英文病历模版
新生儿科英文病历
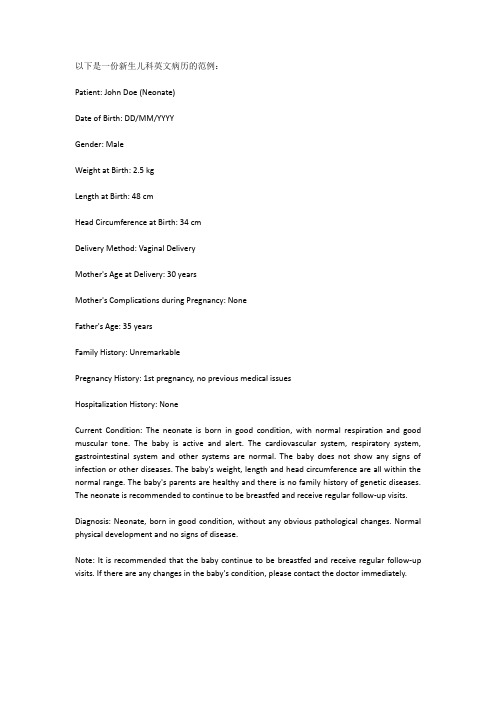
以下是一份新生儿科英文病历的范例:Patient: John Doe (Neonate)Date of Birth: DD/MM/YYYYGender: MaleWeight at Birth: 2.5 kgLength at Birth: 48 cmHead Circumference at Birth: 34 cmDelivery Method: Vaginal DeliveryMother's Age at Delivery: 30 yearsMother's Complications during Pregnancy: NoneFather's Age: 35 yearsFamily History: UnremarkablePregnancy History: 1st pregnancy, no previous medical issuesHospitalization History: NoneCurrent Condition: The neonate is born in good condition, with normal respiration and good muscular tone. The baby is active and alert. The cardiovascular system, respiratory system, gastrointestinal system and other systems are normal. The baby does not show any signs of infection or other diseases. The baby's weight, length and head circumference are all within the normal range. The baby's parents are healthy and there is no family history of genetic diseases. The neonate is recommended to continue to be breastfed and receive regular follow-up visits.Diagnosis: Neonate, born in good condition, without any obvious pathological changes. Normal physical development and no signs of disease.Note: It is recommended that the baby continue to be breastfed and receive regular follow-up visits. If there are any changes in the baby's condition, please contact the doctor immediately.。
soap英文病历
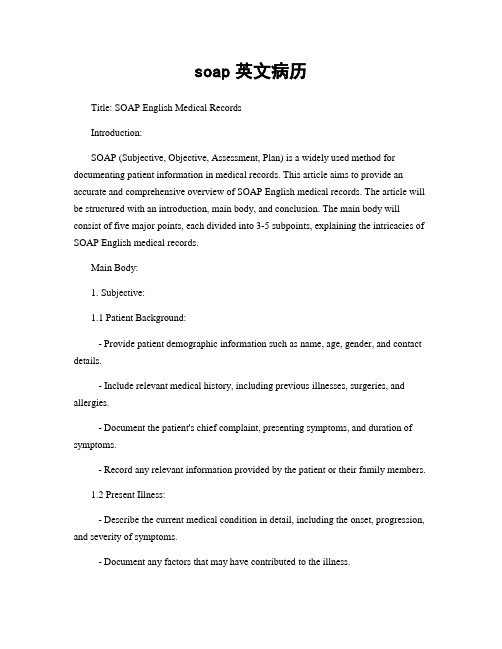
soap英文病历Title: SOAP English Medical RecordsIntroduction:SOAP (Subjective, Objective, Assessment, Plan) is a widely used method for documenting patient information in medical records. This article aims to provide an accurate and comprehensive overview of SOAP English medical records. The article will be structured with an introduction, main body, and conclusion. The main body will consist of five major points, each divided into 3-5 subpoints, explaining the intricacies of SOAP English medical records.Main Body:1. Subjective:1.1 Patient Background:- Provide patient demographic information such as name, age, gender, and contact details.- Include relevant medical history, including previous illnesses, surgeries, and allergies.- Document the patient's chief complaint, presenting symptoms, and duration of symptoms.- Record any relevant information provided by the patient or their family members.1.2 Present Illness:- Describe the current medical condition in detail, including the onset, progression, and severity of symptoms.- Document any factors that may have contributed to the illness.- Include a timeline of events leading up to the current condition.- Record any treatments or medications the patient has already tried.1.3 Review of Systems:- Systematically document the patient's symptoms and complaints related to each body system.- Include information on constitutional symptoms, such as fever, weight loss, or fatigue.- Record any positive or negative findings in each system, such as respiratory, cardiovascular, gastrointestinal, etc.- Mention any relevant family history that may impact the patient's condition.2. Objective:2.1 Physical Examination:- Document the findings of a thorough physical examination, including vital signs, general appearance, and specific organ system assessments.- Describe any abnormalities or notable observations.- Include results of laboratory tests, imaging studies, or other diagnostic procedures.- Record the patient's height, weight, and body mass index (BMI).2.2 Assessment:- Summarize the healthcare provider's assessment of the patient's condition.- Include a differential diagnosis, listing possible conditions based on the subjective and objective findings.