2016 美国2型糖尿病综合管理方案图表
美国眼科协会临床指南:糖尿病视网膜病变
表 1 AAO 糖尿病性视网膜病变分期和国际糖尿病性 视网膜病变临床分期
表 2 国际糖尿病性黄斑水肿临床分级
表 3 尚未发生糖尿病性视网膜病变的糖尿病患者进行 眼科检查的推荐意见
指南强调了糖尿病患者早期发现视网膜病变和定期随访 的重要性,并指出眼科医生应向患者说明,即使他们没 有任何眼部症状和不适,也应当定期随诊。关于眼科检 查的时机和频率,指南给出了如下推荐(表 3):
>>>>玻璃体内注射抗 VEGF 药物被证明可以有效地 治疗累及中心的糖尿病性黄斑水肿,同时也可以作为 激光治疗 PDR 的替代方式。
>>>>目前,激光光凝仍然是不累及中心的糖尿病性 黄斑水肿的首选治疗。
2016 版 AAO 指南沿用了此前 DR 的分期,并将其和 国际糖尿病性视网膜病变临床分期一并列出(表 1)。
表 4 糖尿病患者有关视网膜病变的治疗方案推荐
一、正常或极轻度 NPDR
患者应当接受每年定期复查。一年内 5%~10% 没有 视网膜病变的患者会发展为 DR。激光治Βιβλιοθήκη 、彩色眼 底照相和 FA 并非必需。
二、轻度到中度 NPDR,不伴有黄斑水肿
已经有视网膜微动脉瘤和多发出血灶或硬性渗 出的患者应当 6~12 个月接受一次复查。约 16% 的 1 型糖尿病轻度 NPDR 患者会在 4 年 内进展到增殖期。对这部分病人,激光治疗和 FA 检查并非必要。彩色眼底照相和 OCT 检查 对了解病人的基线状况以方便复诊和患者教育 更为有利。 轻度 NPDR 的病人 4 年内发生黄斑水肿的概率 约为 12%,中度 NPDR 患者则增加到 23%。即 使无临床意义黄斑水肿病人也应在 3~4 年内 接受复查,因为发展为 CSME 的风险非常高。
2016 AACE糖尿病管理最新指南

84 ENDOCRINE PRACTICE Vol 22 No. 1 January 2016AACE/ACE Consensus StatementCONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2016 EXECUTIVE SUMMARYAlan J. Garber, MD, PhD, FACE 1; Martin J. Abrahamson, MD 2; Joshua I. Barzilay, MD, FACE 3; Lawrence Blonde, MD, FACP , FACE 4; Zachary T. Bloomgarden, MD, MACE 5; Michael A. Bush, MD 6;Samuel Dagogo-Jack, MD, DM, FRCP , FACE 7; Ralph A. DeFronzo, MD, BMS, MS, BS 8;Daniel Einhorn, MD, FACP , FACE 9; Vivian A. Fonseca, MD, FACE 10; Jeffrey R. Garber, MD, FACP , FACE 11; W. Timothy Garvey, MD, FACE 12;George Grunberger, MD, FACP , FACE 13; Yehuda Handelsman, MD, FACP , FNLA, FACE 14;Robert R. Henry, MD, FACE 15; Irl B. Hirsch, MD 16;Paul S. Jellinger, MD, MACE 17; Janet B. McGill, MD, FACE 18; Jeffrey I. Mechanick, MD, FACN, FACP , FACE, ECNU 19;Paul D. Rosenblit, MD, PhD, FNLA, FACE 20; Guillermo E. Umpierrez, MD, FACP , FACE 21From the 1Chair, Professor, Departments of Medicine, Biochemistry and Molecular Biology, and Molecular and Cellular Biology, Baylor College of Medicine, Houston, Texas, 2Beth Israel Deaconess Medical Center, Department of Medicine and Harvard Medical School, Boston, Massachusetts, 3Division of Endocrinology, Kaiser Permanente of Georgia and the Division of Endocrinology, Emory University School of Medicine, Atlanta, Georgia, 4Director, Ochsner Diabetes Clinical Research Unit, Department of Endocrinology, Diabetes and Metabolism, Ochsner Medical Center, New Orleans, Louisiana, 5Clinical Professor, Mount Sinai School of Medicine, Editor, Journal of Diabetes , New York, New York, 6Clinical Chief, Division of Endocrinology, Cedars-Sinai Medical Center, Associate Clinical Professor of Medicine, Geffen School of Medicine, UCLA, Los Angeles, California, 7A.C. Mullins Professor & Director, Division of Endocrinology, Diabetes and Metabolism, University of Tennessee Health Science Center, Memphis, Tennessee, 8Professor of Medicine, Chief, Diabetes Division, University of Texas Health Science Center at San Antonio, San Antonio, Texas, 9Immediate Past President, American College of Endocrinology, Past-President, American Association of Clinical Endocrinologists, Medical Director, Scripps Whittier Diabetes Institute, Clinical Professor of Medicine, UCSD, Associate Editor, Journal of Diabetes , Diabetes and Endocrine Associates, La Jolla, California, 10Professor of Medicine and Pharmacology, Tullis Tulane Alumni Chair in Diabetes, Chief, Section of Endocrinology, Tulane University Health Sciences Center, New Orleans, Louisiana, 11Endocrine Division, Harvard Vanguard Medical Associates, Boston, Massachusetts, Division of Endocrinology, Beth Israel Deaconess Medical Center, Boston, Massachusetts, 12Professor and Chair, Department of Nutrition Sciences, University of Alabama at Birmingham, Director, UABThis document represents the official position of the American Association of Clinical Endocrinologists and American College of Endocrinology. Where there were no randomized controlled trials or specific U.S. FDA labeling for issues in clinical practice, the participating clinical experts utilized their judgment and experience. Every effort was made to achieve consensus among the committee members. Position statements are meant to provide guidance, but they are not to be consid -ered prescriptive for any individual patient and cannot replace the judgment of a clinician.Diabetes Research Center, Mountain Brook, Alabama, 13Grunberger Diabetes Institute, Clinical Professor, Internal Medicine and Molecular Medicine & Genetics, Wayne State University School of Medicine, Bloomfield Hills, Michigan, 14Medical Director & Principal Investigator, Metabolic Institute of America, President, American College of Endocrinology, Tarzana, California, 15Professor of Medicine, University of California San Diego, Chief, Section of Diabetes, Endocrinology & Metabolism, VA San Diego Healthcare System, San Diego, California, 16Professor of Medicine, University of Washington School of Medicine, Seattle, Washington, 17Professor of Clinical Medicine, University of Miami, Miller School of Medicine, Miami, Florida, The Center for Diabetes & Endocrine Care, Hollywood, Florida, 18Professor of Medicine, Division of Endocrinology, Metabolism & Lipid Research, Washington University, St. Louis, Missouri, 19Clinical Professor of Medicine, Director, Metabolic Support, Division of Endocrinology, Diabetes, and Bone Disease, Icahn School of Medicine at Mount Sinai, New York, New York, 20Clinical Professor, Medicine, Division of Endocrinology, Diabetes, Metabolism, University California Irvine School of Medicine, Irvine, California, Co-Director, Diabetes Out-Patient Clinic, UCI Medical Center, Orange, California, Director & Principal Investigator, Diabetes/Lipid Management & Research Center, Huntington Beach, California, and 21Professor of Medicine, Emory University School of Medicine, Director, Endocrinology Section, Grady Health System, Atlanta, Georgia.Address correspondence to American Association of ClinicalEndocrinologists, 245 Riverside Avenue, Suite 200, Jacksonville, FL 32202. E-mail: publications@. DOI: 10.4158/EP151126.CSTo purchase reprints of this article, please visit: /reprints.Copyright © 2016 AACE.85Abbreviations:A1C= hemoglobin A1C; AACE= American