英语 病例 模板
英文病例写作范文阅读带翻译
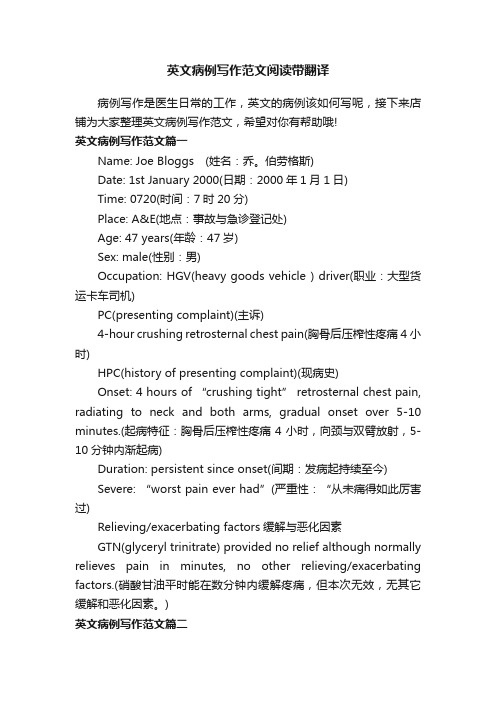
英文病例写作范文阅读带翻译病例写作是医生日常的工作,英文的病例该如何写呢,接下来店铺为大家整理英文病例写作范文,希望对你有帮助哦!英文病例写作范文篇一Name: Joe Bloggs (姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Onset: 4 hours of “crushing tight” retrosternal chest pain, radiating to neck and both arms, gradual onset over 5-10 minutes.(起病特征:胸骨后压榨性疼痛4小时,向颈与双臂放射,5-10分钟内渐起病)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
英文病历报告作文模板
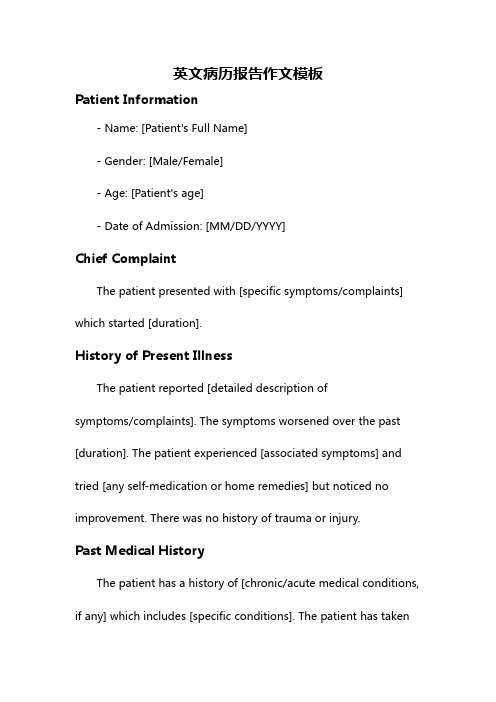
英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。
英文完全病历模板-详细版
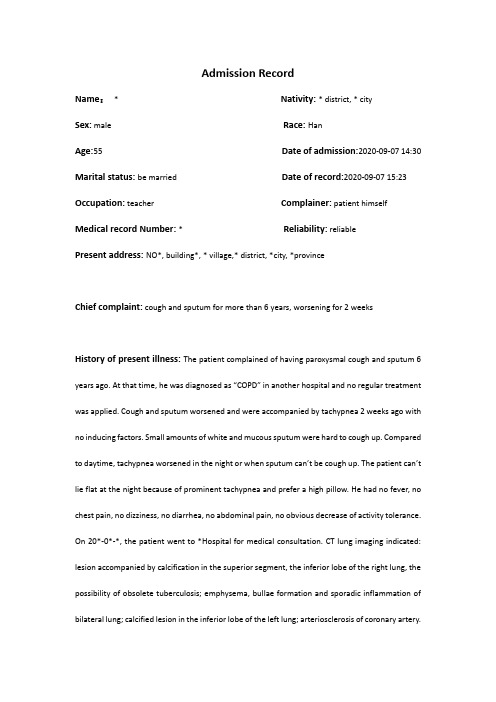
Admission RecordName:* Nativity: * district, * citySex:male Race: HanAge:55 Date of admission:2020-09-07 14:30 Marital status: be married Date of record:2020-09-07 15:23 Occupation:teacher Complainer:patient himself Medical record Number: * Reliability: reliablePresent address: NO*, building*, * village,* district, *city, *provinceChief complaint: cough and sputum for more than 6 years, worsening for 2 weeksHistory of present illness: The patient complained of having paroxysmal cough and sputum 6 years ago. At that time, he was diagnosed as “COPD” in another hospital and no regular treatment was applied. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago with no inducing factors. Small amounts of white and mucous sputum were hard to cough up. Compared to daytime, tachypnea worsened in the night or when sputum can’t be cough up. The patient can’t lie flat at the night because of prominent tachypnea and prefer a high pillow. He had no fever, no chest pain, no dizziness, no diarrhea, no abdominal pain, no obvious decrease of activity tolerance. On 20*-0*-*, the patient went to *Hospital for medical consultation. CT lung imaging indicated: lesion accompanied by calcification in the superior segment, the inferior lobe of the right lung, the possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in the inferior lobe of the left lung; arteriosclerosis of coronary artery.Pulmonary function tests indicated:d obstructive ventilation dysfunction; bronchial dilation test was negative2.moderate decrease of diffusion function, lung volume, residual volume and the ratio of lungvolume; residual volume were normalThe patient was diagnosed as “AECOPD” and prescribed cefoxitin to anti-infection for a week, Budesonide and Formoterol to relieve bronchial muscular spasm and asthma,amb roxol to dilute sputum, and traditional Chinese medicine (specific doses were unknown).The patient was discharged from the hospital after symptoms of cough and sputum slightly relieved with a prescription of using Moxifloxacin outside the hospital for 1 week. Cough and sputum were still existing, thus the patient came to our hospital