医学英语病历书写范文住院病历书写的范文
医学英语病历范文
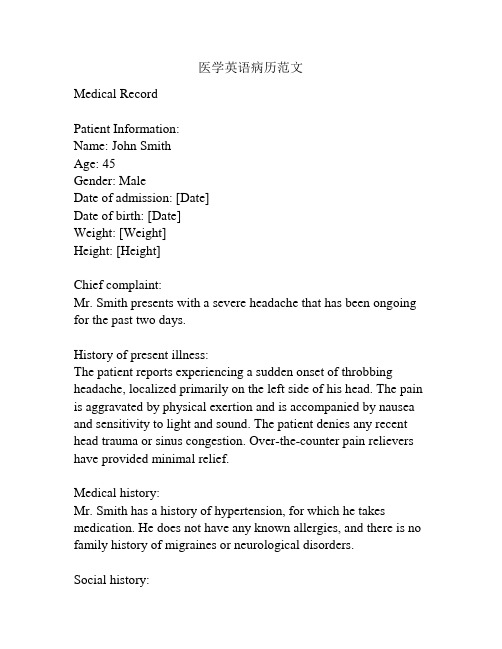
医学英语病历范文Medical RecordPatient Information:Name: John SmithAge: 45Gender: MaleDate of admission: [Date]Date of birth: [Date]Weight: [Weight]Height: [Height]Chief complaint:Mr. Smith presents with a severe headache that has been ongoing for the past two days.History of present illness:The patient reports experiencing a sudden onset of throbbing headache, localized primarily on the left side of his head. The pain is aggravated by physical exertion and is accompanied by nausea and sensitivity to light and sound. The patient denies any recent head trauma or sinus congestion. Over-the-counter pain relievers have provided minimal relief.Medical history:Mr. Smith has a history of hypertension, for which he takes medication. He does not have any known allergies, and there is no family history of migraines or neurological disorders.Social history:The patient is a smoker, consuming approximately 10 cigarettes per day. He drinks alcohol in moderation, primarily on social occasions. He denies any illicit drug use. His occupation involves long hours of computer work.Physical examination:On examination, the patient appears to be in mild distress due to the headache. His vital signs are within normal limits. Neurological examination reveals no focal deficits, and his cranial nerves appear to be intact. There is no evidence of meningeal irritation. His neck is supple, and there is no nuchal rigidity. The remainder of the physical examination is unremarkable. Laboratory tests:Blood tests, including a complete blood count and comprehensive metabolic panel, were performed. All results were within normal limits.Imaging studies:A brain MRI was ordered to rule out any structural abnormalities. The scan revealed no evidence of intracranial hemorrhage, mass, or other abnormalities.Assessment and plan:Mr. Smith is presenting with a severe headache consistent with a migraine without aura. He will be prescribed a triptan medication for acute management of his headache. He will also be counseled on lifestyle modifications, including smoking cessation and stress reduction techniques. A follow-up appointment will be scheduled in two weeks to evaluate the effectiveness of the treatment plan.Additionally, the patient is advised to seek immediate medical attention if his symptoms worsen or if he develops any new neurological symptoms.Signature: [Physician's Name]Date: [Date]。
英语病历作文格式模板
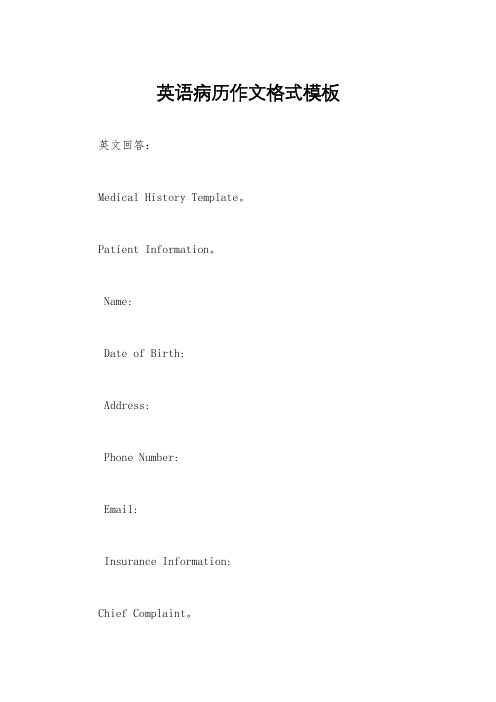
英语病历作文格式模板英文回答:Medical History Template。
Patient Information。
Name:Date of Birth:Address:Phone Number:Email:Insurance Information:Chief Complaint。
A brief summary of the patient's primary reason for the visit.Example: "The patient presents with a 3-day history of fever and chills."History of Present Illness。
A detailed description of the patient's symptoms, including:Onset: When did the symptoms first appear?Duration: How long have the symptoms been present?Severity: How severe are the symptoms?Location: Where are the symptoms located?Associated symptoms: Any other symptoms that are present, such as nausea, vomiting, or headache.Past Medical History。
A list of any previous medical conditions, surgeries, or hospitalizations.Example: "The patient has a history of hypertension and hyperlipidemia."Family History。
住院病历英文作文

住院病历英文作文I was admitted to the hospital last week due to a severe stomachache. It came on suddenly and was so intense that I couldn't even stand up straight. The doctors ran some tests and found out that I had acute appendicitis, so they decided to perform surgery to remove my appendix.The surgery went well, but the recovery process has been tough. I've been in a lot of pain and have had trouble sleeping. The nurses have been really helpful though, and they've been giving me pain medication to help manage the discomfort.I've been feeling pretty bored and restless in the hospital. I miss being able to go outside and do things on my own. I've been trying to pass the time by reading, watching TV, and chatting with the other patients, but it's still tough being cooped up in this room all day.The food here is not great. I know hospital food isn'tsupposed to be gourmet, but I was hoping for something a little more appetizing. I've been craving some real home-cooked meals, and I can't wait to get out of here and eat some good food.I'm grateful for the care I've received here, but I'm really looking forward to going home. I miss my own bed, my own shower, and just being in my own space. I know I still have some recovery ahead of me, but I can't wait to get back to my normal routine.。
住院病历英语作文