- Discuss any further diagnostic tests required to confirm or rule out specific conditions.- Mention any consultations or referrals to other specialists.2.3 Diagnostic Impressions:- Provide a concise summary of the confirmed diagnosis or a list of potential diagnoses.- Include the rationale behind the diagnosis, considering the patient's symptoms, physical examination, and test results.- Discuss any complications or comorbidities related to the diagnosis.- Mention any chronic conditions that may impact the patient's current illness.3. Plan:3.1 Treatment Plan:- Outline the proposed treatment options, including medications, therapies, or procedures.- Specify the dosage, frequency, and duration of medications.- Discuss potential side effects or contraindications of the chosen treatment.- Mention any lifestyle modifications or patient education required.3.2 Follow-up:- Schedule any necessary follow-up appointments or tests.- Specify the expected timeline for improvement or resolution of symptoms.- Discuss any potential red flags or warning signs that require immediate medical attention.- Mention any referrals to other healthcare providers or specialists.3.3 Patient Education:- Provide information to the patient regarding their condition, treatment options, and expected outcomes.- Discuss any lifestyle modifications or self-care measures the patient should undertake.- Address any concerns or questions the patient may have.- Offer resources or references for additional information.Conclusion:In conclusion, SOAP English medical records provide a structured and comprehensive approach to documenting patient information. The subjective section captures the patient's background, present illness, and review of systems. The objective section includes physical examination findings and diagnostic impressions. The plan section outlines the treatment plan, follow-up, and patient education. By following this organized format, healthcare providers can ensure accurate and consistent documentation of patient care.。
英文病历报告作文模板
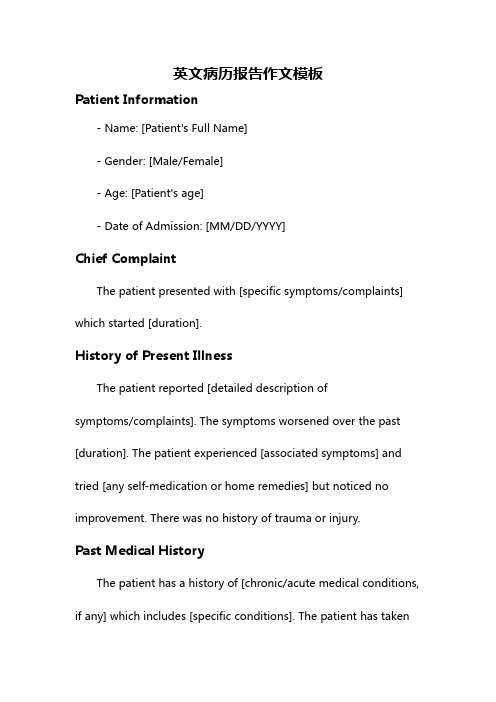
英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。
英文完全病历模板-详细版
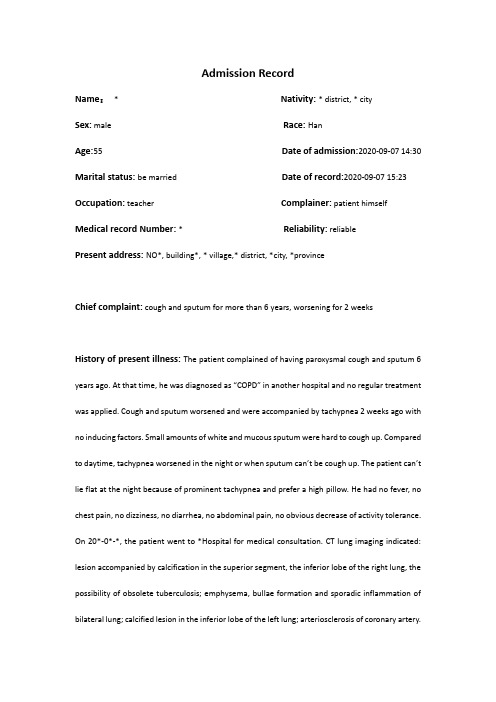
Admission RecordName:* Nativity: * district, * citySex:male Race: HanAge:55 Date of admission:2020-09-07 14:30 Marital status: be married Date of record:2020-09-07 15:23 Occupation:teacher Complainer:patient himself Medical record Number: * Reliability: reliablePresent address: NO*, building*, * village,* district, *city, *provinceChief complaint: cough and sputum for more than 6 years, worsening for 2 weeksHistory of present illness: The patient complained of having paroxysmal cough and sputum 6 years ago. At that time, he was diagnosed as “COPD” in another hospital and no regular treatment was applied. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago with no inducing factors. Small amounts of white and mucous sputum were hard to cough up. Compared to daytime, tachypnea worsened in the night or when sputum can’t be cough up. The patient can’t lie flat at the night because of prominent tachypnea and prefer a high pillow. He had no fever, no chest pain, no dizziness, no diarrhea, no abdominal pain, no obvious decrease of activity tolerance. On 20*-0*-*, the patient went to *Hospital for medical consultation. CT lung imaging indicated: lesion accompanied by calcification in the superior segment, the inferior lobe of the right lung, the possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in the inferior lobe of the left lung; arteriosclerosis of coronary artery.Pulmonary function tests indicated:d obstructive ventilation dysfunction; bronchial