-old male who presents to the emergency department with a chief complaint of left leg pain. He states that he fell down a flight of stairs approximately 3 hours prior to presentation. He reports that he is in moderate to severe pain, which is localized to his left lower extremity. He denies any associated numbness or tingling. He has no prior history of leg pain or injury.Past Medical History: The patient has a history of hypertension, which is well-controlled with medication. He has no other significant medical history.Social History: The patient is married and has two children. He is a retired construction worker. He smokes one pack of cigarettes per day and drinks alcohol socially.Family History: The patient's father has a history of coronary artery disease. His mother has a history of Alzheimer's disease.Physical Examination:Vital signs: Blood pressure 140/80 mmHg, heart rate 80 bpm, respiratory rate 18 breaths per minute, temperature 98.6°F (37°C).General: The patient is in moderate distress due to pain. He is alert and oriented to person, place, and time.HEENT: Normocephalic and atraumatic. Pupils are equal and reactive to light. Extraocular movements are intact. No conjunctival injection or discharge. Tympanic membranes are intact and mobile.Neck: Supple with full range of motion. No masses or tenderness.Chest: Auscultation reveals clear breath soundsbilaterally. No wheezes, rales, or rhonchi.Cardiovascular: Regular rate and rhythm. No murmurs, rubs, or gallops.Abdomen: Soft and non-tender. No masses or organomegaly.Extremities: Left lower extremity: Examination reveals swelling and tenderness of the left knee. There is a palpable step-off deformity of the lateral aspect of theleft knee. Active and passive range of motion is limiteddue to pain. Distal pulses are palpable and capillaryrefill is brisk. Sensation is intact. Right lower extremity: Examination reveals no abnormalities.Neurological Examination:Mental status: Alert and oriented to person, place,and time. No deficits in attention, memory, or language.Cranial nerves: No deficits.Motor: Strength is 5/5 in both upper and lower extremities. No atrophy or fasciculations.Sensory: Sensation is intact to light touch, pinprick, and temperature in all four extremities.Diagnostic Studies:X-ray of the left knee: The X-ray shows a displaced lateral tibial plateau fracture.Assessment:Left knee pain.Displaced lateral tibial plateau fracture.Plan:The patient will be admitted to the hospital for further evaluation and treatment.He will be placed in a knee immobilizer and will be started on pain medication.Orthopedic surgery will be consulted for further management.。
医学英语病历写作范文
医学英语病历写作范文Chief Complaint: Patient presents with chest pain and shortness of breath for 3 days.History of Present Illness: The patient, a 55-year-old male, reports experiencing sudden onset of chest pain 3 days ago. The pain is described as sharp and crushing, radiating to the left arm. He also reports associated shortness of breath and diaphoresis. The symptoms are aggravated with physical activity and alleviated with rest. There is no history of similar episodes in the past.Past Medical History: The patient has a history of hypertension and hyperlipidemia. He is on regular medications including amlodipine and atorvastatin.Family History: The patient's father had a history of myocardial infarction at the age of 60. His mother has hypertension and diabetes.Social History: The patient is a non-smoker and denies alcohol or recreational drug use. He is currently employed as a manager and reports moderate stress at work.Review of Systems: The patient denies any recent weight changes, fever, or chills. There is no history of cough, sputum production, or hemoptysis. He denies any gastrointestinal symptoms such as nausea, vomiting, or abdominal pain.Physical Examination:- Vital signs: Blood pressure 140/90 mmHg, heart rate 90 bpm, respiratory rate 20 breaths per minute, oxygen saturation 96% on room air.- General: The patient appears uncomfortable and diaphoretic.- Cardiovascular: Regular rhythm, no murmurs, rubs, or gallops. Capillary refill time is less than 2 seconds.- Respiratory: Clear breath sounds bilaterally, no wheezing or crackles.Assessment and Plan:1. Rule out acute coronary syndrome: The patient's presentation is concerning for acute coronary syndrome given the symptoms of chest pain, shortness of breath, anddiaphoresis. ECG and cardiac enzymes will be obtained to evaluate for myocardial ischemia.2. Blood pressure management: The patient's blood pressure is elevated, and optimization of antihypertensive medications will be addressed.3. Lipid management: Given the patient's history of hyperlipidemia, lipid panel will be obtained to assess for dyslipidemia and adjust medications as needed.4. Stress management: The patient's moderate stress at work will be addressed through counseling and potential referral to a stress management program.中文病历:主诉:患者因胸痛和呼吸急促已3天。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
医学英语口语:英文病历
导读:本文医学英语口语:英文病历,仅供参考,如果觉得很不错,欢迎点评和分享。
a sample of complete history
patient's name: mary swan
chart number: 660518
date of birth:10-5-1993
sex: female
date of admission: 10-12-2000
date of discharge: 10-15-2000
final discharge summary
chief complaint:
coughing, wheezing with difficult respirations.
present illness:
this is the first john hopkins hospital admission for this seven-year-old female with a history of asthma since the age of 3 who had never been hospitalized for asthma before and had been perfectly well until three days prior to admission when the patient development shortness of breath and was unresponsive to tedral or cough medicine.
the wheezing progressed and the child was taken to john hopkins hospital emergency room where the child was given epinephrine and oxygen. she was sent home. the patient was brought back to the er three hours later was admitted.past
history:
the child was a product of an 8.5-month gestation. the mother had toxemia of pregnancy. immunizations: all. feeding: good. allergies: chocolate, dog hair, tomatoes.
family history:
the mother is 37, alive and well. the father is 45, alive and well. two sibs, one brother and one sister, alive and well. the family was not positive for asthma, diabetes, etc.
review of systems:
negative except for occasional conjunctivitis and asthma.
physical examination on admission:
the physical examination revealed a well-developed and well-nourished female, age 7, with a pulse of 96, respiratory rate of 42 and temperature of 101.0℉. she was in a mist tent at the time of examination.
funduscopic examination revealed normal fundi with flat discs. nose and throat were somewhat injected, particularly the posterior pharynx. the carotids were palpable and equal. ears were clear. thyroid not palpable. the examination of the chest revealed bilateral inspiratory and expiratory wheezes. breath sounds were decreased in the left anterior lung field. the heart was normal. abdomen was soft and symmetrical, no palpable liver, kidney, or spleen. the bowel sounds were normal. pelvic: normal female child. rectal deferred. extremities negative.
impression:
bronchial asthma, and pharyngitis.
laboratory data:
the white count on admission was 13,600 with hgb of 13.0. differential revealed 64 segs and 35 lymphs with 3 eos. adequate platelets. sputum culture and sensitivity revealed alpha hemolytic streptococcus sensitive to penicillin. chest x-ray on admission showed hyperaeration and prominent bronchovascular markings. the child was started on procaine penicillin 600,000 unites im q.d in accordance with the culture and sensitivity of the sputum.
hospital course:the child was given penicillin im as stated above. ten drops of isuprel were added to the respirator every 2 hours. the patient improved steadily. she took her diet well. she was discharged on 10-15-2000 in good condition.
operation procedure: none
condition on discharge: improved
diagnosis: asthma. pharyngitis. possible right upper lobs pneumonia.
new words and expressions
wheeze vi & n. 喘息(声)
asthma n. 哮喘、气喘病
epinephrine n 肾上腺素
gestation n 妊娠
toxemia n 毒血症
allergy n 变应性、过敏症
negative a 反的、阴性的
positive a 正的、阳性的
diabetes n 糖尿病。