住院病历英语作文In the medical field, the importance of accurate and detailed patient records cannot be overstated. Hospital discharge summaries, in particular, serve as vital documents that provide an overview of a patient's hospital stay, including their diagnosis, treatment, and progress.As the global community becomes increasingly interconnected, the ability to communicate medical information in auniversal language like English has become crucial. This article aims to guide medical professionals and students through the process of writing hospital discharge summaries in English, emphasizing the key elements and best practices. **Structure of a Hospital Discharge Summary**A hospital discharge summary typically follows a standard structure, which ensures consistency and ease of understanding. Here's a breakdown of the key sections:1. **Patient Information**: This section includes basic details about the patient, such as their full name, age, gender, and contact information. It also provides thepatient's admission and discharge dates.* Example: "Patient Name: John Doe, Age: 45, Gender: Male, Admission Date: 01/01/2023, Discharge Date:01/10/2023." 2. **Admission Diagnosis**: This section summarizes the patient's primary reason for being admitted to the hospital.* Example: "Admission Diagnosis: Acute Myocardial Infarction (AMI)." 3. **Hospital Course**: This section details the patient's progress and treatment during their hospital stay. It should include any significant medical events, procedures, and changes in the patient's condition. * Example: "During his stay, the patient underwent coronary angioplasty and stent placement. His symptoms improved gradually, and he was stable by the end of his hospital stay." 4. **Discharge Diagnosis**: This section provides the final diagnosis based on the patient's condition and any tests or procedures performed duringtheir stay.* Example: "Discharge Diagnosis: ST-elevation myocardial infarction (STEMI) with successful revascularization." 5. **Discharge Instructions**: This section outlines the care instructions for the patientafter discharge, including any recommended medications, follow-up appointments, and lifestyle modifications.* Example: "Patient is advised to continue taking aspirin and statin medication regularly. Follow-up appointment with the cardiologist is scheduled for02/01/2023. Patient is also advised to quit smoking and maintain a healthy diet." 6. **Signature**: The discharge summary should be signed and dated by the attending physician to certify its authenticity.* Example: "Signed and dated by Dr. Smith on01/10/2023."**Writing Tips for Hospital Discharge Summaries**When writing hospital discharge summaries in English, here are some key tips to ensure clarity and accuracy:* **Use Simple Language**: Avoid complex medical terminology and stick to plain English to ensure that the information is easily understood by non-medical personnel. * **Focus on the Essentials**: Stick to the key points and avoid adding irrelevant details. The summary should be concise and focused. * **Provide Accurate Information**:Ensure that all information, including dates, procedures, and diagnoses, is accurate and up-to-date. Double-check all facts before finalizing the summary. * **Use Bullet Points or Lists**: Organize information using bullet points or lists to make it easier to read and understand. ***Proofread**: Always proofread your work to catch any spelling or grammar errors that could affect the clarity of the information.By following these tips and adhering to the standard structure of a hospital discharge summary, medical professionals and students can ensure that they are providing patients and other medical providers with accurate, detailed, and easily understandable medical information. This is crucial for effective patient care and safe medical practice.。
最新英文住院病例模板

Divisi on: _________ Ward: __________ Bed: _________ Case No. ___________Name: _____________ Sex: __________ Age: ___________ Natio n: ___________ Birth Place: ________________________________ Marital Status: _____________ Work-orga nizatio n & Occupatio n: _____________________________________ Livi ng Address & Tel: _________________________________________________ Date of admissio n: ______ D ate of history taken: ______ Informant: __________Chief Complaint: ___________________________________________History of Present Illness:Past History:General Health Status: 1.good 2.moderate 3.poorDisease history:(if any, please write down the date of onset, brief diagnosticand therapeutic course, and the results.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest painCirculatory system:1.None2.Palpitation3.exertional dyspnea4..cyanosis5.hemoptysis6.Edema of lower extremities7.chest pain8.syncope9.hypertension Digestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea11.hematemesis 12.Hematochezia 13.jaundiceUrinary system:1.None2.Lumbar pain3.urinary frequency4.urinary urgency5.dysuria6.oliguria7.polyuria 8.retention of urine 9.incontinence of urine 10.hematuria11.Pyuria 12.nocturia 13.puffy faceHematopoietic system:1.None2.Fatigue3.dizziness4.gingival hemorrhage5.epistaxis6.subcutaneous hemorrhageMetabolic and endocrine system:1.None2.Bulimia3.anorexia4.hot intolerance5.cold intolerance6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character change 11.Marked obesity12.marked emaciation 13.hirsutism 14.alopecia15.Hyperpigmentation 16.sexual function changeNeurological system:1.None2.Dizziness3.headache4.paresthesia5.hypomnesis6. Visual disturbance7.Insomnia8.somnolence9.syncope 10.convulsion 11.Disturbance of consciousness12.paralysis 13. vertigoReproductive system:1.None2.othersMusculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophyInfectious Disease:1.None2.Typhoid