dilation test was negative2.moderate decrease of diffusion function, lung volume, residual volume and the ratio of lungvolume; residual volume were normalThe patient was diagnosed as “AECOPD” and prescribed cefoxitin to anti-infection for a week, Budesonide and Formoterol to relieve bronchial muscular spasm and asthma,amb roxol to dilute sputum, and traditional Chinese medicine (specific doses were unknown).The patient was discharged from the hospital after symptoms of cough and sputum slightly relieved with a prescription of using Moxifloxacin outside the hospital for 1 week. Cough and sputum were still existing, thus the patient came to our hospital for further treatment and the outpatient department admitted him in the hospital with “COPD”. His mental status, appetite, sleep, voiding, and stool were normal. No obvious decrease or increase of weight.Past history: The patient was diagnosed as type 2 diabetes 1 years ago and take Saxagliptin (5mg po qd) without regularly monitoring the levels of blood sugar. The patient denies hepatitis, tuberculosis, malaria, hypertension, mental illness, and cardiovascular diseases. Denies surgical procedures, trauma, transfusion, food allergy and drug allergy. The history of preventive inoculation is not quite clear.Personal history: The patient was born in *district, * city and have lived in * since birth. He denies water contact in the schistosome epidemic area. Smoking 10 cigarettes a day for 20 years and have stopped for half a month. Denies excessive drinking and contact with toxics.Marital history: Married at age of 27 and have two daughters. Both the mate and daughters are healthy.Family history: Denies familial hereditary diseases.Physical ExaminationT: 36.5℃ P:77bpm R: 21 breaths/min BP:148/85mmHgGeneral condition:normally developed, well-nourished, normal facies, alert, active position, cooperation is goodSkin and mucosa: no jaundiceSuperficial lymph nodes: no enlargementHead organs: normal shape of headEyes:no edema of eyelids; no exophthalmos; eyeballs move freely; no bleeding spots of conjunctiva; no sclera jaundice; cornea clear; pupils round, symmetrical in size and acutely reactive to light.Ears: no deformity of auricle; no purulent secretion of the external canals; no tenderness over mastoidsNose: normal shape; good ventilation;no nasal ale flap; no tenderness over nasal sinus; Mouth: no cyanosis of lips; no bleeding spots of mouth mucosa; no tremor of tongue; glossy tongue in midline; no pharynx hyperemia; no enlarged tonsils seen and no suppurative excretions; Neck: supple without rigidity, symmetrical; no cervical venous distension; Hepatojugular reflux is negative; no vascular murmur; trachea in midline; no enlargement of thyroid glandChest: symmetrical; no deformity of thoraxLung:Inspection:equal breathing movement on two sidesPalpation: no difference of vocal fremitus over two sides;Percussion: resonance over both lungs;Auscultation: decreased breath sounds over both lungs; no dry or moist rales audible; no pleural friction rubsHeart:Inspection: no pericardial protuberance; Apex beat seen 0.5cm within left mid-clavicular at fifth intercostal space;Palpation: no thrill felt;Percussion: normal dullness of heart bordersAuscultation: heart rate 78bpm; rhythm regular; normal intensity of heart sounds; no murmurs or pericardial friction sound audiblePeripheral vascular sign: no water-hammer pulse; no pistol shot sound; no Duroziez’s murmur; no capillary pulsation sign; no visible pulsation of carotid arteryAbdomen:Inspection: no dilated veins; no abnormal intestinal and peristaltic waves seenPalpation: no tenderness or