for further treatment and the outpatient department admitted him in the hospital with “COPD”. His mental status, appetite, sleep, voiding, and stool were normal. No obvious decrease or increase of weight.Past history: The patient was diagnosed as type 2 diabetes 1 years ago and take Saxagliptin (5mg po qd) without regularly monitoring the levels of blood sugar. The patient denies hepatitis, tuberculosis, malaria, hypertension, mental illness, and cardiovascular diseases. Denies surgical procedures, trauma, transfusion, food allergy and drug allergy. The history of preventive inoculation is not quite clear.Personal history: The patient was born in *district, * city and have lived in * since birth. He denies water contact in the schistosome epidemic area. Smoking 10 cigarettes a day for 20 years and have stopped for half a month. Denies excessive drinking and contact with toxics.Marital history: Married at age of 27 and have two daughters. Both the mate and daughters are healthy.Family history: Denies familial hereditary diseases.Physical ExaminationT: 36.5℃ P:77bpm R: 21 breaths/min BP:148/85mmHgGeneral condition:normally developed, well-nourished, normal facies, alert, active position, cooperation is goodSkin and mucosa: no jaundiceSuperficial lymph nodes: no enlargementHead organs: normal shape of headEyes:no edema of eyelids; no exophthalmos; eyeballs move freely; no bleeding spots of conjunctiva; no sclera jaundice; cornea clear; pupils round, symmetrical in size and acutely reactive to light.Ears: no deformity of auricle; no purulent secretion of the external canals; no tenderness over mastoidsNose: normal shape; good ventilation;no nasal ale flap; no tenderness over nasal sinus; Mouth: no cyanosis of lips; no bleeding spots of mouth mucosa; no tremor of tongue; glossy tongue in midline; no pharynx hyperemia; no enlarged tonsils seen and no suppurative excretions; Neck: supple without rigidity, symmetrical; no cervical venous distension; Hepatojugular reflux is negative; no vascular murmur; trachea in midline; no enlargement of thyroid glandChest: symmetrical; no deformity of thoraxLung:Inspection:equal breathing movement on two sidesPalpation: no difference of vocal fremitus over two sides;Percussion: resonance over both lungs;Auscultation: decreased breath sounds over both lungs; no dry or moist rales audible; no pleural friction rubsHeart:Inspection: no pericardial protuberance; Apex beat seen 0.5cm within left mid-clavicular at fifth intercostal space;Palpation: no thrill felt;Percussion: normal dullness of heart bordersAuscultation: heart rate 78bpm; rhythm regular; normal intensity of heart sounds; no murmurs or pericardial friction sound audiblePeripheral