盐酸莫西沙星氯化钠的用法用量及注意事项
拜复乐(盐酸莫西沙星片)使用说明

拜复乐(盐酸莫西沙星片)【用法用量】剂量范围任何适应症均推荐口服莫西沙星片一次0.4g(1片),一日1次。
成年人服用方法片剂以水送服,服用时间不受饮食影响。
治疗时间治疗时间应根据症状的严重程度或临床反应决定。
治疗上呼吸道和下呼吸道感染时可按照下列方法:慢性支气管炎急性发作:5天社区获得性肺炎:10天急性窦炎:7天治疗皮肤和软组织感染的推荐治疗时间为7天。
莫西沙星0.4g片剂在临床试验中最多用过14天疗程。
老年人老年人不必要调整用药剂量。
儿童莫西沙星对儿童和青少年的疗效和安全性尚未确定。
肝损伤肝功能损伤的患者不必调整莫西沙星的剂量(肝功能严重受损Child-PughC的患者见禁忌)。
肾功能异常任何程度的肾功能受损的患者(包括肌酐清除宰≤30ml/min/1.73m2)和慢性透析,如血液透析和持续性腹膜透析的患者,均无需调整莫西沙星的剂量。
种族间差别不同种族间不必调整药物剂量。
【注意事项】1.莫西沙星能够延长一些患者心电图的QT间期。
该药应避免用于QT间期延长的患者﹑患有无法纠正的低钾血症患者及接受Ia类(如:奎尼丁,普鲁卡因胺)或III类(如:胺碘酮,索他洛尔)抗心律失常药物治疗的患者。
2.莫西沙星和可能延长QT间期的药物:西沙比利,红霉素,抗精神病药和三环类抗抑郁药,联合用药时可能存在累加效应。
所以,应慎重与这些药物合用。
莫西沙星在致心律失常的条件存在时应慎用,如:严重的心动过缓或急性心肌缺血。
3.和男性相比,由于女性患者往往拥有更长的QTc间期,她们对引发QTc间期延长的药物可能更敏感。
老年患者也更容易遭受药物引发的QT间期延长的影响。
4.QT间期延长的程度随着药物浓度的增加而增加。
所以不应超过推荐剂量。
但是,在肺炎患者中没有观察到莫西沙星血药浓度和QT间期延长相关。
QT间期延长可以导致室性心律失常包括尖端扭转型室速的发生危险增高。
在莫西沙星治疗的超过9000名患者的临床研究中,没有因QT间期延长导致的心血管的发病率或死亡率,但某些潜在条件可以增加室性心律失常的危险。
盐酸莫西沙星氯化钠注射液
盐酸莫西沙星氯化钠注射液【药品名称】通用名称:盐酸莫西沙星氯化钠注射液英文名称:Moxifloxacin Hydrochloride and Sodium Chloride Injection【成份】本品主要成份为盐酸莫西沙星,化学名为:1-环丙基-7-[(s,s)-2,8-重氮-二环[4.3.0]壬-8-基]-6-氟-8-甲氧-1,4-二氢-4-氧-3-11奎啉羧酸盐酸盐。
【适应症】成人(≥18岁)上呼吸道和下呼吸道感染,如:急性窦炎、慢性支气管炎急性发作、社区获得性肺炎;以及皮肤和软组织感染。
【用法用量】400 mg qd,口服或静滴90分钟。
疗程:慢性支气管炎急性发作- 5天;社区获得性肺炎:序贯给药(静脉给药后继续口服用药)总疗程为7-14天;急性鼻窦炎- 7天;皮肤和软组织感染- 7天。
最多14天。
【不良反应】在莫西沙星的临床试验中,绝大多数的不良反应为轻中度(约90%),由于不良反应导致停用莫西沙星治疗的病人为36%,序贯治疗(静脉给药后继续口服用药)为5.7%。
根据莫西沙星的临床试验总结出的常见不良反应列表如下:发生率≥1%<10%全身症状:腹痛、头痛、注射部位反应(如水肿/过敏/炎症/疼痛)心血管系统:合并低血钾症患者QT间期延长消化系统:恶心、腹泻、呕吐、消化不良、肝功能化验异常特殊感官:味觉倒错神经系统:头晕发生率≥0.1%<1%全身症状:乏力、念珠菌病、疼痛、不适、胸痛心血管系统:心动过速、高血压、心悸、QT间期延长、静脉炎(注射部位)消化系统:口干、恶心和呕吐、腹胀、便秘、口腔念珠菌病、食欲下降、口腔炎、胃肠功能失调、舌炎、γGT(γ谷氨酰转肽酶)增高血液和淋巴系统:白细胞减少、凝血酶原减少/国际标准化比值增高、嗜酸细胞增多、血小板增多症代谢和营养:淀粉酶增加骨骼肌肉系统:关节痛、肌肉痛神经系统失眠、眩晕、神经质、嗜睡、焦虑、震颤、感觉异常呼吸系统:呼吸困难皮肤和附件:皮疹、瘙痒、多汗泌尿生殖系统:阴道念珠菌病、阴道炎发生率≥0.01%<0.1%全身症状:骨盆疼、面部浮肿、背疼、实验室检验异常、过敏反应、腿疼心血管系统:低血压、血管扩张、外周性水肿消化系统:胃炎、舌变色、吞咽困难、黄疸(主要为胆汁淤积性)、腹泻(难辨梭菌)血液和淋巴系统:凝血活酶减少、凝血酶原增加/国际标准化比值降低、血小板减少、贫血代谢和营养:高血糖、高血脂、高尿酸血症、LDH(乳酸脱氢酶)增高(与肝功能检查异常有关)骨骼肌肉:关节炎、肌腱异常神经系统:幻觉、人格解体、紧张、动作失调、激动不安、健忘症、失语症、情绪不稳定、睡眠障碍、语言障碍、思维异常、感觉减退、梦异常、惊厥、精神错乱、忧郁症呼吸系统:哮喘皮肤和附件:皮疹(斑丘疹、紫癜、脓泡)、荨麻疹特殊感官:耳鸣、视觉异常、味觉丧失、嗅觉倒错(包括嗅觉倒错,嗅觉减低及嗅觉丧失)、弱视泌尿生殖系统:肾功能异常(肌酐或尿素升高)上市后报道的不良反应:发生率≥0.01%<0.1%心血管系统:晕厥发生率<0.01%过敏性:过敏反应、过敏性休克(可危及生命)、血管性水肿(包括喉头水肿;潜在生命危险)消化系统:伪膜性结肠炎(在极少数病例伴有危及生命的并发症),肝炎(主要为胆汁淤积性)肌肉骨胳系统:肌腱断裂皮肤和附件:斯蒂文斯-约翰逊综合征(Stevens-JohnsonSyndrome)神经系统:精神病反应心血管系统:报道在极少数病例尤其是在有严重的潜在性致心律失常条件的病人出现,包括尖端扭转型室速的室性快速性心律失常和心脏停搏。
2023年关于“盐酸莫西沙星注射液”解析

注意事项
1、致残和潜在的不可逆转的严重不良反应,包括肌腱炎和肌腱断裂、周围神经病变和中枢神经系统的影响:使用氟喹诺酮类 药物(包括盐酸莫西沙星),已有报告在同一患者的身体不同器官系统同时发生致残和潜在的不可逆转的严重不良反应,通 常包括:肌腱炎,肌腱断裂,关节痛,肌痛,周围神经病变和中枢神经系统反应(幻觉,焦虑,抑郁,失眠,严重头痛和错 乱)。这些不良反应可发生在使用盐酸莫西沙星后数小时至数周。任何年龄段的患者,之前没有相关风险因素,均有报告发 生这些不良反应。
由于缺乏这些患者的用药经验,本品应避免用于下列患者:
(1)已知QT间期延长;
(2)室性心律失常,包括尖端扭转型,因为QT间期延长可能导致发生这些状况的风险增加;
(3)持续的心律失常状况,如具有临床显著性的心动过缓和急性心肌缺血;
(4)未治疗的低钾血症或低镁血症;
(5)使用抗心律失常IA类药物(例如,奎尼丁、普鲁卡因胺)或III类药物(例如,胺碘酮、索他洛尔);
用法用量
盐酸莫西沙星氯化钠注射液: 盐酸莫西沙星氯化钠注射液用于感染性疾病的治疗,通用的用法用量如下所示,但必须结合疾病严重程度由临床医生最终确定。 4、给药说明: (1)给药前应检查本品是否有不溶颗粒或变色。应使用澄明,无不溶颗粒的本品。穿刺使用前应对本品进行目视检查,不得使用变色、存在颗粒物质或容器存在破损的 产品。 (2)盐酸莫西沙星氯化钠注射液为静脉注射剂,只能用于静脉滴注,不能用于动脉内、肌内、鞘内注射,不能腹膜内或皮下给药。 (3)由于本品与其他注射液的相容性数据较少,本品中不得加入溶媒或其他药物,也不得使用同根静脉输液管同时输注本品,溶媒或其他药物。如使用同根静脉输液管 或Y型管来连续滴注其他药物,或采用背负式输液,在滴注本品之前和之后,应使用和本品和其他滴注药物相容的注射液冲洗该管路。 (4)当开具盐酸莫西沙星来治疗某种细菌感染时,应告知患者:尽管在疗程早期病情通常会好转,但仍应遵医嘱使用药物。跳过剂量或不完成整个疗程可能会降低紧急 治疗的有效性,增加细菌耐药性形成的可能性,未来将不能使用盐酸莫西沙星或其他抗菌药进行治疗。 5、药物相容性:比例在1:10至10:1之间时,本品与下列静脉注射液相容: (1)0.9%氯化钠注射液,无菌注射用水。 (2)1M氯化钠注射液,10%葡萄糖注射液。 (3)5%葡萄糖注射液,乳酸林格注射液 6、种族差异:对高加索人、日本人、黑人及其他种族人群进行了可能的种族间差别试验,未发现临床相关的药代动力学差别。因此,不同种族间不必调整药物剂量。
来盐酸莫西沙星氯化钠注射液的配伍禁忌
来盐酸莫西沙星氯化钠注射液的配伍禁忌盐酸莫西沙星氯化钠注射液(商品名:拜复乐),黄色澄明液体,规格250ml,是第4代新型8-甲氧基氟喹诺酮类抗菌药物,具有抗菌谱广、抗菌力强、体内分布广、体内药物浓度高、半衰期长、疗效好、不良反应小、与其他抗菌药物无交叉耐药性、几乎无光敏反应等优点。
临床上主要应用于治疗呼吸系统、泌尿生殖系统、皮肤系统等感染性疾病。
在近几年的临床用药过程中,笔者发现盐酸莫西沙星氯化钠注射液与多种药物之间存在配伍禁忌,经混合后,均出现白色浑浊现象或者有晶体析出。
为保证临床用药安全,本文查阅了国内相关文献,对其配伍禁忌进行综述,以供临床合理配伍药品参考,保证患者用药安全。
1 抗感染类药物1.1头孢菌素类与头孢哌酮钠他唑巴坦钠存在配伍禁忌。
有研究报道,头孢哌酮钠他唑巴坦钠组滴注完予更换盐酸莫西沙星氯化钠注射剂组液体5s后,茂菲氏滴管内出现白色浑浊,经摇晃不消失[1]。
1.2青霉素类与氟氯西林钠存在配伍禁忌。
有研究报道,将盐酸莫西沙星氯化钠注射剂与0.9%氯化钠注射液100ml+注射用氟氯西林钠联合应用,盐酸莫西沙星氯化钠注射剂更换注射用氟氯西林钠组液体时,输液管内立即出现乳白色浑浊及絮状物;将两种溶液直接混合,发现混合液立即变为乳白色浑浊液,轻摇晃后不溶解,放置30min后观察乳白色浑浊液未恢复澄清[2]。
1.3利福霉素与注射用利福霉素钠存在配伍禁忌。
有研究报道,将注射用利福霉素钠1.0g溶解于5%葡萄糖250ml,抽取2ml注射用利福霉素钠溶液,再抽取2ml 盐酸莫西沙星氯化钠注射剂,将两者混合,或更换两者顺序抽取,混合液均立即出现红色絮状混浊物,剧烈振荡后无变化[3]。
1.4米卡芬净钠与注射用米卡芬净钠存在配伍禁忌。
有研究报道,盐酸莫西沙星氯化钠注射剂输注完毕更换米卡芬净钠时,输液器内溶液呈现乳黄色混浊并有絮状物[4]。
1.5夫西地酸钠与注射用夫西地酸钠存在配伍禁忌。
有研究报道,用20ml 注射器分别抽取夫西地酸钠和莫西沙星注射液各5ml。
莫西沙星服用方法
莫西沙星服用方法莫西沙星是一种常见的抗生素药物,常用于治疗感染性疾病。
正确的使用方法对于药效的发挥和治疗效果至关重要。
下面将为您介绍莫西沙星的服用方法。
1. 用药时间,莫西沙星一般每日2次,每次12小时,最好在饭后服用。