rebounding tenderness; abdominal wall flat and soft; liver and spleen not palpable; Murphy's sign is negativePercussion: no shifting dullness; no percussion tenderness over the liver and kidney regionAuscultation: normal bowel sounds.External genitalia: uncheckedSpine: normal spinal curvature without deformities; normal movementsExtremities: no clubbed fingers(toes); no redness and swelling of joints; no edema over both legs; no pigmentation of skins of legsNeurological system: normal muscle tone and myodynamia; normal abdominal and bicipital muscular reflex; normal patellar and heel-tap reflex; Babinski sign(-);Kerning sign(-) ; Brudzinski sign(-)Laboratory DataKey Laboratory results including CT imaging and pulmonary function test have been detailed in the part of history of present illness.Abstract*, male, 55 years old. Admitted to our hospital with the chief complaint of cough and sputum for more than 6 years, worsening for 2 weeks. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago. The patient can’t lie flat in the night because of prominent tachypnea and prefer a high pillow.Physical Examination: T: 36.5℃,P: 77bpm, R: 21 breaths per minute, BP:148/85mmHg. Decreased breath sounds over both lungs; no dry or moist rales audible.Laboratory data: CT lung imaging indicates: lesion accompanied by calcification in superior segment, inferior lobe of right lung, possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in inferior lobe of left lung. Pulmonary function tests indicate: mild obstructive ventilation dysfunction, bronchial dilation test was negative moderate decrease of diffusion function.Primary Diagnosis:1.AECOPD2.Type 2 Diabetes3.Primary Hypertension Doctor’s Signature:。
医学英语阅读:英文病历
医学英语阅读:英文病历导读:本文医学英语阅读:英文病历,仅供参考,如果觉得很不错,欢迎点评和分享。
a sample of complete historypatient's name: mary swanchart number: 660518date of birth:10-5-1993sex: femaledate of admission: 10-12-2000date of discharge: 10-15-2000final discharge summarychief complaint:coughing, wheezing with difficult respirations.present illness:this is the first john hopkins hospital admission for this seven-year-old female with a history of asthma since the age of 3 who had never been hospitalized for asthma before and had been perfectly well until three days prior to admission when the patient development shortness of breath and was unresponsive to tedral or cough medicine.the wheezing progressed and the child was taken to john hopkins hospital emergency room where the child was given epinephrine and oxygen. she was sent home. the patient was brought back to the er three hours later was admitted.pasthistory:the child was a product of an 8.5-month gestation. the mother had toxemia of pregnancy. immunizations: all. feeding: good. allergies: chocolate, dog hair, tomatoes.family history:the mother is 37, alive and well. the father is 45, alive and well. two sibs, one brother and one sister, alive and well. the family was not positive for asthma, diabetes, etc.review of systems:negative except for occasional conjunctivitis and asthma.physical examination on admission:the physical examination revealed a well-developed and well-nourished female, age 7, with a pulse of 96, respiratory rate of 42 and temperature of 101.0℉. she was in a mist tent at the time of examination.funduscopic examination revealed normal fundi with flat discs. nose and throat were somewhat injected, particularly the posterior pharynx. the carotids were palpable and equal. ears were clear. thyroid not palpable. the examination of the chest revealed bilateral inspiratory and expiratory wheezes. breath sounds were decreased in the left anterior lung