Association of Clinical Endocrinologists; ACCORD = Action to Control Cardiovascular Risk in Diabetes; ACCORD BP= Action to Control Cardiovascular Risk in Diabetes Blood Pressure; ACEI = angiotensin-converting enzyme inhibitor; AGI = alpha-glucosidase inhibitor; apo B = apolipoprotein B; ARB = angiotensin II receptor blocker; ASCVD= atherosclerotic cardio-vascular disease; BAS = bile acid sequestrant; BMI = body mass index; BP = blood pressure; CHD = coro-nary heart disease; CKD= chronic kidney disease; CVD = cardiovascular disease; DKA = diabetic ketoac-idosis; DPP-4 = dipeptidyl peptidase 4; EPA = eicosa-pentaenoic acid; FDA = Food and Drug Administration; GLP-1= glucagon-like peptide 1; HDL-C= high-density-lipoprotein cholesterol; LDL-C = low-density-lipoprotein cholesterol; LDL-P = low-density-lipopro-tein particle; Look AHEAD = Look Action for Health in Diabetes; NPH = neutral protamine Hagedorn; OSA = obstructive sleep apnea; SFU = sulfonylurea; SGLT-2 = sodium glucose cotransporter-2; SMBG = self-moni-toring of blood glucose; T2D = type 2 diabetes; TZD = thiazolidinedioneEXECUTIVE SUMMARYThis algorithm for the comprehensive management of persons with type 2 diabetes (T2D) was developed to provide clinicians with a practical guide that considers the whole patient, their spectrum of risks and complica-tions, and evidence-based approaches to treatment. It is now clear that the progressive pancreatic beta-cell defect that drives the deterioration of metabolic control over time begins early and may be present before the diagnosis of diabetes (1). In addition to advocating glycemic control to reduce microvascular complications, this document high-lights obesity and prediabetes as underlying risk factors for the development of T2D and associated macrovascular complications. In addition, the algorithm provides recom-mendations for blood pressure (BP) and lipid control, the two most important risk factors for cardiovascular disease (CVD).Since originally drafted in 2013, the algorithm has been updated as new therapies, management approach-es, and important clinical data have emerged. The 2016 edition includes a new section on lifestyle therapy as well as discussion of all classes of obesity, antihyperglycemic, lipid-lowering, and antihypertensive medications approved by the U.S. Food and Drug Administration (FDA) through December 2015.This algorithm supplements the American Association of Clinical Endocrinologists (AACE) and A merican College of Endocrinology (ACE) 2015 Clinical Practice Guidelines for Developing a Diabetes Mellitus Comprehensive Care Plan (2) and is organized into discrete sections that address the following topics: the founding principles of the algo-rithm, lifestyle therapy, obesity, prediabetes, glucose control with noninsulin antihyperglycemic agents and insulin, management of hypertension, and management of dyslipidemia. In the accompanying algorithm, a chart summarizing the attributes of each antihyperglycemic class and the principles of the algorithm appear at the end. (Endocr Pract. 2016;22:84-113)PrinciplesThe founding principles of the Comprehensive Type 2 Diabetes Management Algorithm are as follows (see Comprehensive Type 2 Diabetes Management Algorithm—Principles):1. Lifestyle optimization is essential for all patientswith diabetes. Lifestyle optimization is multifac-eted, ongoing, and should engage the entire diabe-tes team. However, such efforts should not delayneeded pharmacotherapy, which can be initiatedsimultaneously and adjusted based on patientresponse to lifestyle efforts. The need for medicaltherapy should not be interpreted as a failure oflifestyle management, but as an adjunct to it.2. The hemoglobin A1C (A1C) target should beindividualized based on numerous factors, such asage, life expectancy, comorbid conditions, dura-tion of diabetes, risk of hypoglycemia or adverseconsequences from hypoglycemia, patient moti-vation, and adherence. An A1C level of ≤6.5% isconsidered optimal if it can be achieved in a safeand affordable manner, but higher targets maybe appropriate for certain individuals and maychange for a given individual over time.3. Glycemic control targets include fasting and post-prandial glucose as determined by self-monitor-ing of blood glucose (SMBG).4. The choice of diabetes therapies must be individu-alized based on attributes specific to both patientsand the medications themselves. Medication attri-butes that affect this choice include antihyper-glycemic efficacy, mechanism of action, risk ofinducing hypoglycemia, risk of weight gain, otheradverse effects, tolerability, ease of use, likelyadherence, cost, and safety in heart, kidney, orliver disease.5. Minimizing risk of both severe and nonseverehypoglycemia is a priority. It is a matter of safety,adherence, and cost.6. Minimizing risk of weight gain is also a priority.It too is a matter of safety, adherence, and cost.7. The initial acquisition cost of medications is onlya part of the total cost of care, which includesmonitoring requirements and risks of hypoglyce-86mia and weight gain. Safety and efficacy shouldbe given higher priority than medication cost.8. This algorithm stratifies choice of therapies basedon initial A1C level. It provides guidance as towhat therapies to initiate and add but respectsindividual circumstances that could lead to differ-ent choices.9. Combination therapy is usually required andshould involve agents with complementary mech-anisms of action.10. Comprehensive management includes lipid andBP therapies and treatment of related comorbidi-ties.11. Therapy must be evaluated frequently (e.g., every3 months) until stable using multiple criteria,including A1C, SMBG records (fasting and post-prandial), documented and suspected hypoglyce-mia events, lipid and BP values, adverse events(weight gain, fluid retention, hepatic or renalimpairment, or CVD), comorbidities, other rele-vant laboratory data, concomitant drug adminis-tration, diabetic complications, and psychosocialfactors affecting patient care. Less frequent