如果您错过了一次服用,尽快补上,但如果离下一次服用时间不到4小时,就不要服用忘记的那一次,以免造成药物浓度过高。
2. 用药剂量,一般情况下,成人每次口服莫西沙星250-500mg,儿童根据体重和病情确定剂量。
请严格按照医生的建议和处方用药,不要随意增减剂量。
3. 服用方法,莫西沙星通常是口服的药物,可以用水送服。
如果您有胃肠道不适,可以在饭后服用,以减轻不适感。
另外,莫西沙星不宜与奶制品一同服用,因为奶制品中的钙离子会影响药物的吸收。
4. 注意事项,在服用莫西沙星期间,应避免饮酒,因为酒精会影响药物的代谢和排泄,增加药物的毒副作用。
同时,莫西沙星也会增加对阳光的敏感度,所以在用药期间应避免暴晒,并做好防晒措施。
5. 用药期间的饮食,在服用莫西沙星期间,应避免食用刺激性食物,如辛辣食物、烟酒等,以免刺激胃肠道,影响药效。
多食用清淡易消化的食物,保持充足的水分摄入,有助于减轻药物对胃肠道的刺激。
6. 用药期间的注意事项,在服用莫西沙星期间,如出现过敏反应、消化道不适、皮肤瘙痒等不良反应,应立即停药并就医。
同时,不要随意更改用药方案,必须在医生的指导下进行用药。
总之,正确的莫西沙星服用方法对于治疗感染性疾病至关重要。
在用药期间,务必严格按照医生的建议用药,避免饮酒、暴晒,注意饮食卫生,如有不良反应应及时就医。
希望您能根据以上建议正确使用莫西沙星,祝您早日康复!。
拜复乐(莫西沙星)
【药品名称】通用名称:拜复乐商品名称:拜复乐【英文名称】汉语拼音:baifule【成份】盐酸莫西沙星氯化钠【性状】本品为黄色的澄明液体【作用类别】【适应症】成人(大于18岁)上呼吸道和下呼吸道感染,如,急性窦炎,慢性支气管炎急性发作,社区获得性肺炎,及皮肤及软组织感染。
【规格】250ml:0.4g × 1【用法用量】推荐剂量一次400mg,一日一次,慢性支气管炎急性发作:5天。
社区获得性肺炎:序贯给药推荐总疗程为7—14天。
急性窦炎:7天。
治疗皮肤及软组织感染的推荐为7天。
【不良反应】绝大多数不良反应为轻中度胃肠道反应,中枢神精系统不良反应,皮肤过敏等【禁忌】已知对该注射液的任何成份或其他喹诺酮类过敏者。
禁用于儿童,青少年,孕妇及哺乳期妇女。
【药物毒理】莫西沙星是具有广谱活性和杀菌作用的8—甲氧基氟喹诺酮类药物。
莫西沙星在体外显示对革兰阳性菌,革兰阴性菌,厌氧菌,抗酸菌和非典型微生物和支原体,衣原体和军团菌具有广谱抗菌活性。
杀菌作用机制为干扰拓扑异构酶Ⅱ和Ⅳ。
拓朴异构酶是控制DNA拓朴和在DNA复制,修复和转录中关键的酶。
【贮藏】干燥条件下贮藏。
【包装】瓶批准文号:国药准字J20040068生产企业:德国拜耳(拜耳医药保健分装)处方类型:本品为处方药!基本药理本品是广谱和具有抗菌活性的8-甲氧基氟喹诺酮类抗菌药。
抗菌机制为干扰II、IV拓扑异构酶。
本品是具有浓度依赖性的杀菌活性。
临床用途本品适应症为治疗患有上呼吸道和下呼吸道感染的成人,如急性窦炎,慢性支气管炎急性发作,社区获得性肺炎,以及皮肤和软组织感染给药途径及用量任何适应症推荐一次400mg,一日一次,服用时间不受饮食影响治疗时间:慢性支气管炎急性发作:5天;社区获得性肺炎:10天;急性窦炎:7天;治疗皮肤和软组织感染推荐治疗时间为7天药物相互作用抗酸药、矿物质和多种维生素同服,本品会形成多价螯合而减少药物吸收,因此抗酸药、含镁、铝和其它矿物质如铁等制剂需服用本品4小时前或2小时后慎与下列药物合用:1a类(如奎宁丁普鲁卡因)或III类(如胺碘酮索托落尔)抗心律失常药西沙必利红霉素抗精神病药物和三环类抗抑郁药食物和乳制品:食物的摄入不影响莫西沙星的吸收因此莫西沙星的服用时间不受进食的影响抗酸药矿物质和多种维生素:莫西沙星与抗酸药矿物质和多种维生素同时服用会因为与这些物质形成多价螯合物而减少药物的吸收这将导致血浆中的药物浓度比预定值低因此抗酸药抗逆转录病毒和其他含有镁铝和其他矿物质如铁等的制剂需要在口服莫西沙星4小时前或2小时后服用雷尼替丁:与雷尼替丁同时服用不会影响莫西沙星的吸收特性其吸收参数(CmaxTmaxAUC)均提示莫西沙星不受胃酸缺乏的影响钙补充剂:当给予高剂量补充剂时仅观察到吸收率稍有减少而吸收范围保持不变高剂量钙补充剂对莫西沙星的吸收不具有临床意义茶碱:莫西沙星对稳态时茶碱的药代动力学无影响提示莫西沙星对P450酶的1A2亚型无影响当服用莫西沙星治疗时达到稳态的茶碱浓度未升高因此服用莫西沙星时不必调整茶碱的用量华法令:据观察莫西沙星与华法令同时服用未发现对凝血酶原时间和凝血的其他参数有影响口服避孕药:莫西沙星与口服避孕药同时服用未发现有相互作用抗糖尿病药:优降糖和莫西沙星同时服用未发现有相互作用伊曲康唑:莫西沙星与伊曲康唑同时服用时伊曲康唑的药时曲线下面积(AUC)仅少量改变伊曲康唑对莫西沙星的药代动力学无显著性影响当服用伊曲康唑时给予莫西沙星不需要调整剂量反之亦然地高辛:莫西沙星对地高辛的药代动力学没有严重影响反之亦然吗啡:肠外给予吗啡同时服用莫西沙星并不减少口服莫西沙星的生物利用度且Cmax(17%)仅稍有下降普鲁苯辛:在一项观察普鲁苯辛对肾脏排泄功能影响的研究中未发现对莫西沙星的全身清除和肾脏清除有明显影响因此当这两种药同时服用时不必调整剂量炭:同时口服炭及400 mg莫西沙星能减少药物的全身利用在体内能阻止80%药物吸收药物过量时利用活性炭能在吸收早期阻止药物的进一步进入全身系统注意事项1.喹诺酮药物使用可诱发癫痫的发作,因此此类病人服用本品要注意2.本品应避免用QT间期延长的患者。
来盐酸莫西沙星氯化钠注射液的配伍禁忌

来盐酸莫西沙星氯化钠注射液的配伍禁忌作者:周爽罗珍利来源:《医学信息》2015年第13期盐酸莫西沙星氯化钠注射液(商品名:拜复乐),黄色澄明液体,规格250ml,是第4代新型8-甲氧基氟喹诺酮类抗菌药物,具有抗菌谱广、抗菌力强、体内分布广、体内药物浓度高、半衰期长、疗效好、不良反应小、与其他抗菌药物无交叉耐药性、几乎无光敏反应等优点。
临床上主要应用于治疗呼吸系统、泌尿生殖系统、皮肤系统等感染性疾病。
在近几年的临床用药过程中,笔者发现盐酸莫西沙星氯化钠注射液与多种药物之间存在配伍禁忌,经混合后,均出现白色浑浊现象或者有晶体析出。
为保证临床用药安全,本文查阅了国内相关文献,对其配伍禁忌进行综述,以供临床合理配伍药品参考,保证患者用药安全。
1 抗感染类药物1.1头孢菌素类与头孢哌酮钠他唑巴坦钠存在配伍禁忌。
有研究报道,头孢哌酮钠他唑巴坦钠组滴注完予更换盐酸莫西沙星氯化钠注射剂组液体5s后,茂菲氏滴管内出现白色浑浊,经摇晃不消失[1]。
1.2青霉素类与氟氯西林钠存在配伍禁忌。
有研究报道,将盐酸莫西沙星氯化钠注射剂与0.9%氯化钠注射液100ml+注射用氟氯西林钠联合应用,盐酸莫西沙星氯化钠注射剂更换注射用氟氯西林钠组液体时,输液管内立即出现乳白色浑浊及絮状物;将两种溶液直接混合,发现混合液立即变为乳白色浑浊液,轻摇晃后不溶解,放置30min后观察乳白色浑浊液未恢复澄清[2]。
1.3利福霉素与注射用利福霉素钠存在配伍禁忌。
有研究报道,将注射用利福霉素钠1.0g 溶解于5%葡萄糖250ml,抽取2ml注射用利福霉素钠溶液,再抽取2ml 盐酸莫西沙星氯化钠注射剂,将两者混合,或更换两者顺序抽取,混合液均立即出现红色絮状混浊物,剧烈振荡后无变化[3]。
1.4米卡芬净钠与注射用米卡芬净钠存在配伍禁忌。
有研究报道,盐酸莫西沙星氯化钠注射剂输注完毕更换米卡芬净钠时,输液器内溶液呈现乳黄色混浊并有絮状物[4]。
1.5夫西地酸钠与注射用夫西地酸钠存在配伍禁忌。
盐酸莫西沙星氯化钠注射液说明书
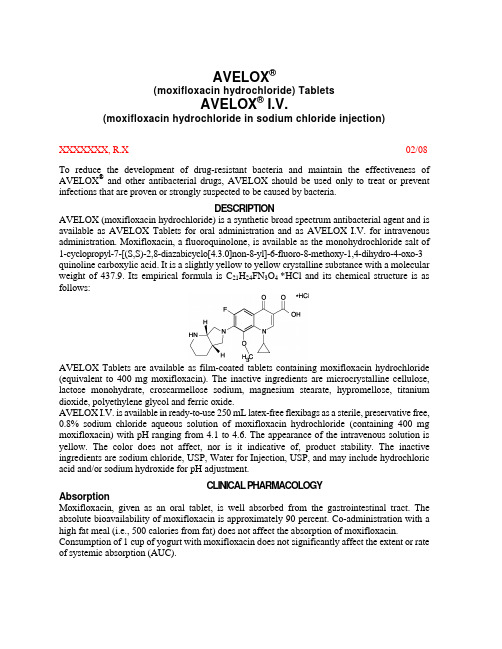
AVELOX®(moxifloxacin hydrochloride) TabletsAVELOX® I.V.(moxifloxacin hydrochloride in sodium chloride injection)XXXXXXX, R.X02/08 To reduce the development of drug-resistant bacteria and maintain the effectiveness of AVELOX® and other antibacterial drugs, AVELOX should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.DESCRIPTIONAVELOX (moxifloxacin hydrochloride) is a synthetic broad spectrum antibacterial agent and is available as AVELOX Tablets for oral administration and as AVELOX I.V. for intravenous administration. Moxifloxacin, a fluoroquinolone, is available as the monohydrochloride salt of 1-cyclopropyl-7-[(S,S)-2,8-diazabicyclo[4.3.0]non-8-yl]-6-fluoro-8-methoxy-1,4-dihydro-4-oxo-3 quinoline carboxylic acid. It is a slightly yellow to yellow crystalline substance with a molecular weight of 437.9. Its empirical formula is C21H24FN3O4 *HCl and its chemical structure is as follows:AVELOX Tablets are available as film-coated tablets containing moxifloxacin hydrochloride (equivalent to 400 mg moxifloxacin). The inactive ingredients are microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate, hypromellose, titanium dioxide, polyethylene glycol and ferric oxide.AVELOX I.V. is available