vascular sign: no water-hammer pulse; no pistol shot sound; no Duroziez’s murmur; no capillary pulsation sign; no visible pulsation of carotid arteryAbdomen:Inspection: no dilated veins; no abnormal intestinal and peristaltic waves seenPalpation: no tenderness or rebounding tenderness; abdominal wall flat and soft; liver and spleen not palpable; Murphy's sign is negativePercussion: no shifting dullness; no percussion tenderness over the liver and kidney regionAuscultation: normal bowel sounds.External genitalia: uncheckedSpine: normal spinal curvature without deformities; normal movementsExtremities: no clubbed fingers(toes); no redness and swelling of joints; no edema over both legs; no pigmentation of skins of legsNeurological system: normal muscle tone and myodynamia; normal abdominal and bicipital muscular reflex; normal patellar and heel-tap reflex; Babinski sign(-);Kerning sign(-) ; Brudzinski sign(-)Laboratory DataKey Laboratory results including CT imaging and pulmonary function test have been detailed in the part of history of present illness.Abstract*, male, 55 years old. Admitted to our hospital with the chief complaint of cough and sputum for more than 6 years, worsening for 2 weeks. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago. The patient can’t lie flat in the night because of prominent tachypnea and prefer a high pillow.Physical Examination: T: 36.5℃,P: 77bpm, R: 21 breaths per minute, BP:148/85mmHg. Decreased breath sounds over both lungs; no dry or moist rales audible.Laboratory data: CT lung imaging indicates: lesion accompanied by calcification in superior segment, inferior lobe of right lung, possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in inferior lobe of left lung. Pulmonary function tests indicate: mild obstructive ventilation dysfunction, bronchial dilation test was negative moderate decrease of diffusion function.Primary Diagnosis:1.AECOPD2.Type 2 Diabetes3.Primary Hypertension Doctor’s Signature:。
英文病例模版
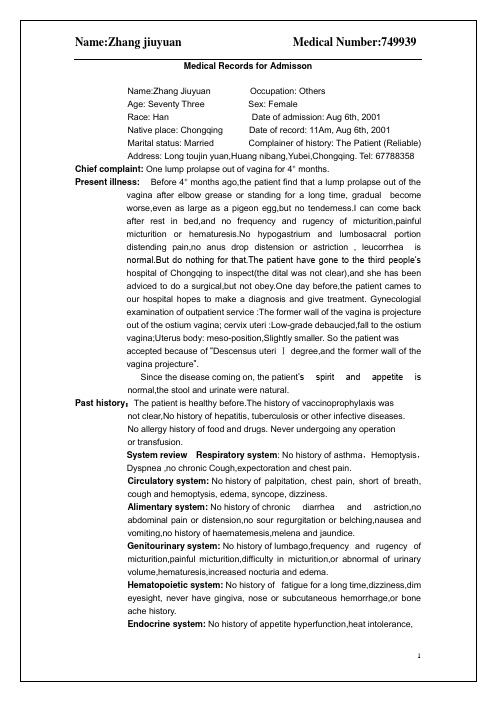
discharges were found invetibulum nasi. Septum nasi was in midline. No
nares flaring. No tenderness in nasal sinuses.
Superficial lymph nodes:Superficial lymph nodes were not found enlarged.
Head:Cranium:Hair was black and white, well distributed.No deformities. No scars.No pain when we press on. No masses.No tenderness.
Kinetic system:No history of joint pain, numbness,red and swollen,
metallaxis,myalgia or myophagism.
Neural system:No history of long-term headache,dizziness and vertigo,
atage 46.
Marital history:She’s marriedat 28,her husband is heslth,and the relationship
between them were concord.
Childbearing history:G4P2,induced abortion twice,natural labourtwice,and they are heathy.