field. the heart was normal. abdomen was soft and symmetrical, no palpable liver, kidney, or spleen. the bowel sounds were normal. pelvic: normal female child. rectal deferred. extremities negative.impression:bronchial asthma, and pharyngitis.laboratory data:the white count on admission was 13,600 with hgb of 13.0. differential revealed 64 segs and 35 lymphs with 3 eos. adequate platelets. sputum culture and sensitivity revealed alpha hemolytic streptococcus sensitive to penicillin. chest x-ray on admission showed hyperaeration and prominent bronchovascular markings. the child was started on procaine penicillin 600,000 unites im q.d in accordance with the culture and sensitivity of the sputum.hospital course:。
护理病历英文
护理病历英文全文共四篇示例,供读者参考第一篇示例:Nursing notes typically include a variety of information, such as vital signs, medications administered, procedures performed, and observations of the patient's physical and mental status. They also document any changes in the patient's condition, response to treatment, and any concerns or issues that arise during the course of care.第二篇示例:Nursing Care RecordA nursing care record, also known as a nursing documentation or a patient care record, is an important document that records the care provided to a patient by a nurse. It serves as a legal document, communication tool between healthcare professionals, and a vital source of information for future care planning.The nursing care record typically includes the following components:第三篇示例:The nursing care record is a legal document that serves as a communication tool between healthcare professionals involved in the patient's care. It helps to ensure continuity of care and provide a clear picture of the patient's progress and response to treatment. In addition, it also serves as a quality assurance tool to evaluate the effectiveness of nursing interventions and to identify areas for improvement in patient care.The nursing care record typically includes the following information:4. Physical assessment: This includes the patient's vital signs, general appearance, level of consciousness, and any physical findings relevant to the patient's condition.第四篇示例:Nursing Progress NotesPatient Name: John DoeAge: 45Date of Admission: September 15th, 2021Vital Signs:- Blood pressure: 140/90 mmHg- Heart rate: 110 beats per minute- Respiratory rate: 20 breaths per minute- Temperature: 98.6°FNursing Care Plan:- Monitor patient's cardiac status closely, including vital signs, EKG changes, and symptoms- Administer medications as ordered, including nitroglycerin and aspirin- Provide emotional support and education to the patient and family members about the importance of medication compliance and lifestyle modifications- Encourage the patient to participate in cardiac rehabilitation programs and follow-up appointments with the cardiologistOverall, John Doe is responding well to treatment and is stable at this time. Close monitoring and follow-up care will be essential to ensuring the patient's continued recovery andwell-being.。
英语大病历模板
英文大病例写作示例时间:2007-06-04 17:19来源:中国医师协会作者: 点击: 355 次 ?撰写大病例是实习医师与住院医师的日常工作,也是上级医师作进一步诊断治疗的原始依据,国外的英文大病例并无统一格式,但是基本内容大致相仿,本节介绍的许多医疗记录的词汇值得借鉴。
Details个人资料Name: Joe Bloggs(姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
)Associated symptoms相关症状Nausea, vomiting×2, sweating, dizzy(恶心、呕吐2次、出汗、眩晕)1997:external chest tightness and dyspnea initially controlled atenolol.1997年:出现胸外疼痛与呼吸困难,最终经服atenolol控制。
英文病历书写

过饱的人 a heavy (great; hard) eater
食量 capacity for eating
ex1:他的食欲良好,但他平常的吃食习惯,由于口里伤处而中断。
His appetite was good, but the sore place in his mouth interrupted his usual eating habit.