moni-toring is acceptable once targets are achieved.12. The therapeutic regimen should be as simple aspossible to optimize adherence.13. This algorithm includes every FDA-approved classof medications for T2D (as of December 2015).Lifestyle TherapyThe key components of lifestyle therapy include medical nutrition therapy, regular physical activity, suffi-cient amounts of sleep, behavioral support, and smok-ing cessation and avoidance of all tobacco products (see Comprehensive Type 2 Diabetes Management Algorithm—Lifestyle Therapy). In the algorithm, recommendations appearing on the left apply to all patients. Patients with increasing burden of obesity or related comorbidities may also require the additional interventions listed in the middle and right side of the figure.Lifestyle therapy begins with nutrition counseling and education. All patients should strive to attain and maintain an optimal weight through a primarily plant-based diet high in polyunsaturated and monounsaturated fatty acids, with limited intake of saturated fatty acids and avoidance of trans fats. Patients who are overweight (body mass index [BMI] of 25 to 29.9 kg/m2) or obese (BMI ≥30 kg/ m2) should also restrict their caloric intake with the goal of reducing body weight by at least 5 to 10%. As shown in the Look AHEAD (Action for Health in Diabetes) and Diabetes Prevention Program studies, lowering caloric intake is the main driver for weight loss (3-6). The clini-cian or a registered dietitian (or nutritionist) should discuss recommendations in plain language at the initial visit and periodically during follow-up office visits. Discussion should focus on foods that promote health versus those that promote metabolic disease or complications and should include information on specific foods, meal plan-ning, grocery shopping, and dining-out strategies. In addi-tion, education on medical nutrition therapy for patients with diabetes should also address the need for consisten-cy in day-to-day carbohydrate intake, limiting sucrose-containing or high-glycemic-index foods, and adjusting insulin doses to match carbohydrate intake (e.g., use of carbohydrate counting with glucose monitoring) (2,7). Structured counseling (e.g., weekly or monthly sessions with a specific weight-loss curriculum) and meal replace-ment programs have been shown to be more effective than standard in-office counseling (3,6,8-15). Additional nutri-tion recommendations can be found in the 2013 Clinical Practice Guidelines for Healthy Eating for the Prevention and Treatment of Metabolic and Endocrine Diseases in Adults from AACE/ACE and The Obesity Society (16).After nutrition, physical activity is the main compo-nent in weight loss and maintenance programs. Regular physical exercise—both aerobic exercise and strength training—improves glucose control, lipid levels, and BP; decreases the risk of falls and fractures; and improves functional capacity and sense of well-being (17-24). In Look AHEAD, which had a weekly goal of ≥175 minutes per week of moderately intense activity, minutes of physi-cal activity were significantly associated with weight loss, suggesting that those who were more active lost more weight (3). The physical activity regimen should involve at least 150 minutes per week of moderate-intensity exer-cise such as brisk walking (e.g., 15- to 20-minute mile) and strength training; patients should start any new activity slowly and increase intensity and duration gradually as they become accustomed to the exercise. Structured programs can help patients learn proper technique, establish goals, and stay motivated. Patients with diabetes and/or severe obesity or complications should be evaluated for contrain-dications and/or limitations to increased physical activity, and an exercise prescription should be developed for each patient according to both goals and limitations. More detail on the benefits and risks of physical activity and the practi-cal aspects of implementing a training program in people with T2D can be found in a joint position statement from the American College of Sports Medicine and American Diabetes Association (25).Adequate rest is important for maintaining energy levels and well-being, and all patients should be advised to sleep approximately 7 hours per night. Evidence supports an association of 6 to 9 hours of sleep per night with a reduction in cardiometabolic risk factors, whereas sleep deprivation aggravates insulin resistance, hypertension, hyperglycemia, and dyslipidemia and increases inflamma-tory cytokines (26-31). Daytime drowsiness—a frequent symptom of sleep disorders such as sleep apnea—is asso-ciated with increased risk of accidents, errors in judgment,87and diminished performance (32). The most common type of sleep apnea, obstructive sleep apnea (OSA), is caused by physical obstruction of the airway during sleep. The resulting lack of oxygen causes the patient to awaken and snore, snort, and grunt throughout the night. The awaken-ings may happen hundreds of times per night, often with-out the patient’s awareness. OSA is more common in men, the elderly, and persons with obesity (33,34). Individuals with suspected OSA should be referred to a sleep specialist for evaluation and treatment (2).Behavioral support for lifestyle therapy includes the structured weight loss and physical activity programs mentioned above as well as support from family and friends. Patients should be encouraged to join commu-nity groups dedicated to a healthy lifestyle for emotional support and motivation. In addition, obesity and diabetes are associated with high rates of anxiety and depression, which can adversely affect outcomes (35,36). Healthcare professionals should assess patients’ mood and psycho-logical well-being and refer patients with mood disorders to mental healthcare professionals. Cognitive behavior-al therapy may be beneficial. A recent meta-analysis of psychosocial interventions provides insight into successful approaches (37).Smoking cessation is the final component of lifestyle therapy and involves