英文病例模版
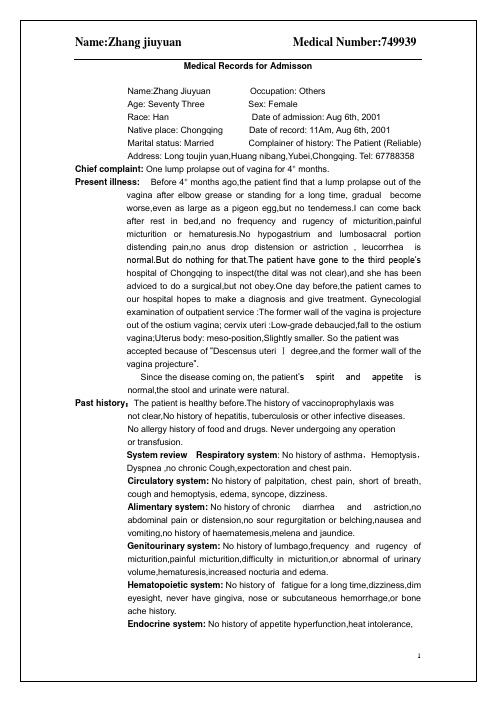
Present illness:Before 4+months ago,the patient find that a lump prolapse out of the vagina afterelbow grease or standing for a long time,gradualbecome worse,even as large as a pigeon egg,but no tenderness.I can come back after rest in bed,and no frequency and rugency of micturition,painful micturition or hematuresis.No hypogastrium and lumbosacral portion distending pain,no anus drop distension or astriction , leucorrhea is normal.But do nothing for that.The patient have gone to the third people’s hospital of Chongqing to inspect(the dital was not clear),and she has been adviced to do a surgical,but not obey.One day before,the patient cames to our hospital hopes to make a diagnosis and give treatment. Gynecologial examination of outpatient service :The former wall of the vagina is projecture out of the ostium vagina; cervix uteri :Low-grade debaucjed,fall to the ostium vagina;Uterus body: meso-position,Slightly smaller. So the patient was
英语病历模板范文

英语病历模板范文Patient Identification:Date of Birth: [DOB]Sex: [Male/Female]Patient ID: [Unique Identifier]Chief Complaint:[Patient's primary concern or reason for the visit, e.g., "Severe headache for the past 3 days"]History of Present Illness:[Detailed account of the onset, duration, severity, and any associated symptoms of the current illness. Include any treatments already attempted.]Past Medical History:[List any previous medical conditions, surgeries, or hospitalizations.]Medications:[List all current medications, including dosages andfrequency.]Allergies:[Note any known allergies to medications, foods, or environmental factors.]Family Medical History:[Provide information on any significant medicalconditions in the patient's family.]Social History:[Include relevant lifestyle factors such as smoking status, alcohol consumption, exercise habits, and occupation.]Review of Systems:[Briefly summarize the patient's current state inrelation to various body systems, e.g., "No chest pain, no shortness of breath."]Physical Examination:[Record findings from the physical examination, including vital signs, general appearance, and specific observations related to the chief complaint.]Assessment:[Summarize the likely diagnosis or condition based on the information gathered.]Plan:[Outline the proposed treatment plan, including medications, referrals, follow-up appointments, and any necessary tests or procedures.]。
英文病例范文
英文病例范文Title: A Case Study of Patient with Hypertension and Type 2 DiabetesPatient History:The patient is a 55-year-old male who presents with a history of hypertension and type 2 diabetes. The patient reports a 10-year history of hypertension and a recent diagnosis of type 2 diabetes. He reports that he has been experiencing increased fatigue, frequent urination, andblurred vision over the past few months.Physical Exam:Upon physical examination, the patient's blood pressureis 150/90 mmHg, and his heart rate is 80 beats per minute.His BMI is 30 kg/m2, and his waist circumference is 40 inches. The patient's respiratory rate is 16 breaths per minute, and his oxygen saturation is 98% on room air. The patient's bloodglucose level is 200 mg/dL, and his HbA1c is 8.5%. His lipid panel shows elevated LDL cholesterol and decreased HDL cholesterol.Diagnosis:Based on the patient's history and physical exam, he is diagnosed with uncontrolled hypertension and uncontrolled type 2 diabetes. The patient's elevated blood pressure and high blood glucose levels indicate poorly controlled conditions. In addition, the patient's lipid panel results suggest dyslipidemia.Treatment Plan:The treatment plan for this patient consists of lifestyle modifications and pharmacotherapy. The patient is advised to adopt a healthy diet, engage in regular physical activity, and quit smoking. The patient is also prescribed antihypertensive medication to manage his elevated bloodpressure and antidiabetic medication to control his high blood glucose levels.Follow-up:The patient is scheduled for regular follow-up visits to monitor his blood pressure, blood glucose levels, and lipid profile. The patient's progress will be closely monitored to assess the effectiveness of the treatment plan and to make any necessary adjustments. The patient will also receive ongoing education and counseling on the importance of adherence to his treatment plan and the management of his chronic conditions.Conclusion:In conclusion, the case study of this patient with hypertension and type 2 diabetes highlights the importance of early detection, proper diagnosis, and comprehensive management of these chronic conditions. Through a combination of lifestyle modifications and pharmacotherapy, the patientwill aim to achieve better control of his blood pressure, blood glucose levels, and lipid profile, ultimately reducing the risk of complications and improving his overall health and well-being.。