in ready-to-use 250 mL latex-free flexibags as a sterile, preservative free, 0.8% sodium chloride aqueous solution of moxifloxacin hydrochloride (containing 400 mg moxifloxacin) with pH ranging from 4.1 to 4.6. The appearance of the intravenous solution is yellow. The color does not affect, nor is it indicative of, product stability. The inactive ingredients are sodium chloride, USP, Water for Injection, USP, and may include hydrochloric acid and/or sodium hydroxide for pH adjustment.CLINICAL PHARMACOLOGYAbsorptionMoxifloxacin, given as an oral tablet, is well absorbed from the gastrointestinal tract. The absolute bioavailability of moxifloxacin is approximately 90 percent. Co-administration with a high fat meal (i.e., 500 calories from fat) does not affect the absorption of moxifloxacin. Consumption of 1 cup of yogurt with moxifloxacin does not significantly affect the extent or rate of systemic absorption (AUC).The mean (± SD) C max and AUC values following single and multiple doses of 400 mg moxifloxacin given orally are summarized below.C max (mg/L)AUC(mg•h/L)Half-life(hr)Single Dose OralHealthy (n = 372) 3.1 ± 1.036.1 ± 9.111.5 - 15.6* Multiple Dose OralHealthy young male/female (n = 15) 4.5 ± 0.548.0 ± 2.712.7 ± 1.9 Healthy elderly male (n = 8) 3.8 ± 0.351.8 ± 6.7Healthy elderly female (n = 8) 4.6 ± 0.654.6 ± 6.7Healthy young male (n = 8) 3.6 ± 0.548.2 ± 9.0Healthy young female (n = 9) 4.2 ± 0.549.3 ± 9.5* Range of means from different studiesThe mean (± SD) C max and AUC values following single and multiple doses of 400 mg moxifloxacin given by 1 hour I.V. infusion are summarized below.C max (mg/L)AUC(mg•h/L)Half-life(hr)Single Dose I.V.Healthy young male/female (n = 56) 3.9 ± 0.939.3 ± 8.68.2 - 15.4* Patients (n = 118)Male (n = 64) 4.4 ± 3.7Female (n = 54) 4.5 ± 2.0< 65 years (n = 58) 4.6 ± 4.2≥ 65 years (n = 60) 4.3 ± 1.3Multiple Dose I.V.Healthy young male (n = 8) 4.2 ± 0.838.0 ± 4.714.8 ± 2.2 Healthy elderly (n =12; 8 male, 4 female) 6.1 ± 1.348.2 ± 0.910.1 ± 1.6 Patients** (n = 107)Male (n = 58) 4.2 ± 2.6Female (n = 49) 4.6 ± 1.5< 65 years (n = 52) 4.1 ± 1.4≥ 65 years (n = 55) 4.7 ± 2.7* Range of means from different studies** Expected C max (concentration obtained around the time of the end of the infusion)Plasma concentrations increase proportionately with dose up to the highest dose tested (1200 mg single oral dose). The mean (± SD) elimination half-life from plasma is 12 ± 1.3 hours; steady-state is achieved after at least three days with a 400 mg once daily regimen.Mean Steady-State Plasma Concentrations of Moxifloxacin Obtained With Once Daily Dosing of 400 mg Either Orally (n=10) or by I.V. Infusion (n=12)DistributionMoxifloxacin is approximately 30-50% bound to serum proteins, independent of drug concentration. The volume of distribution of moxifloxacin ranges from 1.7 to 2.7 L/kg. Moxifloxacin is widely distributed throughout the body, with tissue concentrations often exceeding plasma concentrations. Moxifloxacin has been detected in the saliva, nasal and bronchial secretions, mucosa of the sinuses, skin blister fluid, subcutaneous tissue, skeletal muscle, and abdominal tissues and fluids following oral or intravenous administration of 400 mg. Moxifloxacin concentrations measured post-dose in various tissues and fluids following a 400 mg oral or I.V. dose are summarized in the following table. The rates of elimination of moxifloxacin from tissues generally parallel the elimination from plasma.Moxifloxacin Concentrations (mean ± SD) in Tissuesand the Corresponding Plasma Concentrations After a Single 400 mg Oral orIntravenous Dose §Tissue or Fluid NPlasmaConcentration(µg/mL)Tissue or FluidConcentration(µg/mL or µg/g)TissuePlasmaRatio:RespiratoryAlveolar Macrophages5 3.3± 0.761.8± 27.321.2 ± 10.0 Bronchial Mucosa8 3.3± 0.7 5.5± 1.3 1.7 ± 0.3 Epithelial Lining Fluid5 3.3± 0.724.4± 14.78.7 ± 6.1 SinusMaxillary Sinus Mucosa4 3.7± 1.1†7.6± 1.7 2.0 ± 0.3 Anterior Ethmoid Mucosa3 3.7± 1.1†8.8± 4.3 2.2 ± 0.6 Nasal Polyps4 3.7± 1.1†9.8± 4.5 2.6 ± 0.6 Skin, MusculoskeletalBlister Fluid5 3.0± 0.5‡ 2.6± 0.9 0.9 ± 0.2 Subcutaneous Tissue6 2.3± 0.4#0.9± 0.3* 0.4 ± 0.6 Skeletal Muscle6 2.3± 0.4#0.9± 0.2* 0.4 ± 0.1 Intra-AbdominalAbdominal tissue 8 2.9± 0.5 7.6 ± 2.0 2.7 ± 0.8 Abdominal exudate 10 2.3±0.5 3.5 ±1.2 1.6 ± 0.7 Abscess fluid 6 2.7± 0.7 2.3 ±1.5 0.8±0.4§all moxifloxacin concentrations were measured 3 hours after a single 400 mg dose, except the abdominal tissue and exudate concentrations which were measured at 2 hours post-dose and the sinus concentrations which were measured 3 hours post-dose after 5 days of dosing.