fever3.Dysentery4.Malaria 4.Schistosomiasis4. Leptospirosis 7.Tuberculosis 8.Epidemic hemorrhagic fever9.othersVaccine inoculation:1.None2.Yes3.Not clearVaccine detail _________________________________________ Trauma and/or operation history: Operations:1.None2.YesOperation details: _______________________________________ Traumas:1.None2.YesTrauma details: _________________________________________ Blood transfusion history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredient transfusion) Blood type:Transfusion time: ______Transfusion reaction1.None2.YesClinic manifestation: ____________________________ Allergic history:1.None2.Yes3.Not clear allergen: __________________________________clinical manifestation: _____________________________________Personal history:Custom living address_: __________________________________________Resident history in endemic disease are_a_: _________________________Smoking: 1.No 2.YesAverage ___pieces per day; about___yearsGiving-up 1.No 2.Yes (Time: _______________________ ) Drinking: 1.No 2.YesAverage ___grams per day; about ___yearsGiving-up 1.No 2.Yes(Time: _________________________ ) Drug abuse:1.No 2.YesDrug names: _______________________________________Marital and obstetrical history:Married age: _________ years old Pregnancy ______________ timesLabor _______________ times(〔.Natural labor: _____ times 2.0perative labor: __________ times3. __________________ Natural abortion: _______________ times4.Artificial abortion: ____ times5. _______________________ P remature labor: ________ times6.stillbirth________________________ t imes)Health status of the Mate:1.Well2.Not fineDetails: _______________________________________________Menstrual history:Menarchal age: ______ Duration ________ d ay Interval ________ daysLast menstrual period: ___________ Menopausal age: _____ years oldAmount of flow: 1.small 2. moderate 3. large Dysmenorrheal: 1. prese nee2.abse nc M enstrual irregularity 1. No 2.YesFamily history: (especially pay atte ntio n to the in fectious and hereditary diseaserelated to the present illness)Father: l.healthy 2.ill: ________ 3.deceased cause: ____________________ Mother:1.healthy 2.ill: ________ 3.deceased cause: ____________________ Others: ________________________________________________________The an terior stateme nt was agreed by the in forma nt.Sig nature of in forma nt: Datetime:Physical ExaminationVital signs:Temperature:0C Blood pressure: / mmHg Pulse: _________ bpm (l.regular 2.irregular ) Respirati on: _______ bpm (l.regular 2.irregular ) General conditions:Development:I.Normal 2.Hypoplasia 3.HyperplasiaNutrition: l.good 2.moderate 3.poor 4.cachexiaFacial expression 1. no rmal 2.acute 3.chro nic other __________________Habitus: l.asthenic type 2.sthenic type 3.ortho-thenic typePosition: l.active 2.positive pulsive 4.other ______________________ Consciousness l .clear 2.somnolence 3.confusion 4.stupor 5.slight coma6. mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: l.normal 2.abnormal ______Skin and mucosa:Color: 1.normal 2.pale 3.redness 4.cyanosis 5.jaundice 6.pigmentationSkin eruption:1.No 2.Yes( type: _________ distribution: __________________ ) Subcutaneous bleeding1: .no 2.yes (type: ____ distribution: ______________ )Edema:1. no 2.yes ( location and degree _______________________________ ) Hair: 1.normal 2.abnormal(details _____________________________________ ) Temperature and moisture:normal cold warm dry moist dehydration Liverpalmar : 1.no 2.yes Spider angioma(location: __________________________ ) Others: __________________________________________________________Lymph nodes: enlargement of superficial lymph node:1. no2.yesDescription: _______________________________________________Head:Skull size:1.normal 2.abnormal (description: ___________________________ ) Skull shape:1.normal 2.abnormal(description: __________________________ ) Hair distribution :1.normal 2.abnormal(description: ______________________ ) Others: ___________________________________________________________ Eye: exophthalmos: __________ e yelid: ___________ conjunctiva: _________ sclera: ________________ C ornea: ______________________Pupil: 1.equally round and in size 2.unequal (R _____ mm L _______ mm)Pupil reflex: 1.normal 2.delayed (R___s L___s ) 3.absent (R___L___) others:__________________________________________________________ Ear: Auricle 1.normal 2.desformation (description: _____________________ ) Discharge of external auditory canal:1.no 2.yes (1.left 2.right quality: ___ )Mastoid tenderness 1.no 2.yes (1.left 2.right quality: ________________ )Disturbance of auditory acuity:1.no 2.yes(1.left 2.right description: _____ ) Nose:Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no 2.yes(quality _____ ) Tenderness over paranasal sinuses:1.no 2.yes (location: ______________ ) Mouth: Lip _____________ Mucosa ____________ T ongue _______________ Teeth:1.normal 2.Agomphiasis 3. Eurodontia 4.others: _____________________Gum :1.normal 2.abnormal (Description __________________________ )Tonsil: __________________________ Pharynx: _____________________Sound: 1.normal 2.hoarseness 3.others: ____________________________ Neck:Neck rigidity 1.no 2.yes ( _____________ transvers fingers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distentionTrachea location:1.middle 2.deviation (1.leftward ________ 2.rightward ____ ) Hepatojugular vein reflux: 1. negative 2.positiveThyroid: 1.normal 2.enlarged ______ 3.bruit (1.no 2.yes _______________ )Chest:Chest wall: 1.normal 2.barrel chest 3.prominence or retraction: (left _______ right ___________ P recordial prominence _____________________ ) Percussion pain over sternum1.No 2.YesBreast: 1.Normal 2.ab no rmal _____________________________________Lung: Inspection: respiratory movement 1.normal 2.abnormal ___________ Palpation: vocal tactile fremitus:1. no rmal 2.ab no rmal ____________pleural rubb ing sen sati on :1. no 2.yes ___________________Subcuta neous crepitus sen sati on :1. no 2.yes _____________ Percussion:1resonance 2. Hyperresonance &location _____________3 Flatness&location ________________________________4. dulln ess & location: _____________________________5. tympa ny &location: _____________________________lower border of lung: (detailed percussi on in respiratory disease)midclavicular line : R: ____ i n tercostae L: ____ in tercostaemidaxillary line: R: _______ i n tercostae L: ____ in tercostaescapular li ne: R: ________ i n tercostae L: ____ in tercostaemoveme nt of lower borders:R: ______ cmL: _________ c m Auscultation: Breath ing sound : 1.no rmal 2.ab no rmal ___________Rales:1. no 2.yes _________________________________ Heart: lnspection:Apical pulsation: 1.normal 2.unseen 3.increase 4.diffuseSubxiphoid pulsation: 1.no 2.yesLocati on of apex beat: 1. no rmal 2.shift ( _____in tercosta,dista nee away from left MCL ____ cm) Palpation:Apical pulsation:1. normal 2.lifting apex impulse 3.negative pulsationThrill:1. no 2.yes(location: __________ phase: ________________ )Percussion relative dullness border: 1.normal 2.abnormal(Dista nee betwee n An terior Medli ne and left MCL ____ cm) Auscultation: Heart rate: __bpm Rhythm:1.regular 2.irregular ______Heart sound: 1.no rmal 2.abnormal ______________________Extra sound: 1.no 2.S3 3.® 4. opening snapP2 ____________ A _________ Pericardial frictio n soun d:1. no 2.yesMurmur: 1.no 2.yes (location ___________ phase ___________quality _____ i ntensity ________ tran smissio n _________effects of position ________________________________effects of respiration _____________________________Peripheral vascular signs1.None2.paradoxical pulse3.pulsus alternans4. Water hammer pulse5.capillary pulsation6.pulse deficit7.Pistol shot sound8.DuroziezsignAbdomen:Inspection:Shape: 1.normal 2.protuberance 3.scaphoid 4.frog-belly Gastricpattern 1.no 2.yes Intestinal pattern 1.no 2.yesAbdominal vein varicosis 1.no 2.yes(direction: _____________ )Operation scar1.no 2.yes _______________________________ Palpation: 1.soft 2. tensive (location:_____________________________ )Tenderness: 1.no 2.yes(location: _____________________ )Rebound tenderness:1.no 2.yes(location: _______________ )Fluctuation: 1.present 2.abscentSuccussion splash: 1.negative 2.positiveLiver: ______________________________________________Gallbladder:____________________ ______ M urphy sign: ___________Spleen:____________________Kidneys: _____________Abdominal mass: ______Others: _____________________________________________ Percussion:Liver dullness border: 1.normal 2.decreased 3.absentUpper hepatic border:Right Midclavicular Line _______ IntercostaShift dullness:1.negative 2.positive Ascites: _____________ degreePain on percussion in costovertebral area: 1.negative 2.positve ___ Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis 3.hypoperistalsis4.absence Gurgling sound:1.no 2.yesVascular bruit 1.no 2.yes (location ___________________ ) Genital organ: 1.unexamined 2.normal 3.abnormalAnus and rectum: 1.unexamined 2.normal 3.abnormalSpine and extremities:Spine: 1.normal 2.deformity (1.kyphosis 2.lordosis 3.scoliosis)3.Tenderness(location _____________________________ )Extremities: 1.normal 2.arthremia & arthrocele (location _________________ )3.Ankylosis (location __________ )4.Aropachy: 1.no 2.yes5.Muscular atrophy (location ______________________ ) Neurological system1:.normal 2.abnormal ______________________________Important examination results before hospitalized Summary of the history: _____________________________________Initial diagnosis: ____________________________________________Recorder:Corrector:。
病历书写(英文)

A. Outline of case record
1. Biographical data Biographical information of patient should include his full name, age (date of birth), sex, race, occupation, nationality, marital status and permanent home address. Also, the date of admission, the time at which you took the history, the source of history and estimate of reliability should be involved. 2. chief complaint The chief complaint consists of main symptom(s) and duration. It should constitute in a few simple words the main reasons why the patient consulted doctor and should be state as nearly as possible in the patient’s own wards. In general, the chief complaint should include age, sex, complaint, and duration of the complaint. It should no included diagnostic terms or disease entities. For example:” This 70-year old man has had short breath for a week.”