没有发烧 be afebrile; have no fever
ex1:在发烧期间,他的平均体温是摄氏39度。
He ran a febrile course with an average temperature of 39°C.
ex2:他在患病期间尿量减少,并且发烧。
发烧
发烧 become feverish; have a temperature
发高烧 have a high fever
平常有微热,有几次升到38.4度 have low grade (slight) fever to 38.4°C on a few occasions
(2)他诉说非常口渴,但一点食欲也没有。
He complains of his thirst hard to release, while he has absolutely no appetite.
口渴
口渴 be (feel) thirsty form
ex2:他的胃口变得很大,食物热量增加2倍,但体重却减轻了10公斤。
His appetite became ravenous and his caloric intake doubled, yet he lost 10 kg.
英文病历书写——睡眠
- 1、下载文档前请自行甄别文档内容的完整性,平台不提供额外的编辑、内容补充、找答案等附加服务。
- 2、"仅部分预览"的文档,不可在线预览部分如存在完整性等问题,可反馈申请退款(可完整预览的文档不适用该条件!)。
- 3、如文档侵犯您的权益,请联系客服反馈,我们会尽快为您处理(人工客服工作时间:9:00-18:30)。
Name: ______________ Sex: __________ Age: ___________ Nation:___________Birth Place: ________________________________ MaritalStatus:____________Work-organization & Occupation:_______________________________________Living Address & Tel:_________________________________________________Date of admission: _______Date of history taken:_______Informant:__________Chief Complaint:___________________________________________________History of Present Illness:__________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ ________________________________________________________________________Past History:General Health Status: 1.good 2.moderate 3.poorDisease history:(if any, please write down the date of onset, briefdiagnostic and therapeutic course, and theresults.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest pain_______________________________________________________________ Circulatory system:1.None2.Palpitation3.exertional dyspnea4..cyanosis5.hemoptysis6.Edema of lower extremities7.chest pain8.syncope9.hypertension_______________________________________________________________Digestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea 11.hematemesis12.Hematochezia 13.jaundice_______________________________________________________________Urinary system:1.None2.Lumbar pain3.urinary frequency4.urinary urgency5.dysuria6.oliguria7.polyuria8.retention of urine9.incontinence of urine 10.hematuria 11.Pyuria12.nocturia 13.puffy face_______________________________________________________________Hematopoietic system:1.None2.Fatigue3.dizziness4.gingival hemorrhage5.epistaxis6.subcutaneous hemorrhage_______________________________________________________________Metabolic and endocrine system:1.None2.Bulimia3.anorexia4.hot intolerance5.coldintolerance6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character change 11.Markedobesity 12.marked emaciation 13.hirsutism14.alopecia15.Hyperpigmentation 16.sexual function change_______________________________________________________________Neurological system:1.None2.Dizziness3.headache4.paresthesia5.hypomnesis6. Visual disturbance7.Insomnia8.somnolence9.syncope 10.convulsion 11.Disturbance ofconsciousness 12.paralysis 13. vertigo_______________________________________________________________Reproductive system:1.None2.others_______________________________________________________________Musculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophy_______________________________________________________________Infectious Disease:1.None2.Typhoid fever3.Dysentery4.Malaria4.Schistosomiasis 4.Leptospirosis 7.Tuberculosis8.Epidemic hemorrhagic fever 9.others_______________________________________________________________Vaccine inoculation:1.None2.Yes3.Not clearVaccine detail__________________________________________Trauma and/or operation history:Operations:1.None2.YesOperationdetails:_______________________________________Traumas:1.None2.YesTraumadetails:_________________________________________Blood transfusion history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredienttransfusion)Blood type:____________ Transfusion time:___________Transfusion reaction1.None2.YesClinicmanifestation:_____________________________Allergic history:1.None2.Yes3.Not clearallergen:______________________________________________ __clinicalmanifestation:_____________________________________Personal history:Custom livingaddress:____________________________________________Resident history in endemic diseasearea:_____________________________Smoking: 1.No 2.YesAverage ___pieces per day; about___yearsGiving-up 1.No 2.Yes(Time:_______________________)Drinking: 1.No 2.YesAverage ___grams per day; about ___yearsGiving-up 1.No2.Yes(Time:________________________)Drug