† N = 5‡N = 7#N = 12* Reflects only non-protein bound concentrations of drug.MetabolismApproximately 52% of an oral or intravenous dose of moxifloxacin is metabolized via glucuronide and sulfate conjugation. The cytochrome P450 system is not involved in moxifloxacin metabolism, and is not affected by moxifloxacin. The sulfate conjugate (M1) accounts for approximately 38% of the dose, and is eliminated primarily in the feces. Approximately 14% of an oral or intravenous dose is converted to a glucuronide conjugate (M2), which is excreted exclusively in the urine. Peak plasma concentrations of M2 are approximately 40% those of the parent drug, while plasma concentrations of M1 are generally less than 10% those of moxifloxacin.In vitro studies with cytochrome (CYP) P450 enzymes indicate that moxifloxacin does not inhibit CYP3A4, CYP2D6, CYP2C9, CYP2C19, or CYP1A2, suggesting that moxifloxacin is unlikely to alter the pharmacokinetics of drugs metabolized by these enzymes.ExcretionApproximately 45% of an oral or intravenous dose of moxifloxacin is excreted as unchanged drug (~20% in urine and ~25% in feces). A total of 96% ± 4% of an oral dose is excreted as either unchanged drug or known metabolites. The mean (± SD) apparent total body clearance and renal clearance are 12 ± 2.0 L/hr and 2.6 ± 0.5 L/hr, respectively.Special PopulationsGeriatricFollowing oral administration of 400 mg moxifloxacin for 10 days in 16 elderly (8 male; 8 female) and 17 young (8 male; 9 female) healthy volunteers, there were no age-related changes in moxifloxacin pharmacokinetics. In 16 healthy male volunteers (8 young; 8 elderly) given a single 200 mg dose of oral moxifloxacin, the extent of systemic exposure (AUC and C max)was not statistically different between young and elderly males and elimination half-life was unchanged. No dosage adjustment is necessary based on age. In large phase III studies, the concentrations around the time of the end of the infusion in elderly patients following intravenous infusion of 400 mg were similar to those observed in young patients.PediatricThe pharmacokinetics of moxifloxacin in pediatric subjects have not been studied.GenderFollowing oral administration of 400 mg moxifloxacin daily for 10 days to 23 healthy males (19-75 years) and 24 healthy females (19-70 years), the mean AUC and C max were 8% and 16% higher, respectively, in females compared to males. There are no significant differences in moxifloxacin pharmacokinetics between male and female subjects when differences in body weight are taken into consideration.A 400 mg single dose study was conducted in 18 young males and females. The comparison of moxifloxacin pharmacokinetics in this study (9 young females and 9 young males) showed no differences in AUC or C max due to gender. Dosage adjustments based on gender are not necessary. RaceSteady-state moxifloxacin pharmacokinetics in male Japanese subjects were similar to those determined in Caucasians, with a mean C max of 4.1 µg/mL, an AUC24 of 47 µg•h/mL, and an elimination half-life of 14 hours, following 400 mg p.o. daily.Renal InsufficiencyThe pharmacokinetic parameters of moxifloxacin are not significantly altered in mild, moderate, severe, or end-stage renal disease. No dosage adjustment is necessary in patients with renal impairment, including those patients requiring hemodialysis (HD) or continuous ambulatory peritoneal dialysis (CAPD).In a single oral dose study of 24 patients with varying degrees of renal function from normal to severely impaired, the mean peak concentrations (C max) of moxifloxacin were reduced by 21% and 28% in the patients with moderate (CL CR ≥30 and ≤ 60 mL/min) and severe (CL CR < 30 mL/min) renal impairment, respectively. The mean systemic exposure (AUC) in these patients was increased by 13%. In the moderate and severe renally impaired patients, the mean AUC for the sulfate conjugate (M1) increased by 1.7-fold (ranging up to 2.8-fold) and mean AUC andC max for the glucuronide conjugate (M2) increased by 2.8-fold (ranging up to 4.8-fold) and1.4-fold (ranging up to2.5-fold), respectively.The pharmacokinetics of single dose and multiple dose moxifloxacin were studied in patients with CL CR < 20 mL/min on either hemodialysis or continuous ambulatory peritoneal dialysis (8 HD, 8 CAPD). Following a single 