医学英语病历书写范文
医学英语病历书写范文Here's a sample of a medical English patient chart entry, written in an informal yet professional manner, adhering to the given requirements:The patient presented with complaints of persistent headache and occasional dizziness. He mentioned that the pain was localized to the left side of his forehead and tended to worsen with stress.On physical examination, I noticed a slight elevation in blood pressure, but other vital signs were within normal limits. The patient's neurological reflexes were intact.The patient mentioned a history of high blood pressure and was on regular medication for the same. However, he admitted to missing a few doses recently.We discussed possible causes of his headache, including stress, lack of sleep, and diet. I recommended lifestylemodifications and a follow-up visit if symptoms persisted.The patient expressed concern about the possibility of a more serious underlying condition. I assured him that while we need to be vigilant, his current symptoms are more likely to be related to lifestyle factors.I prescribed a mild pain reliever and advised him to monitor his blood pressure regularly. The patient seemed relieved after the consultation and thanked me for my time.Overall, the patient's condition seems manageable with lifestyle changes and regular monitoring. I'll recommend further testing if symptoms worsen or persist.。
临床案例模板英语作文
临床案例模板英语作文英文回答:Clinical Case Template。
Demographic Information:Name: John Doe。
Age: 55。
Gender: Male。
Occupation: Software Engineer。
Chief Complaint:Intermittent chest pain for the past 2 weeks。
History of Present Illness:The patient is a 55-year-old male who presents with a 2-week history of intermittent chest pain. The pain is described as a squeezing sensation that radiates to theleft arm. It occurs with exertion and is relieved by rest. The patient also reports shortness of breath and fatigue.The patient has no history of coronary artery disease, but he does have a history of hypertension and hyperlipidemia. He is a current smoker and drinks alcohol socially.Past Medical History:Hypertension。
Hyperlipidemia。
Social History:Current smoker。
Drinks alcohol socially。
Family History:Father died of myocardial infarction at age 60。
四年级英语病历范文
四年级英语病历范文Patient Name: Zhang SanAge: 10 years oldDate of Visit: October 10th, 2023Chief Complaint:The patient complains of a sore throat, cough, and runny nose for the past three days.History of Present Illness:The patient's symptoms started three days ago with a sore throat, followed by a cough and runny nose. The cough is dry and persistent, and the patient has been experiencing some difficulty swallowing due to the sore throat. There is no history of fever, chills, or ear pain. The patient's appetite has decreased, and there is a mild decrease in energy levels.Past Medical History:The patient has a history of seasonal allergies, with symptoms of sneezing and itchy eyes during the spring andfall seasons. There is no history of asthma or other chronic respiratory conditions.Family History:There is no significant family history of respiratory illnesses or other chronic conditions.Medications:The patient is not currently taking any medications.Allergies:The patient has no known drug allergies.Review of Systems:- Constitutional: Decreased appetite and energy levels - Respiratory: Sore throat, cough, runny nose- Gastrointestinal: No nausea, vomiting, or diarrhea - Musculoskeletal: No joint pain or swellingPhysical Examination:- Vital Signs: Temperature 98.6°F, pulse 80 beats per minute, respiratory rate 20 breaths per minute, blood pressure 110/70 mmHg- General: The patient appears fatigued, but alert and oriented- Head and Neck: Erythematous pharynx, no tonsillar exudates, clear nasal discharge- Respiratory: Lungs clear to auscultation bilaterally - Cardiovascular: Regular rate and rhythm, no murmurs or gallops- Abdomen: Soft, non-tender, non-distendedAssessment:Based on the patient's history and physical examination, the likely diagnosis is an upper respiratory tract infection, possibly viral in nature.Plan:1. Symptomatic treatment for sore throat and cough, including acetaminophen for pain and discomfort2. Encourage increased fluid intake and rest3. Monitor for any signs of worsening symptoms, such as persistent high fever or difficulty breathing4. Follow up in three days if symptoms do not improve or worsen中文回答:患者张三,10岁,主诉三天来咽喉痛、咳嗽和流鼻涕。