avoidance of all tobacco products. Structured programs should be recommended for patients unable to stop smoking on their own (2).ObesityObesity is a disease with genetic, environmental, and behavioral determinants that confers increased morbidity and mortality (38,39). An evidence-based approach to the treatment of obesity incorporates lifestyle, medical, and surgical options, balances risks and benefits, and empha-sizes medical outcomes that address the complications of obesity rather than cosmetic goals. Weight loss should be considered in all overweight and obese patients with prediabetes or T2D, given the known therapeutic effects of weight loss to lower glycemia, improve the lipid profile, reduce BP, and decrease mechanical strain on the lower extremities (hips and knees) (2,38).The AACE Obesity Treatment Algorithm emphasizes a complications-centric model as opposed to a BMI-centric approach for the treatment of patients who have obesity or are overweight (see Comprehensive Type 2 Diabetes Management Algorithm—Complications-Centric Model for Care of the Overweight/Obese Patient). The patients who will benefit most from medical and surgical interven-tion have obesity-related comorbidities that can be clas-sified into 2 general categories: insulin resistance/cardio-metabolic disease and biomechanical consequences of excess body weight (40). Clinicians should evaluate and stage patients for each category. The presence and severity of complications, regardless of patient BMI, should guide treatment planning and evaluation (41,42). Once these factors are assessed, clinicians can set therapeutic goals and select appropriate types and intensities of treatment that will help patients achieve their weight-loss goals. Patients should be periodically reassessed (ideally every 3 months) to determine if targets for improvement have been reached; if not, weight loss therapy should be changed or intensi-fied. Lifestyle therapy can be recommended for all patients with overweight or obesity, and more intensive options can be prescribed for patients with comorbidities. For exam-ple, weight-loss medications can be used in combination with lifestyle therapy for all patients with a BMI ≥27 kg/ m2 and comorbidities. As of 2015, the FDA has approved 8 drugs as adjuncts to lifestyle therapy in patients with over-weight or obesity. Diethylproprion, phendimetrazine, and phentermine are approved for short-term (a few weeks) use, whereas orlistat, phentermine/topiramate extended release (ER), lorcaserin, naltrexone/bupropion, and liraglutide 3 mg may be used for long-term weight-reduction therapy. In clinical trials, the 5 drugs approved for long-term use were associated with statistically significant weight loss (placebo-adjusted decreases ranged from 2.9% with orlistat to 9.7% with phentermine/topiramate ER) after 1 year of treatment. These agents improve BP and lipids, prevent progression to diabetes during trial periods, and improve glycemic control and lipids in patients with T2D (43-60). Bariatric surgery should be considered for adult patients with a BMI ≥35 kg/ m2 and comorbidities, especially if therapeutic goals have not been reached using other modalities (2,61).PrediabetesPrediabetes reflects failing pancreatic islet beta-cell compensation for an underlying state of insulin resistance, most commonly caused by excess body weight or obesity. Current criteria for the diagnosis of prediabetes include impaired glucose tolerance, impaired fasting glucose, or metabolic syndrome (see Comprehensive Type 2 Diabetes Management Algorithm—Prediabetes Algorithm). Any one of these factors is associated with a 5-fold increase in future T2D risk (62).The primary goal of prediabetes management is weight loss. Whether achieved through lifestyle therapy, pharma-cotherapy, surgery, or some combination thereof, weight loss reduces insulin resistance and can effectively prevent progression to diabetes as well as improve plasma lipid profile and BP (44,48,49,51,53,60,63). However, weight loss may not directly address the pathogenesis of declining beta-cell function. When indicated, bariatric surgery can be highly effective in preventing progression from prediabe-tes to T2D (62).No medications (either weight loss drugs or antihy-perglycemic agents) are approved by the FDA solely for the management of prediabetes and/or the prevention of T2D. However, antihyperglycemic medications such as metformin and acarbose reduce the risk of future diabetes88in prediabetic patients by 25 to 30%. Both medications are relatively well-tolerated and safe, and they may confer a cardiovascular risk benefit (63-66). In clinical trials, thia-zolidinediones (TZDs) prevented future development of diabetes in 60 to 75% of subjects with prediabetes, but this class of drugs has been associated with a number of adverse outcomes (67-69). Glucagon-like peptide 1 (GLP-1) receptor agonists may be equally effective, as demon-strated by the profound effect of liraglutide 3 mg in safely preventing diabetes and restoring normoglycemia in the vast majority of subjects with prediabetes (59,60,70,71). However, owing to the lack of long-term safety data on the GLP-1 receptor agonists and the known adverse effects of the TZDs, these agents should be considered only for patients at the greatest risk of developing future diabetes and those failing more conventional therapies.As with diabetes, prediabetes increases the risk for atherosclerotic cardiovascular disease (ASCVD). Patients with prediabetes should be offered lifestyle therapy and pharmacotherapy to achieve lipid and BP targets that will reduce ASCVD risk.T2D PharmacotherapyIn patients with T2D, achieving the glucose target and A1C goal requires a nuanced approach that balances age, comorbidities, and hypoglycemia risk (2). The AACE supports an A1C goal of ≤6.5% for most patients and a goal of >6.5% (up to 8%; see below) if the lower target cannot be achieved without adverse outcomes (see Comprehensive Type 2 Diabetes Management Algorithm—Goals for Glycemic