abuse:1.No 2.YesDrug names:_______________________________________ _______________________________________________________________Marital and obstetrical history:Married age: __________years old Pregnancy ___________times Labor _______________times(1.Natural labor: _______times 2.Operative labor:________times3.Natural abortion: ______times4.Artificial abortion:_______times5.Premature labor:__________times6.stillbirth__________times)Health status of the Mate:1.Well2.Not fineDetails:_______________________________________________Menstrual history:Menarchal age:_______ Duration ______day Interval____days Last menstrual period: ____________ Menopausal age: ____years oldAmount of flow: 1.small 2. moderate 3. largeDysmenorrheal: 1. presence 2.absence Menstrual irregularity 1. No2.YesFamily history: (especially pay attention to the infectious andhereditary disease related to the present illness) Father: 1.healthy 2.ill:________ 3.deceased cause:___________________Mother:1.healthy 2.ill:________ 3.deceased cause:___________________Others: ________________________________________________________The anterior statement was agreed by the informant.Signature of informant: Datetime:Physical ExaminationVital signs:Temperature:______0C Blood pressure:_______/_______mmHg Pulse: _____ bpm (1.regular2.irregular_____________________________)Respiration: ___bpm (1.regular2.irregular____________________________)General conditions:Development: 1.Normal 2.Hypoplasia 3.HyperplasiaNutrition: 1.good 2.moderate 3.poor 4.cachexiaFacial expression: 1.normal 2.acute 3.chronicother_____________________Habitus: 1.asthenic type 2.sthenic type 3.ortho-thenic typePosition: 1.active 2.positive pulsive4.other_______________________Consciousness: 1.clear 2.somnolence 3.confusion 4.stupor5.slight coma6.mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: 1.normal 2.abnormal______Skin and mucosa:Color:1.normal 2.pale 3.redness 4.cyanosis 5.jaundice 6.pigmentation Skin eruption:1.No 2.Yes( type:__________distribution:__________________)Subcutaneous bleeding: 1.no 2.yes(type:_______distribution:______________)Edema:1. no 2.yes ( location anddegree________________________________)Hair: 1.normal2.abnormal(details_____________________________________)Temperature and moisture: normal cold warm dry moist dehydrationLiver palmar : 1.no 2.yes Spider angioma(location:________________)Others: __________________________________________________________ Lymph nodes: enlargement of superficial lymph node:1.no2.yesDescription:________________________________________________Head:Skull size:1.normal 2.abnormal(description:____________________________)Skull shape:1.normal2.abnormal(description:___________________________)Hair distribution :1.normal2.abnormal(description:______________________)Others:__________________________________________________________ _Eye:exophthalmos:___________eyelid:____________conjunctiva:__________ sclera:________________Cornea:_______________________ Pupil: 1.equally round and in size 2.unequal (R______mmL_______mm)Pupil reflex: 1.normal 2.delayed (R___s L___s ) 3.absent (R___L___)others:______________________________________________________Ear: Auricle 1.normal 2.desformation(description:_______________________)Discharge of external auditory canal:1.no 2.yes (1.left 2.right quality:_____)Mastoid tenderness 1.no 2.yes (1.left 2.rightquality:__________________) Disturbance of auditoryacuity:1.no 2.yes(1.left 2.right description:_______) Nose: Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no2.yes(quality______)Tenderness over paranasal sinuses:1.no 2.yes(location:_______________)Mouth: Lip______________Mucosa_____________Tongue________________ Teeth:1.normal 2. Agomphiasis 3. Eurodontia4.others:____________________Gum :1.normal 2.abnormal(Description____________________________)Tonsil:___________________________Pharynx:_____________________Sound: 1.normal 2.hoarseness3.others:_____________________________Neck:Neck rigidity 1.no 2.yes (______________transvers fingers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distentionTrachea location: 1.middle 2.deviation(1.leftward_______2.rightward______)Hepatojugular vein reflux: 1. negative 2.positiveThyroid: 1.normal 2.enlarged _______ 3.bruit (1.no 2.yes________________)Chest:Chest wall: 1.normal 2.barrel chest 3.prominence or retraction: ( left________right_________Precordialprominence__________)Percussion