400 mg oral dose, the AUC of moxifloxacin in these HD and CAPD patients did not vary significantly from the AUC generally found in healthy volunteers. C max values of moxifloxacin were reduced by about 45% and 33% in HD and CAPD patients, respectively, compared to healthy, historical controls. The exposure (AUC) to the sulfate conjugate (M1) increased by 1.4- to 1.5-fold in these patients. The mean AUC of the glucuronide conjugate (M2) increased by a factor of 7.5, whereas the mean C max values of the glucuronide conjugate (M2) increased by a factor of 2.5 to 3, compared to healthy subjects. The sulfate and the glucuronide conjugates of moxifloxacin are not microbiologically active, and the clinical implication of increased exposure to these metabolites in patients with renal disease including those undergoing HD and CAPD has not been studied.Oral administration of 400 mg QD moxifloxacin for 7 days to patients on HD or CAPD produced mean systemic exposure (AUC ss) to moxifloxacin similar to that generally seen in healthy volunteers. Steady-state C max values were about 22% lower in HD patients but were comparable between CAPD patients and healthy volunteers. Both HD and CAPD removed only small amounts of moxifloxacin from the body (approximately 9% by HD, and 3% by CAPD). HD and CAPD also removed about 4% and 2% of the glucuronide metabolite (M2), respectively. Hepatic InsufficiencyIn 400 mg single oral dose studies in 6 patients with mild (Child Pugh Class A), and 10 patients with moderate (Child Pugh Class B), hepatic insufficiency, moxifloxacin mean systemic exposure (AUC) was 78% and 102%, respectively, of 18 healthy controls and mean peak concentration (C max)was 79% and 84% of controls.The mean AUC of the sulfate conjugate of moxifloxacin (M1) increased by 3.9-fold (ranging up to 5.9-fold) and 5.7-fold (ranging up to 8.0-fold) in the mild and moderate groups, respectively. The mean C max of M1 increased by approximately 3-fold in both groups (ranging up to 4.7- and 3.9-fold). The mean AUC of the glucuronide conjugate of moxifloxacin (M2) increased by 1.5-fold (ranging up to 2.5-fold) in both groups. The mean C max of M2 increased by 1.6- and 1.3-fold (ranging up to 2.7- and 2.1-fold), respectively. The clinical significance of increased exposure to the sulfate and glucuronide conjugates has not been studied. No dosage adjustment is recommended for mild or moderate hepatic insufficiency (Child Pugh Classes A and B). The pharmacokinetics of moxifloxacin in severe hepatic insufficiency (Child Pugh Class C) have not been studied. (See DOSAGE AND ADMINISTRATION.)Photosensitivity PotentialA study of the skin response to ultraviolet (UVA and UVB) and visible radiation conducted in 32 healthy volunteers (8 per group) demonstrated that moxifloxacin does not show phototoxicity in comparison to placebo. The minimum erythematous dose (MED) was measured before and after treatment with moxifloxacin (200 mg or 400 mg once daily), lomefloxacin (400 mg once daily), or placebo. In this study, the MED measured for both doses of moxifloxacin were not significantly different from placebo, while lomefloxacin significantly lowered the MED. (See PRECAUTIONS, Information for Patients.)It is difficult to ascribe relative photosensitivity/phototoxicity among various fluoroquinolones during actual patient use because other factors play a role in determining a subject’s susceptibility to this adverse event such as: a patient’s skin pigmentation, frequency and duration of sun and artificial ultraviolet light (UV) exposure, wearing of sunscreen andprotective clothing, the use of other concomitant drugs and the dosage and duration of fluoroquinolone therapy (See ADVERSE REACTIONS and ADVERSEREACTIONS/Post-Marketing Adverse Event Reports).Drug-drug InteractionsThe potential for pharmacokinetic drug interactions between moxifloxacin and itraconazole, theophylline, warfarin, digoxin, atenolol, probenecid, morphine, oral contraceptives, ranitidine, glyburide, calcium, iron, and antacids has been evaluated. There was no clinically significant effect of moxifloxacin on itraconazole, theophylline, warfarin, digoxin, atenolol, oral contraceptives, or glyburide kinetics. Itraconazole, theophylline, warfarin, digoxin, probenecid, morphine, ranitidine, and calcium did not significantly affect the pharmacokinetics of moxifloxacin. These results and the data from in vitro studies suggest that moxifloxacin is unlikely to significantly