住院病历英文作文
住院病历英文作文英文:I recently had to be hospitalized for a few days due toa severe case of pneumonia. During my stay, I had to keep a detailed record of my symptoms, medications, and treatments. This record is commonly known as a hospital or medical record.Hospital records are important because they provide a complete history of a patient's medical condition,including diagnoses, treatments, and outcomes. They arealso used to communicate important information between healthcare providers and ensure that patients receive the appropriate care.In my case, my hospital record included information about my vital signs, such as my temperature, blood pressure, and heart rate. It also included details about my symptoms, such as my cough, chest pain, and shortness ofbreath. Additionally, it listed all of the medications Iwas taking and the dosages, as well as any treatments or procedures I received.Overall, my hospital record was a comprehensive document that provided a clear picture of my medical condition during my hospital stay. It was an essential tool for my healthcare team to ensure that I received the best possible care.中文:最近,我因为严重的肺炎住院了几天。
英文病历报告作文模板
英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。
英文病历书写范例
英文病历书写范例(内科)Medical Records for AdmissonMedical Number: 701721General informationName: Liu SideAge: EightySex: MaleRace: HanNationality: ChinaAddress: NO.35, Dandong Road, Jiefang Rvenue, Hankou, Hubei.Tel: 857307523Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history:patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for fo ur hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought heha date something wrong. At 6 o’cloc k this morning he fainted and rejected lots of blood and gore. T hen hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”. Since the disease coming on, the patient didn’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past history Operative history: Never undergoing any operation. Infectious history: No history of s evere infectious disease. Allergic history: He was not allergic to penicillin or sulfamide. Respirator y system: No history of respiratory disease. Circulatory system: No history of precordial pain. Ali mentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding. Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural sys tem: No history of headache or dizziness. Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living condition s were good. No bad personal habits and customs.Menstrual history: He is a male patient. Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads. Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished.Active position. His consciousness was not clear. His face was cadaverous and the skin was not sta ined yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pi tting edema. Superficial lymph nodes were not found enlarged. HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No ten derness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external au ditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nare s flaring. No tenderness in nasal sinuses. Eye: Bilateral eyelids were not swelling. No ptosis. No e ntropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or dep ressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect p upillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in mi dline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was nei ther narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast: Symmetric bilaterally.