Control). Significant reductions in the risk or progression of nephropathy were seen in the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADV ANCE) study, which targeted an A1C <6.5% in the intensive therapy group versus standard approaches (72). In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, inten-sive glycemic control significantly reduced the risk and/ or progression of retinopathy, nephropathy, and neuropathy (73,74). However, in ACCORD, which involved older and middle-aged patients with longstanding T2D who were at high risk for or had established CVD and a baseline A1C >8.5%, patients randomized to intensive glucose-lowering therapy (A1C target of <6.0%) had increased mortality (75). The excess mortality occurred only in patients whose A1C remained >7% despite intensive therapy, whereas in the standard therapy group (A1C target 7 to 8%), mortality followed a U-shaped curve with increasing death rates at both low (<7%) and high (>8%) A1C levels (76). In contrast, in the Veterans Affairs Diabetes Trial (V ADT), which had a higher A1C target for intensively treated patients (1.5% lower than the standard treatment group), there were no between-group differences in CVD endpoints, cardiovas-cular death, or overall death during the 5.6-year study period (75,77). After approximately 10 years, however, V ADT patients participating in an observational follow-up study were 17% less likely to have a major cardiovascu-lar event if they received intensive therapy during the trial (P<.04; 8.6 fewer cardiovascular events per 1,000 person-years), whereas mortality risk remained the same between treatment groups (78). Severe hypoglycemia occurs more frequently with intensive glycemic control (72,75,77,79). In ACCORD, severe hypoglycemia may have account-ed for a substantial portion of excess mortality among patients receiving intensive therapy, although the hazard ratio for hypoglycemia-associated deaths was higher in the standard treatment group (80). Cardiovascular auto-nomic neuropathy may be another useful predictor of cardiovascular risk, and a combination of cardiovascular autonomic neuropathy (81) and symptoms of peripheral neuropathy increase the odds ratio to 4.55 for CVD and mortality (82).Taken together, this evidence supports individualization of glycemic goals (2). In adults with recent onset of T2D and no clinically significant CVD, an A1C between 6.0 and 6.5%, if achieved without substantial hypoglycemia or other unacceptable consequences, may reduce lifetime risk of microvascular and macrovascular complications. A broader A1C range may be suitable for older patients and those at risk for hypoglycemia. A less stringent A1C of 7.0 to 8.0% is appropriate for patients with history of severe hypoglycemia, limited life expectancy, advanced renal disease or macro-vascular complications, extensive comorbid conditions, or long-standing T2D in which the A1C goal has been diffi-cult to attain despite intensive efforts, so long as the patient remains free of polydipsia, polyuria, polyphagia, or other hyperglycemia-associated symptoms. Therefore, selection of glucose-lowering agents should consider a patient’s ther-apeutic goal, age, and other factors that impose limitations on treatment, as well as the attributes and adverse effects of each regimen. Regardless of the treatment selected, patients must be followed regularly and closely to ensure that glyce-mic goals are met and maintained.The order of agents in each column of the Glucose Control Algorithm suggests a hierarchy of recommended usage, and the length of each line reflects the strength of the expert consensus recommendation (see Comprehensive Type 2 Diabetes Management Algorithm—Glycemic Control Algorithm). Each medication’s properties should be considered when selecting a therapy for individual patients (see Comprehensive Type 2 Diabetes Management Algorithm—Profiles of Antidiabetic Medications), and healthcare professionals should consult the FDA prescrib-ing information for each agent.• Metformin has a low risk of hypoglycemia, can promote modest weight loss, and has good antihyper-glycemic efficacy at doses of 2,000 to 2,500 mg/day.Its effects are quite durable compared to sulfonylureas (SFUs), and it also has robust cardiovascular safety relative to SFUs (83-85). Owing to risk of lactic acido-。
2016AACEACE共识声明:糖尿病综合管理方案

2016 AACEACE 共识声明:糖尿病综合管理方案2016 年1 月,美国临床内分泌医师协会(AACE )和美国内分泌学会(ACE )共同更新了2 型糖尿病综合管理方案,指南内容涵盖生活方式干预、总体指导原则及相关药物组合。
指南发表于《Endocrine Practice 》。
指南要点概括如下。
基本原则1、生活方式治疗,包括药物辅助减重,是治疗 2 型糖尿病的关键。
2、应根据个体化制定A1C 目标。
3、血糖控制目标包括空腹血糖和餐后血糖。
4、根据患者个体特征、医疗费用对患者的影响、处方限制以及患者的个人喜好选择个体化治疗方式。
5、优先选择低血糖风险最小化的治疗方案。
6、优先选择体重增加风险最小化的治疗方案。
7、初始药物费用只是总医疗费用的一部分,后者还包括必要的监测费用、控制低血糖风险以及体重增加风险的费用、保证治疗安全性的费用等。
8、本方案的分层治疗基于初始A1C 水平。
9、联合用药治疗时应选择具有互补作用机制的药物。
10、综合治疗包括血脂、血压以及相关并发症的治疗。
11、治疗期间需要经常评估治疗效果(如每 3 个月一次)直至病情稳定,之后可降低评估频率。
12、治疗方案应尽可能简单以提高依从性。
13、本方案包含的糖尿病治疗药物均经过FDA 批准。
血糖控制根据个体化制定A1C目标• A1C三6.5% :针对无严重疾病并存及低血糖发生风险较低的患者。
• A1C > 6.5% :针对合并严重疾病以及有低血糖发生风险的患者。
生活方式治疗生活方式治疗从营养咨询和教育开始。
所有患者应保持以植物类为基础的饮食习惯;增加多不饱和脂肪酸和单不饱和脂肪酸的摄入,避免反式脂肪酸和饱和脂肪酸摄入,以努力达到并保持最佳体重。
超重/肥胖患者应限制热量摄入以达到减重5%-10% 的目标。
结构化咨询(每周或每月一次的特定减肥课程)以及替代饮食已被证明比标准的办公室咨询更有效。
体力活动是减肥和维持计划的主要组成部分。
美国临床内分泌学医师学会发布2型糖尿病治疗新指南

w i t h s e l e r o s i n g p a n c r e a t i t i s[ J ] .N E n g l J
Me d ,2 0 0 1 ,3 4 4( 4 ) :7 3 2— 7 3 8 .
5 Wa k ha a y a s h i T, Ka wa u r a K ," S a t o mu r a Y, e t 1 . Cl a i n i c a l a n d i ma g i n g f e a t u r e s o f a u t o i m—
2 0 0 3,9 8( 6 ) :2 6 7 9— 2 6 8 7 .
Ta k a y o s h i N , F u mmi mk e T, Hi r o y a s u 0,
病的可能性 ,再进一步完善相关检查 ,也 6
血清学 ( 必备 1条 ) :( 1 )血 清 I g G 可行 诊断性治疗 ,就能 明确诊断 A l P 。 或I g G 4水平 升高 ;( 2 )其他 自身 抗体 阳 参 考 文 献
mu n e p nc a r e a t i c wi t h f o c a l p nc a r e a t i c a we l l i n g o r ma s s f o r ma t i o n: c o mp a is r o n w i t h S O —
[ J ] .I n t e na r l Me d i c i n e ,2 0 0 6 ,4 5( 8) :
4 9 7 .
组 织学 :发 现胰 腺 淋 巴细 胞 、浆 细 胞 浸 润 以及 纤 维 化 ,有 大 量 I g G 4 阳性 细 胞
浸润 。
e t 1.A a u t o i m mu n e p a n e r e a t i t i s[ J ] .N E n — g l J M e d ,2 0 0 6,3 5 5( 1 ) :2 6 7 0—2 6 7 6 .