alter the metabolic clearance of drugs metabolized by CYP3A4, CYP2D6, CYP2C9, CYP2C19, or CYP1A2 enzymes.As with all other quinolones, iron and antacids significantly reduced bioavailability of moxifloxacin.Itraconazole:In a study involving 11 healthy volunteers, there was no significant effect of itraconazole (200 mg once daily for 9 days), a potent inhibitor of cytochrome P4503A4, on the pharmacokinetics of moxifloxacin (a single 400 mg dose given on the 7th day of itraconazole dosing). In addition, moxifloxacin was shown not to affect the pharmacokinetics of itraconazole. Theophylline:No significant effect of moxifloxacin (200 mg every twelve hours for 3 days) on the pharmacokinetics of theophylline (400 mg every twelve hours for 3 days) was detected in a study involving 12 healthy volunteers. In addition, theophylline was not shown to affect the pharmacokinetics of moxifloxacin. The effect of co-administration of a 400 mg dose of moxifloxacin with theophylline has not been studied, but it is not expected to be clinically significant based on in vitro metabolic data showing that moxifloxacin does not inhibit the CYP1A2 isoenzyme.Warfarin:No significant effect of moxifloxacin (400 mg once daily for eight days) on the pharmacokinetics of R- and S-warfarin (25 mg single dose of warfarin sodium on the fifth day) was detected in a study involving 24 healthy volunteers. No significant change in prothrombin time was observed. (See PRECAUTIONS, Drug Interactions.)Digoxin:No significant effect of moxifloxacin (400 mg once daily for two days) on digoxin (0.6 mg as a single dose) AUC was detected in a study involving 12 healthy volunteers. The mean digoxin C max increased by about 50% during the distribution phase of digoxin. This transient increase in digoxin C max is not viewed to be clinically significant. Moxifloxacin pharmacokinetics were similar in the presence or absence of digoxin. No dosage adjustment for moxifloxacin or digoxin is required when these drugs are administered concomitantly. Atenolol:In a crossover study involving 24 healthy volunteers (12 male; 12 female), the mean atenolol AUC following a single oral dose of 50 mg atenolol with placebo was similar to that observed when atenolol was given concomitantly with a single 400 mg oral dose of moxifloxacin. The mean C max of single dose atenolol decreased by about 10% following co-administration with a single dose of moxifloxacin.Morphine:No significant effect of morphine sulfate (a single 10 mg intramuscular dose) on the mean AUC and C max of moxifloxacin (400 mg single dose) was observed in a study of 20 healthy male and female volunteers.Oral Contraceptives:A placebo-controlled study in 29 healthy female subjects showed that moxifloxacin 400 mg daily for 7 days did not interfere with the hormonal suppression of oral contraception with 0.15 mg levonorgestrel/0.03 mg ethinylestradiol (as measured by serum progesterone, FSH, estradiol, and LH), or with the pharmacokinetics of the administered contraceptive agents.Probenecid:Probenecid (500 mg twice daily for two days) did not alter the renal clearance and total amount of moxifloxacin (400 mg single dose) excreted renally in a study of 12 healthy volunteers.Ranitidine:No significant effect of ranitidine (150 mg twice daily for three days as pretreatment) on the pharmacokinetics of moxifloxacin (400 mg single dose) was detected in a study involving 10 healthy volunteers.Antidiabetic agents:In diabetics, glyburide (2.5 mg once daily for two weeks pretreatment and for five days concurrently) mean AUC and C max were 12% and 21% lower, respectively, when taken with moxifloxacin (400 mg once daily for five days) in comparison to placebo. Nonetheless, blood glucose levels were decreased slightly in patients taking glyburide and moxifloxacin in comparison to those taking glyburide alone, suggesting no interference by moxifloxacin on the activity of glyburide. These interaction results are not viewed as clinically significant. Calcium:Twelve healthy volunteers were administered concomitant moxifloxacin (single 400 mg dose) and calcium (single dose of 500 mg Ca++ dietary supplement) followed by an additional two doses of calcium 12 and 24 hours after moxifloxacin administration. Calcium had no significant effect on the mean AUC of moxifloxacin. The mean C max was slightly reduced and the time to maximum plasma concentration was prolonged when moxifloxacin was given with calcium compared to when