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic e xpansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales. Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum imp ulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardi al friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal ty pe or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. T here was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular mur murs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/L History summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph node s were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill ne gative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs. 5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhage Exsanguine shock出院小结(DISCHARGE SUMMARY), ===============Department of GastroenterologyChanghai Hospital,No.174 Changhai Road Shanghai, China Phone: 86-21-25074725-803 DISCHARGE SUMMARYDA TE OF ADMISSION: October 7th, 2005 DA TE OF DISCHARGE: October 12th, 2005 ATTE NDING PHYSICIAN: Yu Bai, MD PA TIENT AGE: 18ADMITTING DIAGNOSIS:V omiting for unknown reason: acute gastroenteritis?BRIEF HISTORYA 18-year-old female with a complaint of nausea and vomiting for nearly one month who was see n at Department of Gastroenterology in Changhai Hospital, found to have acute gastroenteritis and non-atrophic gastritis. The patient was subsequently recovered and discharged soon after medicati on.REVIEW OF SYSTEMShe has had no headache, fever, chills, diarrhea, chest pain, palpitations, dyspnea, cough, hemopty sis, dysuria, hematuria or ankle edema.PAST MEDICAL HISTORYShe has had no previous surgery, accidents or childhood illness.SOCIAL HISTORY: She has no history of excessive alcohol or tobacco use.FAMIL Y HISTORYShe has no family history of cardiovascular, respiratary and gastrointestinal diseases. PHYSICAL EXAMINA TIONTemperature is 37, pulse 80, respirations 16, blood pressure 112/70. General: Plump girl in no app arent distress. HEENT: She has no scalp lesions. Her pupils are equally round and reactive to light and accommodation. Extraocular movements are intact. Sclerae are anicteric. Oropharynx is clear. There is no thyromegaly. There is no cervical or supraclvicular lymphadenopathy. Cardiovascular: Regular rate andrhythm, normal S1, S2. Chest: Clear to auscultation bilateral. Abdomen: Bowel sounds present, no hepatosplenomagaly. Extremities: There is no cyanosis, clubbing or edema. Neurologic: Cranial n erves II-XII are intact. Motor examination is 5/5 in the bilateral upper and lower extremities. Sens ory, cerebellar and gait are normal.LABORATORY DATAWhite blood cells count 5.9, hemoglobin 111g/L, hematocrit 35.4. Sodium 142, potassium 4.3, chl oride 106, CO2 25, BUN 2.6mmol/L, creatinine 57μmol/L, glucose 4.1mmol/L, Albumin 36g/L. Endoscopic ExamChronic non-atrophic gastritisHOSPITAL COURSEThe patient was admitted and placed on fluid rehydration and mineral supplement. The patient im proved, showing gradual resolution of nausea and vomiting. The patient was discharged in stable c ondition.DISCHARGE DIAGNOSIS Acute gastroenteritisChronic non-atrophic gastritisPROGNOSISGood. No medications needed after discharge. But if this patient can not get used to Chinese food, she had better return to UK as soon as possible to prevent the relapse of acute gastroenteritis. The patient is to follow up with Dr. Bai in one week. ___________________________ Yu Bai, MD D: 12/10/2005。