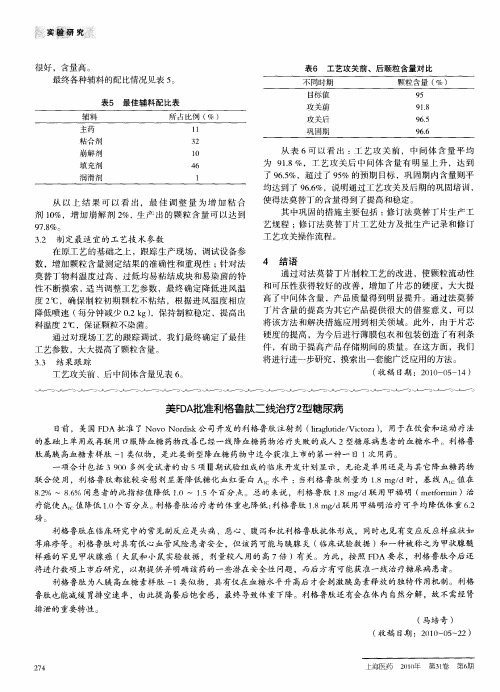
美FDA批准利格鲁肽二线治疗2型糖尿病
通过对法莫 替丁片制粒工艺 的改进 ,使颗粒流动性
和可压性获得较好 的改 善 ,增 加 了片芯 的硬度 ,大大提
通过对现场工艺 的跟踪 调试 ,我们最 终确定 了最佳 工艺 参数 ,大大提 高了颗粒含量。
33 结 果 跟 踪 .
高了 中间体含量 ,产 品质量得 到明显提升 。通过法莫替 丁片含量 的提高 为其它 产品提供很大的借鉴意 义,可 以 将 该方法和解决措施应 用到相关领域 。此外 ,由于片芯 硬度 的提高 ,为今后进行 薄膜 包衣和包装创造 了有利 条
磅。
利格鲁肽在 临床研 究 中的常见副反应是 头痛 、恶心、腹泻和抗利格鲁肽抗体形成 ,同时也见有 变应反应样症状如
荨麻疹等。利格鲁肽对具有低 心血 管风险患者安全 ,但该 药可能与胰腺 炎 ( 临床试验数据 )和一种被称之为 甲状腺髓 样癌 的罕见 甲状腺癌 ( 大鼠和 小鼠实验数据 ,剂量较人 用的 高 7 )有关。为此 ,按 照 F A要 求 ,利格鲁 肽今后还 倍 D 将进行数项上市后研 究,以期提供并 明确该药的一 些潜在安全性 问题 ,而后 方有可能获准一线治疗糖尿病 患者。 利格鲁肽为人胰 高血糖素样肽 一 类似物 ,具有仅在血糖 水平升 高后 才会刺激胰 岛素释放 的独特作 用机制。利格 1 鲁肽也能减缓 胃排 空速率 ,由此提 高餐后饱 食感,最终导致体重下降。利格鲁肽还 有会在体 内 自然分解,故不需经 肾
0 一实鼍 姗 的配 比情况见表 5 。
表5 最 佳辅料 配 比表
辅 料 所 占 比例 ( ) %
1 1 3 2 1 0 4 6 1
表 6 工 艺攻 关前 、后 颗粒含 量对 比
不同时期
2型糖尿病患者自我管理行为量表(DSCS)

5.在同一类食物中进行食物代换
6.定时用餐
锻炼
7.平时坚持锻炼
8.繁忙时仍坚持锻炼
9.主观上不想运动时仍坚持锻炼
10.周末或节假日仍坚持锻炼
遵医嘱
服药
11.平时遵医嘱按时服药
12.出门在外时仍按时服药
13.遵医篡按量服药
血糖
监测
14平时定期监测血糖或尿*
15.出门在外时仍定期监测
2型糖尿病患者自我管理行为量表(DSCS)
您好,此表是为了了解您目前的自我管理行为水平,请根据您的实际情况进行选择,在相应每-行打“√”
自我管理行为
完全没有做到
很少做到
有时做到
经常做到
完全做到
饮食
控制
1.平时严格控制饮食
2出门到熟悉的地方用鬓(如朋友、亲戚家)时仍控制饮食
3.与不热悉的人-起用餐时仍控制饮食
16.记录每次血糖或尿糖的
17.感到不舒服时增加血糖或尿糖的测量次数
足部
护理
18.平时穿软底、宽松、透气的鞋袜19每日检查足部并在足部涂抹润肤露
20.出外应酬仍穿软底、宽松、透气的鞋
21.按规定修剪趾甲
22.足部有异常时立即找医护人员进行处理
高、低血糖
23.血糖控制不佳时及进找医生处理
24.自觉血糖太低时采取正确的百我处理措施
25.血糖比平时高时采取正确的自我处理措施
26.运动时采取预防低血糖措施
2型糖尿病血糖控制策略和治疗路径(防治指南)、附路径图

2型糖尿病血糖控制策略和治疗路径(防治指南)、附路径图前文《什么是糖尿病》中已经讲述,2型糖尿病是因胰岛素绝对或相对分泌不足或(和)胰岛素抵抗而导致高血糖为主要症状的代谢紊乱性疾病。
因此,治疗糖尿病的重要手段之一就是采取综合治疗方法来降低血糖。
下面来看看《中国糖尿病防治指南》提供了怎样的治疗策略和路径。
2型糖尿病是一种进展性的疾病,随着病程的进展,血糖有逐渐升高的趋势,控制高血糖的治疗强度也应随之加强,常需要多种手段的联合治疗。
生活方式干预贯穿始终生活方式干预是2型糖尿病的基础治疗措施,应贯穿于糖尿病治疗的始终。
药物治疗如果单纯生活方式不能使血糖控制达标,则启动药物治疗。
1、首先单药治疗首选:二甲双胍。
若无禁忌证,二甲双胍应一直保留在糖尿病的治疗方案中。
如果不适合二甲双胍治疗者,可选择a-糖苷酶抑制剂或胰岛素促泌剂。
2、二联治疗如单独使用二甲双胍治疗而血糖仍未达标,则可进行二联治疗。
即:二甲双胍 + 胰岛素促泌剂(磺脲类药物:格列苯脲、格列齐特、格列吡嗪、格列喹酮等;格列奈类药物:瑞格列奈、那格列奈等)二甲双胍 +a-糖苷酶抑制剂(阿卡波糖、伏格列波糖)二甲双胍 +DPP-4抑制剂(沙格列汀、西格列汀、维格列汀、利格列汀、阿格列汀)二甲双胍 +TZDs (罗格列酮、吡格列酮)二甲双胍 + SGLT-2抑制剂(达格列净、坎格列净、恩格列净)二甲双胍 + 胰岛素二甲双胍 +GLP-l受体激动剂(艾塞那肽、贝那鲁肽、利拉鲁肽、度拉糖肽)3、三联治疗上述不同机制的降糖药物可以三种药物联合使用。
二甲双胍 + 其他两种4、多次胰岛素治疗如三联治疗控制血糖仍不达标,则应将治疗方案调整为多次胰岛素治疗(基础胰岛素加餐时胰岛素或每日多次预混胰岛素)。
特别提示:采用多次胰岛素治疗时应停用胰岛素促分泌剂。
2 型糖尿病高血糖治疗路径图糖尿病治疗常用药物介绍目前糖尿病治疗药物包括口服药和注射制剂两大类。
口服降糖药主要有促胰岛素分泌剂、非促胰岛素分泌剂、二肽基肽酶-4抑制剂(DPP-4抑制剂)和钠-葡萄糖共转运蛋白2抑制剂(SGLT-2抑制剂)。
美国糖尿病学会_ADA_2016指南_糖尿病血糖控制诊疗标准_