moxifloxacin was given alone (2.5 hours versus 0.9 hours). These differences are not considered to be clinically significant.Antacids:When moxifloxacin (single 400 mg tablet dose) was administered two hours before, concomitantly, or 4 hours after an aluminum/magnesium-containing antacid (900 mg aluminum hydroxide and 600 mg magnesium hydroxide as a single oral dose) to 12 healthy volunteers there was a 26%, 60% and 23% reduction in the mean AUC of moxifloxacin, respectively. Moxifloxacin should be taken at least 4 hours before or 8 hours after antacids containing magnesium or aluminum, as well as sucralfate, metal cations such as iron, and multivitamin preparations with zinc, or VIDEX® (didanosine) chewable/ buffered tablets or the pediatric powder for oral solution. (See PRECAUTIONS, Drug Interactions and DOSAGE AND ADMINISTRATION.) Iron:When moxifloxacin tablets were administered concomitantly with iron (ferrous sulfate 100 mg once daily for two days), the mean AUC and C max of moxifloxacin was reduced by 39% and 59%, respectively. Moxifloxacin should only be taken more than 4 hours before or 8 hours after iron products. (See PRECAUTIONS, Drug Interactions and DOSAGE AND ADMINISTRATION.) Electrocardiogram:Prolongation of the QT interval in the ECG has been observed in some patients receiving moxifloxacin. Following oral dosing with 400 mg of moxifloxacin the mean (± SD) change in QTc from the pre-dose value at the time of maximum drug concentration was 6 msec (± 26) (n = 787). Following a course of daily intravenous dosing (400 mg; 1 hour infusion each day) the mean change in QTc from the Day 1 pre-dose value was 9 msec (± 24) on Day 1 (n = 69) and 3 msec (± 29) on Day 3 (n = 290). (See WARNINGS.)There is limited information available on the potential for a pharmacodynamic interaction in humans between moxifloxacin and other drugs that prolong the QTc interval of the electrocardiogram. Sotalol, a Class III antiarrhythmic, has been shown to further increase the QTc interval when combined with high doses of intravenous (I.V.) moxifloxacin in dogs. Therefore, moxifloxacin should be avoided with Class IA and Class III antiarrhythmics. (See ANIMAL PHARMACOLOGY, WARNINGS,and PRECAUTIONS.)MICROBIOLOGYMoxifloxacin has in vitro activity against a wide range of Gram-positive and Gram-negative microorganisms. The bactericidal action of moxifloxacin results from inhibition of the topoisomerase II (DNA gyrase) and topoisomerase IV required for bacterial DNA replication, transcription, repair, and recombination. It appears that the C8-methoxy moiety contributes to enhanced activity and lower selection of resistant mutants of Gram-positive bacteria compared to the C8-H moiety. The presence of the bulky bicycloamine substituent at the C-7 position prevents active efflux, associated with the NorA or pmrA genes seen in certain Gram-positive bacteria. The mechanism of action for quinolones, including moxifloxacin, is different from that of macrolides, beta-lactams, aminoglycosides, or tetracyclines; therefore, microorganisms resistant to these classes of drugs may be susceptible to moxifloxacin and other quinolones. There is no known cross-resistance between moxifloxacin and other classes of antimicrobials.In vitro resistance to moxifloxacin develops slowly via multiple-step mutations. Resistance to moxifloxacin occurs in vitro at a general frequency of between 1.8 x 10–9 to < 1 x 10–11 for Gram-positive bacteria.Cross-resistance has been observed between moxifloxacin and other fluoroquinolones against Gram-negative bacteria. Gram-positive bacteria resistant to other fluoroquinolones may, however, still be susceptible to moxifloxacin.Moxifloxacin has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section. Aerobic Gram-positive microorganismsEnterococcus faecalis (many strains are only moderately susceptible)Staphylococcus aureus (methicillin-susceptible strains only)Streptococcus anginosusStreptococcus constellatusStreptococcus pneumoniae (including multi-drug resistant strains [MDRSP]*) Streptococcus pyogenes* MDRSP, Multi-drug resistant Streptococcus pneumoniae includes isolates previously known as PRSP (Penicillin-resistant S. pneumoniae), and are strains resistant to two or more of the following antibiotics: penicillin (MIC ≥ 2 μg/mL), 2nd generation cephalosporins (e.g., cefuroxime), macrolides, tetracyclines, and trimethoprim/sulfamethoxazole.Aerobic Gram-negative microorganismsEnterobacter