英语病历范文
英语病历范文Patient Information:- Name: [Not Specified]- Age: [Not Specified]- Date: [Not Specified]- Doctor: [Not Specified]Chief Complaint:The patient presents with a persistent cough, accompanied by mild fever and body aches for the past three days.History of Present Illness:The patient first noticed the symptoms on [Date], with a dry cough that gradually worsened. The fever started as low-grade but has been increasing, reaching up to 38.5 degrees Celsius.Past Medical History:The patient has no significant past medical history. No previous hospitalizations or chronic illnesses are reported.Medications:The patient has not taken any medications for the current illness, nor are they on any regular medication.Allergies:No known allergies to medications or environmental factors.Physical Examination:Vital signs: Temperature 38.3°C, Puls e 92 bpm, Respiratory rate 20 breaths per minute, Blood pressure 120/80 mmHg. The patient appears fatigued but in no acute distress. Lungs are clear to auscultation with no wheezing or crackles. The throat is slightly red without exudates.Assessment:Based on the symptoms and physical examination, the patient is likely suffering from a viral upper respiratory infection.Plan:1. Hydration and rest are recommended.2. Over-the-counter fever reducers and cough suppressants may be used as needed for symptomatic relief.3. If symptoms persist or worsen, the patient should return for further evaluation and potential testing for influenza or COVID-19.Follow-up:The patient is advised to follow up in one week if symptoms have not improved or if new symptoms develop.Instructions:- Increase fluid intake to prevent dehydration.- Avoid contact with others to prevent the spread of the infection.- Monitor for signs of worsening condition, such as difficulty breathing, persistent high fever, or chest pain.Note: This is a hypothetical patient case and should not be used as a substitute for professional medical advice, diagnosis, or treatment.。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
医学英语病历书写范文住院病历书写的范文中医(中西医结合)病历书写范文住院病历姓名:. 性别:男年龄:5岁民族:. 出生地: .婚况:未婚职业:. 单位:. 邮政编码:..常住地址:...入院时间:xx年4月13日10时病史采集时间:xx年4月13日10时病史陈述者:患儿母亲可靠程度:基本可靠发病节气:清明后主诉:反复发热、咳嗽5天现病史:缘患儿5天前无明显诱因下开始出现发热,咳嗽,有痰,鼻塞,呕吐胃内容物一次,曾多次到我院门诊求治,予中药及静滴先锋VI、鱼腥草治疗,症状未见改善。
于今天再次来我院门诊求治,为求进一步系统治疗,遂由门诊收入院。
入院时症见:患儿精神疲倦,发热,咳嗽,有痰,无气促,呕吐胃内容物一次,耳痛,无耳鸣,纳呆,睡眠差,大便烂,日三次,小便调。
既往史:既往健康,否认水痘,麻疹,结核,肝炎病史。
个人史:母孕期健康,足月顺产,第一胎,出生时体重、身高不详。
出生时无窒息、缺氧史,无病理性黄疸,混合喂养,按时添加辅食,生长发育正常,智力正常,按时预防接种。
过敏史:自诉清开灵过敏史,否认其他食物及药物过敏史。
月经婚育史:家族史:父母健康。
否认家族遗传病史。
体格检查T 37℃ P 92次/分 R 20次/分 bp整体状况:望神:神志清楚,精神疲倦,表情正常。
望色:正常面容,色泽偏白。
望形:发育正常,营养一般,体型偏瘦。
望态:体位正常,姿势自然,步态正常。
声音:语言清晰,语言强弱适中,咳嗽,无呃逆、嗳气、哮鸣、呻吟等异常声音。
气味:无特殊气味。
舌象:舌红,苔白。
脉象:脉浮数。
皮肤、粘膜及淋巴结:皮肤粘膜:皮肤粘膜无黄染,纹理、弹性等均正常,皮肤稍热,无汗,无斑疹、疮疡、疤痕、肿物,无腧穴异常征、血管征、蜘蛛痣、色素沉着等,无皮肤划痕征。
淋巴结:双颌下各可扪及花生米大小淋巴结,表面光滑,无压痛,活动度好,无粘连。
头面部:头颅:头颅正常无畸形、肿物、压痛,头发疏密、色泽、分布均正常,无疖、癣、疤痕。
眼:眉毛、睫毛、眼睑、眼球正常,眼结膜轻微充血,巩膜无黄染,角膜清晰,双瞳孔等大等圆,直径2.5mm,对光反应灵敏。
耳:耳廓正常无畸形,外耳道通畅,无异常分泌物,乳突无压痛,听力正常。
鼻:无畸形、鼻中隔居中,无穿孔,无鼻甲肥大或阻塞,无鼻腔异常分泌物,副鼻窦无压痛,嗅觉正常。
口腔:口唇红,无疱疹、皲裂、溃疡,牙齿正常,齿龈无出血或肿胀,口腔粘膜无疱疹、出血、溃疡,咽充血(+++),双侧扁桃体II0肿大,腭垂居中。
颈部:形:对称,无异常肿块。
态:无抵抗强直、压痛,活动无受限。
气管:位置居中。
甲状腺:无肿大或结节。
颈脉:无异常搏动及杂音,颈静脉无怒张,无肝颈回流征。