-905.[12]Qi DJ ,Zhang LH ,Wang S ,et al.Evaluation of case -centered ,problem -based and community -oriented curriculum teaching model in general practice [J ].Chinese General Practice ,2012,15(2):418-420,424.(in Chinese )齐殿君,张联红,王爽,等.“以病例为中心、问题为基础、社区为导向”全科医学教学模式的效果评价研究[J ].中国全科医学,2012,15(2):418-420,424.[13]Li XY ,Tian ZB ,Wang XM ,et al.Undergraduates assumingresponsibility in clinical placement [J ].China Higher Medical Education ,2015,29(2):16-17.(in Chinese )李晓宇,田字彬,王雪梅,等.“责任制实习法”对本科临床实习教学效果探讨[J ].中国高等医学教育,2015,29(2):16-17.[14]Zhu WH ,Fang LZ ,Dai HL ,et al.Utility of tutorial system instandardized training management of general practitioners [J ].Chinese Journal of General Practice ,2014,12(3):333-335.(in Chinese )朱文华,方力争,戴红蕾,等.导师跟踪模式在全科住院医师规范化培训管理中的运用[J ].中华全科医学,2014,12(3):333-335.[15]姚永祥,王宏智,刘建迪.实行实习医生导师制提高临床实习教学效果[J ].现代医药卫生,2003,19(12):1650.[16]高力军,吴群红,郝艳华,等.发达国家全科医生培养模式对我国的启示[J ].继续教育,2014,28(1):58-59.[17]吕慈仙,李学兰.国外全科医生培养方式及其对我国高等院校的启示[J ].中国农村卫生事业管理,2012,32(8):779-782.[18]Yu XY.Exploration on the curriculum system reform of generalmedical clinical teaching [J ].The Science Education Article Cultures ,2015,12(8):79-80.(in Chinese )郁晓燕.全科医学临床教学课程体系的改革探索[J ].科教文汇,2015,12(8):79-80.[19]全国教育科学规划领导小组办公室.“我国全科医生培养模式创新研究”成果报告[J ].大学:学术版,2012,7(4):84-89.[20]He KR.Discussing the medical humanities education in generalpractitioners system [J ].Chinese Health Service Management ,2014,31(4):291-293.(in Chinese )何昆蓉.论全科医生制度下的医学人文教育[J ].中国卫生事业管理,2014,31(4):291-293.(收稿日期:2015-12-10;修回日期:2016-03-15)(本文编辑:闫行敏)·全科医生知识窗·美国糖尿病学会(ADA )2016指南:糖尿病血糖控制诊疗标准近日美国糖尿病学会(ADA )更新了2016年糖尿病诊疗标准,于2015-12-22在线发表于Diabetes Care 2016年1月份增刊。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
AACE/ACE
2 型 糖 尿 病 综 合 管 理 方 案
2016
Martin J. Abrahamson, MD Joshua I. Barzilay, MD, FACE Lawrence Blonde, MD, FACP, FACE Zachary T. Bloomgarden, MD, MACE Michael A. Bush, MD Samuel Dagogo-Jack, MD, DM, FRCP, FACE Ralph A. DeFronzo, MD
AGi
SU/GLN
治疗3个月后, 未达到治疗目标, 则进行三药联合治疗
*药物的顺序代表药物使用的等级顺序;线条的长度代表推荐的强度
三 联 疗 法*
GLP-1 RA
MET
或其他 一线药物 +二线药物
+
SGLT-2i TZD 基础胰岛素 DPP-4i 考来维仑
溴隐亭-快速释放剂型
AGi
SU/GLN
治疗3个月后, 则加用胰岛素, 或强化胰岛素治疗
第 2 页
营 养
运 动 睡 眠 行 为 支 持 戒 烟
生 活 方 式 干 预
糖 尿 病 并 发 症 危 险 分 层
依 据 肥 胖 与 并 发 症 进 行 危 险 度 分 层
t维持最佳体重水平 t热量限制 t素食为主饮食;富含多不饱和脂肪酸 t和避单免不进饱食和反脂式肪脂酸肪酸;
限制饱和脂肪酸的摄入
t每周150分钟中等强度运动
(如步行、爬楼梯)
t力量训练 t耐受后增大运动强度
t 每晚约7小时
t参与社区活动 t筛查情感障碍情绪异常
t拒绝任何烟草制品
+ t规划的咨询课程 t膳食替代
+ t规划锻炼 项目
+ t医学评估/排除 t 医学监测
+ t阻塞性睡眠呼吸暂停筛查
+ t转诊至精神科 t行为治疗
第 3 步
外科手术治疗 (BMI ≥ 35):
胃束带术,袖状胃切除术,或胃转流术
如果未达到并发症的治疗目标,则应进行强化的生活方式干预、药物和/或外科手术治疗, 进一步减轻体重
第 4 页
糖 尿 病 前 期 治 疗 方 案
IFG (100–125) | IGT (140–199) | 代谢综合征(NCEP 2001)
加用钙通道拮抗剂,ß 受体阻滞剂
或噻嗪类利尿剂
如未达标(2-3个月)
加用上述药物种类中的 一种新药,依此类推
如未达标(2-3个月)
其他选择(α受体阻滞剂, 中枢降压药物,血管舒张药物,
醛固酮拮抗剂)
血压达标至关重要
第 9 页
降 糖 药 物 概 况
二甲 GLP-1 RA SGLT-2i DPP-4i 双胍
中 性
中 度 中 性
中 性 中 性
?