cloacaeEscherichia coliHaemophilus influenzaeHaemophilus parainfluenzaeKlebsiella pneumoniaeMoraxella catarrhalisProteus mirabilisAnaerobic microorganismsBacteroides fragilisBacteroides thetaiotaomicronClostridium perfringensPeptostreptococcus speciesOther microorganismsChlamydia pneumoniaeMycoplasma pneumoniaeThe following in vitro data are available, but their clinical significance is unknown.Moxifloxacin exhibits in vitro minimum inhibitory concentrations (MICs) of 2 µg/mL or lessagainst most (≥ 90%) strains of the following microorganisms; however, the safety andeffectiveness of moxifloxacin in treating clinical infections due to these microorganisms have notbeen established in adequate and well-controlled clinical trials.Aerobic Gram-positive microorganismsStaphylococcus epidermidis (methicillin-susceptible strains only)Streptococcus agalactiaeStreptococcus viridans groupAerobic Gram-negative microorganismsCitrobacter freundiiKlebsiella oxytocaLegionella pneumophilaAnaerobic microorganismsFusobacterium speciesPrevotella speciesSusceptibility TestsDilution Techniques:Quantitative methods are used to determine antimicrobial minimuminhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteriato antimicrobial compounds. The MICs should be determined using a standardized procedure.Standardized procedures are based on a dilution method1 (broth or agar) or equivalent withstandardized inoculum concentrations and standardized concentrations of moxifloxacin powder.The MIC values should be interpreted according to the following criteria:For testing Enterobacteriaceae and methicillin-susceptible Staphylococcus aureus:MIC (µg/mL)Interpretation≤2.0 Susceptible(S)4.0Intermediate(I)≥8.0Resistant(R)For testing Haemophilus influenzae and Haemophilus parainfluenzae a:MIC (µg/mL) Interpretation(S) ≤1.0 Susceptiblea This interpretive standard is applicable only to broth microdilution susceptibility tests withHaemophilus influenzae and Haemophilus parainfluenzae using Haemophilus Test Medium1.The current absence of data on resistant strains precludes defining any results other than“Susceptible”. Strains yielding MIC results suggestive of a “nonsusceptible” category should besubmitted to a reference laboratory for further testing.For testing Streptococcus species including Streptococcus pneumoniae b and Enterococcus faecalis:MIC (µg/mL)Interpretation≤1.0 Susceptible(S)2.0Intermediate(I)≥ 4.0Resistant(R)b These interpretive standards are applicable only to broth microdilution susceptibility tests using cation-adjusted Mueller-Hinton broth with 2 - 5% lysed horse blood.A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of “Intermediate” indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard moxifloxacin powder should provide the following MIC values:Microorganism MIC (µg/mL)Enterococcus faecalis ATCC 292120.06- 0.5Escherichia coli ATCC 259220.008- 0.06Haemophilus influenzae ATCC 49247c0.008- 0.03Staphylococcus aureus ATCC 292130.015- 0.06Streptococcus pneumoniae ATCC 49619d0.06- 0.25c This quality control range is applicable to only H. influenzae ATCC 49247 tested by a broth microdilution procedure using Haemophilus Test Medium (HTM)1.d This quality control range is applicable to only S. pneumoniae ATCC 49619 tested by a broth microdilution procedure using cation-adjusted Mueller-Hinton broth with 2 - 5% lysed horse blood.Diffusion Techniques:Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure2 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 5-µg moxifloxacin to test the susceptibility of microorganisms to moxifloxacin.Reports from the laboratory providing results of the standard single-disk susceptibility test with a 5-µg moxifloxacin disk should be interpreted according to the following criteria:。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
盐酸莫西沙星氯化钠的用法用量及注意事项
盐酸莫西沙星氯化钠是我们在日常家庭用药中可以看见的药品,有的家庭如果有家人患有鼻窦炎,可能就会吃这个药,因为它主要就是治疗呼吸道感染的,主要的作用就是消除呼吸道里面的炎症,改善我们的呼吸道。
对这个药品不了解的人可以仔细阅读该药品的用法用量,以及在使用中需要注意到的事项。
一、用法用量给药方法:根据中国健康受试者心脏所能耐受的输液速率以及国内I、II、III期临床研究的结果,推荐本品的输液时间应为90分钟。
(国外推荐0.4g莫西沙星静脉给药的输液时间应大于60分钟。
)
剂量范围(成人):推荐剂量为一次0.4g,一日一次(一次1瓶,一日一次)。
根据症状的严重程度或临床反应决定疗程。
治疗上呼吸道和下呼吸道感染时通常可按照下列疗程:
1.慢性支气管炎急性发作:5天
2.社区获得性肺炎:序贯给药(静脉给药后继续口服用药)推荐的总疗程为7~14天。
3.急性窦炎:7天
4.治疗皮肤和软组织感染的推荐疗程为7天。
二、注意事项:
1.妊娠和哺乳期妇女。
2.由于缺乏患有肝功能严重损伤(Child Pugh C级)的患者和转氨酶升高大于5倍正常值上限的患者使用莫西沙星的临床数据,该药在这类患者中禁止使用。
3.18岁以下患者。
看了上面对盐酸莫西沙星氯化钠的介绍,我们一定知道18岁以下的未成年不能使用该产品。
虽然有时候我们对于一个药的用处很了解,经常会自己去药店买取需要的药品,但是我们也要
注意几点内容,经常去药店买药的朋友要仔细观看药盒上面的注意事项,以及它的用法用量。