胸部:胸廓:外观对称,无畸形,肋间隙正常,无局部隆起、凹陷、压痛及叩击痛,无水肿、皮下气肿、肿块,静脉无怒张及回流异常。
乳房:大小正常,无红肿压痛。
肺:呼吸正常,双侧呼吸活动度正常,语颤正常,双肺叩诊清音,肺肝浊音界、肺下界、呼吸时肺下缘移动度均正常。
双肺呼吸音清,双肺未闻及干湿性啰音,语音传导无异常。
无胸膜摩擦音、哮鸣音。
心:心尖搏动位于第4、5肋间左锁骨中线内0.5cm,无负性心尖搏动及心前区弥散性搏动,无震颤或摩擦感,心脏左右浊音界如右图。
心脏搏动节律整,心率92次/分,心音正常,各瓣膜听诊区未闻及病理性杂音。
血管:动脉:桡动脉的频率、节律均规则正常,无奇脉。
股动脉及肱动脉无抢击音。
周围血管:无毛细血管搏动征,无射枪音,无水冲脉,无动脉异常搏动,Duroziez氏征(-)。
腹部:视诊:腹部对称,大小正常,呼吸运动正常,无膨隆、凹陷,无皮疹、色素沉着、条纹、疤痕、脐疝、静脉曲张、胃肠蠕动波。
触诊:腹部柔软,无压痛、反跳痛,不拒按。
叩诊:鼓音,无移动性浊音和包块。
听诊:肠鸣音正常,无气过水声,无血管杂音。
肝脏:肋下未触及,肝区无压痛。
胆囊:未触及,胆囊区无压痛。
脾脏:未触及,脾区无压痛。
肾脏:双肾无叩击痛,无腰酸痛。
膀胱:未触及,输尿管无压痛点。
二阴及排泄物:二阴:前后二阴正常。
排泄物:未查。
脊柱四肢:脊柱:生理曲度存在,无畸形、强直、叩压痛,运动度不受限、两侧肌肉无紧张、压痛。
四肢:肌力、肌张力均正常,无外伤、骨折、肌萎缩。
关节无红肿、疼痛、压痛、积液、脱臼,活动度正常,无畸形,下肢无水肿、静脉曲张。
指趾甲:指趾甲红润,光泽,形状正常。
神经系统:感觉:痛觉、温度觉、触觉、音叉振动觉及关节位置觉都正常。
运动:肌肉无紧张及萎缩,无瘫痪,无不正常的动作,共剂运动及步态正常。
浅反射:腹壁反射、跖反射正常,提睾反射和肛门反射未查。
深反射:二、三头肌反射,桡骨膜反射,膝腱反射及跟腱反射正常。
病理反射:Hoffmann (-), Babinski (-), Gordon (-), Chaddock (-), Kernig (-)。
实验室检查:血分析:WBC 12.6x10e9/L, GRAN%76.2% 。
胸片示:双肺支气管感染。
辨病辨证依据:四诊合参,本病当属祖国医学之“咳嗽”范畴,证属“风热型”。
缘患儿年幼,肺气虚弱,为风热之邪所袭,邪闭肺络,肺气失于宣肃,腠理开合失度,可致发热,咳嗽。
鼻咽为肺胃之门,感受风热之邪故见咽红。
肺与脾密切相关,肺气受损则脾气亦虚,故见纳呆,胃失和降则呕吐,运化失常则大便烂。
舌红,苔白,脉浮数均为外感风热之征。
西医诊断依据:1.病史:反复发热、咳嗽5天。
2.症状、体征:发热,咳嗽,有痰,呕吐胃内容物一次,耳痛,纳呆,睡眠差,大便烂。
咽充血(+++),双扁桃体II°大。
双肺呼吸音粗,双下肺可闻及少量干湿性罗音。
3、辅助检查:血分析:WBC 12.6x10e9/L, GRAN%76.2%,胸片示:双肺支气管感染。
入院诊断中医诊断:咳嗽风热型西医诊断:急性支气管炎实习医师:住院医师:中医(中西医结合)病历书写范文住院病历姓名:. 性别:男年龄:5岁民族:. 出生地: .婚况:未婚职业:. 单位:. 邮政编码:..常住地址:...入院时间:xx年4月13日10时病史采集时间:xx年4月13日10时病史陈述者:患儿母亲可靠程度:基本可靠发病节气:清明后主诉:反复发热、咳嗽5天现病史:缘患儿5天前无明显诱因下开始出现发热,咳嗽,有痰,鼻塞,呕吐胃内容物一次,曾多次到我院门诊求治,予中药及静滴先锋VI、鱼腥草治疗,症状未见改善。
于今天再次来我院门诊求治,为求进一步系统治疗,遂由门诊收入院。
入院时症见:患儿精神疲倦,发热,咳嗽,有痰,无气促,呕吐胃内容物一次,耳痛,无耳鸣,纳呆,睡眠差,大便烂,日三次,小便调。
既往史:既往健康,否认水痘,麻疹,结核,肝炎病史。
个人史:母孕期健康,足月顺产,第一胎,出生时体重、身高不详。
出生时无窒息、缺氧史,无病理性黄疸,混合喂养,按时添加辅食,生长发育正常,智力正常,按时预防接种。
过敏史:自诉清开灵过敏史,否认其他食物及药物过敏史。
月经婚育史:家族史:父母健康。
否认家族遗传病史。
体格检查T 37℃ P 92次/分 R 20次/分 bp整体状况:望神:神志清楚,精神疲倦,表情正常。
望色:正常面容,色泽偏白。
望形:发育正常,营养一般,体型偏瘦。
望态:体位正常,姿势自然,步态正常。
声音:语言清晰,语言强弱适中,咳嗽,无呃逆、嗳气、哮鸣、呻吟等异常声音。
气味:无特殊气味。
舌象:舌红,苔白。
脉象:脉浮数。
皮肤、粘膜及淋巴结:皮肤粘膜:皮肤粘膜无黄染,纹理、弹性等均正常,皮肤稍热,无汗,无斑疹、疮疡、疤痕、肿物,无腧穴异常征、血管征、蜘蛛痣、色素沉着等,无皮肤划痕征。
淋巴结:双颌下各可扪及花生米大小淋巴结,表面光滑,无压痛,活动度好,无粘连。
头面部:头颅:头颅正常无畸形、肿物、压痛,头发疏密、色泽、分布均正常,无疖、癣、疤痕。
眼:眉毛、睫毛、眼睑、眼球正常,眼结膜轻微充血,巩膜无黄染,角膜清晰,双瞳孔等大等圆,直径2.5mm,对光反应灵敏。
耳:耳廓正常无畸形,外耳道通畅,无异常分泌物,乳突无压痛,听力正常。
鼻:无畸形、鼻中隔居中,无穿孔,无鼻甲肥大或阻塞,无鼻腔异常分泌物,副鼻窦无压痛,嗅觉正常。
口腔:口唇红,无疱疹、皲裂、溃疡,牙齿正常,齿龈无出血或肿胀,口腔粘膜无疱疹、出血、溃疡,咽充血(+++),双侧扁桃体II0肿大,腭垂居中。
颈部:形:对称,无异常肿块。
态:无抵抗强直、压痛,活动无受限。
气管:位置居中。
甲状腺:无肿大或结节。
颈脉:无异常搏动及杂音,颈静脉无怒张,无肝颈回流征。
胸部:胸廓:外观对称,无畸形,肋间隙正常,无局部隆起、凹陷、压痛及叩击痛,无水肿、皮下气肿、肿块,静脉无怒张及回流异常。
乳房:大小正常,无红肿压痛。
肺:呼吸正常,双侧呼吸活动度正常,语颤正常,双肺叩诊清音,肺肝浊音界、肺下界、呼吸时肺下缘移动度均正常。
双肺呼吸音清,双肺未闻及干湿性啰音,语音传导无异常。
无胸膜摩擦音、哮鸣音。
心:心尖搏动位于第4、5肋间左锁骨中线内0.5cm,无负性心尖搏动及心前区弥散性搏动,无震颤或摩擦感,心脏左右浊音界如右图。
心脏搏动节律整,心率92次/分,心音正常,各瓣膜听诊区未闻及病理性杂音。
血管:动脉:桡动脉的频率、节律均规则正常,无奇脉。
股动脉及肱动脉无抢击音。
周围血管:无毛细血管搏动征,无射枪音,无水冲脉,无动脉异常搏动,Duroziez氏征(-)。
腹部:视诊:腹部对称,大小正常,呼吸运动正常,无膨隆、凹陷,无皮疹、色素沉着、条纹、疤痕、脐疝、静脉曲张、胃肠蠕动波。
触诊:腹部柔软,无压痛、反跳痛,不拒按。
叩诊:鼓音,无移动性浊音和包块。
听诊:肠鸣音正常,无气过水声,无血管杂音。
肝脏:肋下未触及,肝区无压痛。
胆囊:未触及,胆囊区无压痛。
脾脏:未触及,脾区无压痛。
肾脏:双肾无叩击痛,无腰酸痛。
膀胱:未触及,输尿管无压痛点。
二阴及排泄物:二阴:前后二阴正常。
排泄物:未查。
脊柱四肢:脊柱:生理曲度存在,无畸形、强直、叩压痛,运动度不受限、两侧肌肉无紧张、压痛。
四肢:肌力、肌张力均正常,无外伤、骨折、肌萎缩。
关节无红肿、疼痛、压痛、积液、脱臼,活动度正常,无畸形,下肢无水肿、静脉曲张。
指趾甲:指趾甲红润,光泽,形状正常。
神经系统:感觉:痛觉、温度觉、触觉、音叉振动觉及关节位置觉都正常。
运动:肌肉无紧张及萎缩,无瘫痪,无不正常的动作,共剂运动及步态正常。
浅反射:腹壁反射、跖反射正常,提睾反射和肛门反射未查。
深反射:二、三头肌反射,桡骨膜反射,膝腱反射及跟腱反射正常。
病理反射:Hoffmann (-), Babinski (-), Gordon (-), Chaddock (-), Kernig (-)。
实验室检查:血分析:WBC 12.6x10e9/L, GRAN%76.2% 。
胸片示:双肺支气管感染。
辨病辨证依据:四诊合参,本病当属祖国医学之“咳嗽”范畴,证属“风热型”。