轻 度 中 度
中 性
中 性 安 全
中 性 中 性
中 度 中 性
骨 骼 中 性
中 性 中 性
中 性
中 度
中 性
中 性
骨折风险
中 性 中 性
中 性 中 性
不良反应少或可能获益
谨慎使用
可能存在不良反应
? 影响不确定
第 10 页
AACE/ACE 2型糖尿病综合管理方案基本原则
+ t规划戒烟项目
第 3 页
以并发症治疗为中心的超重/肥胖患者治疗模式
第 1 步
无并发症 BMI ≥25
第 2 步
选 择
并 发 症 的 评 估 与 分 级 心 脏 代 谢 性 疾 病 | 生物力学并发症
BMI 25–26.9
加强生活干预(减重、锻炼、饮食调整) 以及控制血糖;考虑额外治疗
降低LDL-C: 降低非-HDL-C、TG: 降载脂蛋白- B, LDL-P:
降低FH患者LDL-C:**
强化他汀类治疗,加用依替米贝,PCSK9基因抑制剂,考来维仑或烟酸 强化他汀类治疗和/或加用处方级ω-3脂肪酸,贝特类药物,和/或烟酸 强化他汀类治疗和/或加用依替米贝,PCSK9基因抑制剂,考来维仑,和/或烟酸 他汀类药物+ PCSK9基因抑制剂
控 制 目 标 个 体 化
A1C ≤ 6.5%
针对无严重疾病并存 及低血糖发生风险较低
的患者
A1C > 6.5%
针对合并严重疾病 及有低血糖发生风险
的患者
注:A1C,糖化血红蛋白;
第 6 页
血 糖 控 制 方 案
生 活 方 式 干 预
(包 括 医 学 辅 助 减 重 治 疗)
就诊时 A1C< 7.5%
r FBG> 180 mg/dLT:DD增加20% r FBG140–180 mg/dTLD: D增加10% r FBG110–139 mg/dTLD: D增加1单位 r 如果发生低血糖,TDD减量: r BG< 70 mg/dL减: 10%-20% r BG< 40 mg/dL减: 20%-40%
r 起始剂量:TDD的 50%,分为三个剂量 三餐前给药
每2-3天调整胰岛素剂量以达到血糖控制目标:
r 如果餐后2小时血糖或下一餐前血糖持续> 140 mg/dL,则将 餐时胰岛素用量增加10%或1-2单位
r 如果发生低血糖反应,降低基础TDD或/和餐前胰岛素: r 血糖持续< 70 mg/dL:减10%-20% r 严重低血糖反应(需要其他人帮助)或 血糖< 40 mg/dL:减20%-40%
*TDD:胰岛素总量
第 8 页
ASCVD 风 险 因 素 改 善 方 案
血 脂 异 常
高 血 压
生 活 方 式 干 预 ( 包 括 医 学 辅 助 减 重 治 疗 )
血 脂 检 测:评 估 ASCVD 风险
他 汀 类 药 物 治 疗
若甘油三脂(TG)> 500 mg/dL,使用贝特类药物,处方级ω-3脂肪酸,烟酸
开始基础胰岛素治疗后考虑磺脲类药物停用或减量 (基础胰岛素类似物优于中效胰岛素)
*血糖控制目标
r 对于大多数2型糖尿病患者,A1C<7%; 空腹和餐前血糖< 110 mg/dL;无低血糖发生
r 依据患者的年龄、糖尿病病程长短、合并症、糖尿病并发症 以及低血糖发生风险等因素,调整A1C和空腹血糖的控制目标
Irl B. Hirsch, MD Paul S. Jellinger, MD, MACE Janet B. McGill, MD, FACE Jeffrey I. Mechanick, MD, FACP, FACE, FACN, ECNU Paul D. Rosenblit, MD, PhD, FNLA, FACE Guillermo Umpierrez, MD, FACP, FACE
若他汀类药物不耐受
换用另一种他汀类药物, 减低他汀类药物剂量或给药频次 或加用非他汀类的降LDL-C药物
重复血脂检测,
根据风险水平强化治疗,
评估治疗的充分性和耐受性 以达治疗目标
风险水平
LDL-C (mg/dL) 非-HDL-C (mg/dL)
TG (mg/dL) TC/HDL-C 载脂蛋白- B (mg/dL) LDL-P (nmol/L)
有并发症 BMI ≥ 27: 并发症严重度分级
轻、中度
重 度
并 发 症 改 善 目 标
+ + 治 疗 方 式
依 据 分 级 确 定 治 疗 强 度
生活方式干预
向内科医师/注册营养师咨询;网络/远程干预项目;规划的多学科干预项目
药物治疗 (BMI ≥ 27):
苯丁胺,奥利司他,氯卡色林,苯丁胺/托吡酯缓释剂, 纳曲酮/安非他酮,利拉鲁肽3mg
第 1 页
内 容 目 录
2 型 糖 尿 病 综 合 管 理 方 案
I. 生 活 方 式 干 预 II. 以 并 发 症 治 疗 为 中 心 的 超 重 / 肥 胖 患 者
治 疗 模 式 III. 糖 尿 病 前 期 治 疗 方 案 IV. 血 糖 控 制 目 标 V. 血 糖 控 制 方 案 VI. 胰 岛 素 起 始 / 强 化 治 疗 方 案 VII. ASCVD 风 险 因 素 改 善 方 案 VIII. 降 糖 药 物 概 况 IX. 2 型 糖 尿 病 治 疗 原 则
低血糖 中 性
中 性 中 性
中 性
AGi
中 性
TZD SU
考来
中等剂量
GLN 维仑
中 性
中/重 度
中 性
轻 度
BCR-QR 胰岛素
中 性 中至重度
普兰 林肽
中 性
体 重 轻度减轻 减 轻
减 轻 中 性 中 性 增 加 增 加 中 性 中 性 增 加 减 轻
3B、4、 CrCl < 30时
必要时
肾脏/泌尿 生殖系统
血糖控制 未达标*
基础胰岛素加1、2、 基础胰岛素联合 3次餐时胰岛素治疗 餐时胰岛素治疗
r 在主餐前加用 1次餐时胰岛素
r 如果未达标, 则加用2次或 3次餐时胰岛素
r 起始即采用每次 餐前加用餐时 胰岛素方案
r 50%基础胰岛素/ 50%餐时胰岛素 TDD 0.3–0.5 U/kg
r 起始剂量:基础胰 岛素剂量的10% 或5单位
5期CKD
不推荐
eGFR < 45时 调整剂量 无 效 (利拉利汀
禁用
艾塞那肽 生殖系统
除外)
霉菌感染
中 性
中 性
更高的 低血糖 发生风险
中 性
中 性
更高的 低血糖 发生风险
中 性
胃肠道 中 度 反应 慢性心衰 中 性 ASCVD 获 益
中 度 中 性
中 性 中 性
中 性
可 能 获 益