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
CASEMedical Number: 682786 General informationName:Wang Runzhen Age: Forty threeSex: FemaleRace:Han Occupation: Teacher Nationality:China Marital status: Married Address: NO.38, Hangkong Road, Jiefang Rvenue, Hankou, Hubei. Tel: 82422500Date of admission:Jan 11st, 2001Date of record: 11Am, Jan 11st, 2001 Complainer of history: the patient herself Reliability: ReliableChief complaint: Right breast mass found for more than half a month.Present illness: Half a month ago, the patient suddenly felt pain in her right chest when she put up her hand. After touching it, she found a mass in her right breast, but no tendness, and the patient didn’t pay attention it. Then the pain became more and more serious, so the patient went to tumour hospital and received a pathology centesis. Her diagnosis was breast cancer. Then she came to our hospital and asked for an operation.Since onset, her appetite was good, and both her spiritedness and physical energy are normal. Defecation and urination are normal, too.Past historyOperative history: Never undergoing any operation. Infectious history:No history of severe infectious disease.Allergic history: She was not allergic to penicillin or sulfamide.Respiratory system: No history of respiratory disease. Circulatory system: No history of precordial pain. Alimentary system: No history of regurgitation. Genitourinary system:No history of genitourinary disease.Hematopoietic system:No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural system: No history of headache or dizziness. Personal historyShe was born in Wuhan on Nov 19th, 1957 and almost always lived in Wuhan. She graduated from senior high school. Her living conditions were good. No bad personal habits and customs.Menstrual history:The first time when she was 14. Lasting 3 to 4 days every times and its cycle is about 30 days.Obstetrical history:Pregnacy 3 times, once nature production, abortion twice.Contraceptive history: Not clear.Family history: His parents have both died.Physical examinationT 36.4℃,P 80/min, R 20/min, BP 90/60mmHg. She is well developed and moderately nourished. Active position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were notenlarged.HeadCranium:Hair was black and well distributed. No deformities. No scars. No masses. No tenderness.Ear:Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose:No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye: Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall:Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast:Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs:Respiratory movement was bilaterally symmetric with the frequency of 20/min. Thoracic expansion and tactile fremitus were symmetric bilaterally.No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart:No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 80/min. Cardiac rhythm was regular. No pathological murmurs.Abdomen:Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. There was not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus 5/min. No vascular murmurs. Extremities: No articular swelling. Free movements of all limbs.Neural system:Physiological reflexes were existent without any pathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationNo.Professional Examination There are a about 3*3*2 cm mass in outer-up field of her right breast. It is hard but no tendness. It can be moved and its surface is smooth. The skin of her breast is normal. Corresponding superficial lymph nodes don’t enlarge.History summary1.Patient was a teacher, female, 43 years old.2.Right breast mass found for more than half a month.3.No special past history.4.Physical examination showed no abnormity in lung, heart and abdoman. Information about her breast can be seen above.5. Shorting of investigation information.Impression: Breast cancer (right)Signature: He Lin(95-10033)。