pain over sternum 1.No 2.YesBreast: 1.Normal 2.abnormal_______________________________________Lung:Inspection: respiratory movement 1.normal2.abnormal_____________Palpation: vocal tactile fremitus:1.normal 2.abnormal_______________ pleural rubbing sensation:1.no2.yes______________________Subcutaneous crepitus sensation:1.no2.yes________________Percussion:1. resonance 2. Hyperresonance&location_____________ 3Flatness&location_________________________________4. dullness &location:_______________________________5.tympany&location:_______________________________lower border of lung: (detailed percussion inrespiratory disease)midclavicular line : R:_____intercostaeL:_____intercostaemidaxillary line: R:______intercostaeL:_____intercostaescapular line: R:______intercostaeL:_____intercostaemovement of lower borders:R:_______cmL:__________cm Auscultation: Breathing sound : 1.normal 2.abnormal_______________Rales:1.no2.yes__________________________________Heart: Inspection:Apical pulsation: 1.normal 2.unseen 3.increase4.diffuse Subxiphoid pulsation: 1.no 2.yesLocation of apex beat: 1.normal 2.shift (______intercosta,distance away from leftMCL______cm)Palpation:Apical pulsation:1. normal 2.lifting apex impulse3.negative pulsationThrill:1.no 2.yes(location:___________phase:_________________)Percussion: relative dullness border: 1.normal 2.abnormal_______cm)Auscultation: Heart rate:___bpm Rhythm:1.regular2.irregular_______Heart sound: 1.normal2.abnormal________________________Extra sound: 1.no 2.S3 3.S44. opening snapP2_________ A2_________Pericardial friction sound:1.no2.yesMurmur: 1.no 2.yes(location____________phase_____________quality______intensity________transmission___________effects ofposition_________________________________effects ofrespiration______________________________Peripheral vascular signs:1.None2.paradoxical pulse3.pulsus alternans4. Waterhammer pulse 5.capillary pulsation 6.pulsedeficit 7.Pistol shot sound 8.Duroziez sign Abdomen:Inspection: Shape: 1.normal 2.protuberance 3.scaphoid4.frog-bellyGastric pattern 1.no 2.yes Intestinal pattern1.no2.yesAbdominal vein varicosis 1.no2.yes(direction:______________ )Operation scar1.no 2.yes________________________________Palpation: 1.soft 2. tensive(location:____________________________)Tenderness: 1.no2.yes(location:_______________________)Rebound tenderness:1.no2.yes(location:________________)Fluctuation: 1.present 2.abscentSuccussion splash: 1.negative 2.positiveLiver:_______________________________________________Gallbladder: __________________Murphysign:____________Spleen:______________________________________________Kidneys:____________________________________________Abdominalmass:______________________________________Others:______________________________________________Percussion: Liver dullness border: 1.normal 2.decreased3.absentUpper hepatic border:Right Midclavicular Line________IntercostaShift dullness:1.negative 2.positiveAscites:_____________degreePain on percussion in costovertebral area: 1.negative 2.positve ____Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis3.hypoperistalsis4.absenceGurgling sound:1.no 2.yes Vascular bruit 1.no 2.yes(location_____________________)Genital organ: 1.unexamined 2.normal 3.abnormalAnus and rectum: 1.unexamined 2.normal 3.abnormalSpine and extremities:Spine: 1.normal 2.deformity (1.kyphosis 2.lordosis3.scoliosis)3.Tenderness(location______________________________)Extremities: 1.normal 2.arthremia & arthrocele(location_________________) 3.Ankylosis(location__________) 4.Aropachy: 1.no 2.yes5.Muscular atrophy(location_______________________)Neurological system:1.normal2.abnormal____________________________________________________________________________________________________ Important examination results before hospitalized__________________________________________________________ ____________________________________________________________ ___________________________________________________________ ___________________________________________________________ _Summary of thehistory:________________________________________________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ____________________________________________________________ _Initialdiagnosis:_____________________________________________ __________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ _Recorder:Corrector:欢迎您的下载,资料仅供参考!致力为企业和个人提供合同协议,策划案计划书,学习资料等等打造全网一站式需求。
